Research Article
Exploring the Prevalence and Causes of Normal Tc-99m Thyroid Uptake in Thyrotoxic Patients: A Retrospective Study at a Regional Hospital of Nuclear Medicine in Oman
Department of Nuclear Medicine and Molecular Imaging Center, Royal Hospital, Oman.
*Corresponding Author: Khalsa Al-Nabhani, Department of Nuclear Medicine and Molecular Imaging Center, Royal Hospital, Oman.
Citation: Al-Sawafi F, Al-Nabhani K. (2023). Exploring the Prevalence and Causes of Normal Tc-99m Thyroid Uptake in Thyrotoxic Patients: A Retrospective Study at a Regional Hospital of Nuclear Medicine in Oman, Journal of Endocrinology and Diabetes Research, BRS Publishers. 1(1); DOI: 10.59657/2996-3095.brs.23.002
Copyright: © 2023 Fatema Al-Sawafi, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: April 27, 2023 | Accepted: May 15, 2023 | Published: May 23, 2023
Abstract
This study focuses on assessing the prevalence of normal Technetium-99m (Tc-99m) Thyroid uptake scans among thyrotoxic patients at a specific medical facility in Oman, named "Royal hospital-nuclear medicine department". Thyrotoxicosis is a condition characterized by high levels of thyroid hormones in the body which is usually reflects as a high uptake in Tc-99m Thyroid Pertechnetate uptake scan. However, in some cases the scan shows normal thyroid activity which may lead to misdiagnosis or delayed treatment.
Aim: To determine the prevalence, or the percentage of thyrotoxic patients at the facility who have normal Tc-99m thyroid uptake. This information could help to improve the understanding of the underlying causes of thyrotoxicosis and inform treatment decisions for affected patients.
Methodology: It is a retrospective study that was conducted at the Royal Hospital during the period between February and May 2022 with a total number of 102 patients included.
Results: It has revealed a significant percentage of thyrotoxic patients with normal Tc-99m thyroid uptake levels, out of 102 patients, 38 patients (37.25%).
Conclusion: The importance of considering normal Tc-99m thyroid uptake as a potential finding in thyrotoxic patients undergoing thyroid scintigraphy has been highlighted and the possible underlying causes have been identified. Such knowledge is expected to improve the accuracy of Thyroid uptake scan’s reporting and reduce the likelihood of misdiagnosis or delayed treatment.
Keywords: thyrotoxicosis, tc-99m thyroid uptake scan, hyperthyroidism
Introduction
Thyroid disorders are prevalent globally and affect people of all ages. Thyrotoxicosis, also known as hyperthyroidism, is a common endocrine disorder characterized by increased secretion of thyroid hormones resulting in elevated basal metabolic rate, weight loss, tachycardia, and sweating [1]. It is usually diagnosed by clinical examination, laboratory tests, and imaging studies, including Technetium-99m (Tc-99m) pertechnetate thyroid scan [2]. Tc-99m pertechnetate is a radioactive tracer that is taken up by the thyroid gland and visualized using nuclear medicine imaging [3]. The most common causes of thyrotoxicosis are as follow; Graves' disease, toxic multinodular goiter, toxic adenoma, subacute thyroiditis and less commonly exogenous thyrotoxic medication and exposure to iodine-rich substances [4].
Tc-99m thyroid uptake scan is a widely used imaging test for the diagnosis and evaluation of thyroid diseases. However, normal Tc-99m thyroid uptake has been observed in some thyrotoxic patients, which may lead to misdiagnosis or delayed treatment. The prevalence and causes of normal Tc-99m thyroid uptake in thyrotoxic patients have not been well studied. The objective of this study is to determine the prevalence of normal Tc-99m thyroid uptake among thyrotoxic patients at one of the biggest tertiary hospitals in Oman, the Royal hospital. The aim of this study is to increase the awareness of normal Tc-99m thyroid uptake among thyrotoxic patients and trace the underlying causes of normal uptake in clinically and biomedically toxic patients, which could lead to improved diagnostic accuracy and enhance patient management.
Materials and Methods
This is a retrospective study of medical records of patients who underwent Tc-99m pertechnetate thyroid scan at nuclear medicine department, Royal hospital in Oman, between February 1st, 2022, and May 31, 2022. A total of 102 patients with thyrotoxic symptoms and diagnosis of thyrotoxicosis confirmed by laboratory tests and clinical examination were included in the study. Tc-99m pertechnetate thyroid uptake scan procedure is a diagnostic procedure used to evaluate thyroid gland and detect any functional abnormalities. Thyroid Uptake Procedure’s Protocol: As preparation for the test, the patients are instructed to discontinue certain medications that can interfere with thyroid function, usually their antithyroid medications. The interruption of medication is variable based on the type of medication as follow; carbimazole is stopped for 3-5 days and Propylthiouracil (PTU) for 5-7 days.
Patients were asked to fill out a pre-procedure's questionnaire prior to undergoing the thyroid uptake scan. The questionnaire was designed to gather information about the patient's age, gender, and any medical conditions they have been diagnosed with. It also included enquiries about their medications which might affect the study results, especially thyroid hormone replacement therapy or antithyroid medications. In addition, patients were requested into describe any symptoms related to thyroid gland malfunction, such as fatigue, weight changes, or heart rate abnormalities. Previous thyroid-related procedures, recent enhanced CT scan or surgeries were highlighted too. The questionnaire was typically completed in the waiting area before the scan, under the supervision of a member of the study team.
The information gathered from the pre-procedure questionnaire was used in the analysis of the study results, for example, by collecting information about the patient's medical history and medications, the study team was able to identify potential factors that could affect thyroid function and therefore, its radiotracer uptake. This information was then used in conjunction with the results of the thyroid uptake scan to help identify potential thyroid abnormalities and evaluate underlying causes in the studied participants. Tc -99m pertechnetate thyroid uptake scan was performed by trained nuclear medicine technologists under the supervision of a nuclear medicine physician, following the departmental standard operating procedure, which is typically a painless procedure that takes about 30-60 minutes to be completed. A thyroid uptake was considered normal when the radiotracer activity ranged between 0.4-4% which is the local normal range for thyroid uptake in the Royal hospital.
The data collected has included patient demographics, laboratory results, findings from thyroid ultrasound, global thyroid uptake results, scintigraphic findings and diagnosis, anti-thyroid medications and the number of days of medication interruption as well as history of COVID-19 infection prior to beginning of thyrotoxic symptoms. Certain patients were excluded from participation in the study based on specific criteria which was designed to ensure that the study results were as accurate and reliable as possible.
Patients who met any of the following criteria were excluded from participation in the study:
- Congenital hypothyroidism: Patients who had been diagnosed with congenital hypothyroidism were excluded from the study.
- Failure to fill out the questionnaire: Patients who did not complete the pre-procedure questionnaire were excluded from the study. This was because the questionnaire was an important component of the methodology used in this research study, and failure to complete it could result in missing important patient’s information.
- Non-toxic multinodular goiter patients were excluded from the study. This was because this condition is typically managed differently than toxic goiter.
Data Analysis
Data collected was analysed using descriptive statistics to determine the frequency and distribution of variables such as age, sex, diagnosis, and medications. The results of blood tests and ultrasound findings were also analysed to identify any patterns or correlations. Ethical considerations: The study was conducted and approved by the local hospital ethical institutional review board. No verbal or written consent was obtained from the patients as it is a retrospective study, however, their personal and medical information was kept confidential.
Results
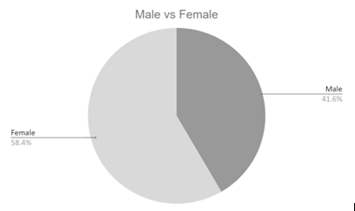
A total of 102 thyrotoxic patients were included in the study, of which 38 (37.25%) had normal Tc-99m thyroid uptake. The mean age of the patients was 41.5 years, and 58.4% were female (Figure 1&2). The most common diagnosis based on Tc-99m thyroid uptake scan findings was Graves' disease (40.19%), followed by heterogenous normal uptake (37.25%) and thyroiditis (10.78%) (Figure-3).
Figure 1: Sex-graph, showed 58.4
Discussion
The current study aimed to investigate the prevalence and causes of normal Tc-99m thyroid uptake among thyrotoxic patients. Our findings revealed that 37.25% of the thyrotoxic patients had a normal thyroid uptake, which is consistent with previous studies [5&7]. There are limited studies directly reporting the prevalence of normal Tc-99m pertechnetate thyroid uptake in thyrotoxic patients. However, a few studies and reviews have mentioned the possibility of observing normal thyroid uptake in certain cases of thyrotoxicosis. In a study by Al-Muqbel et al, researchers evaluated 155 thyrotoxic patients who underwent Tc-99m thyroid uptake scan. They found that 49 of these patients had normal thyroid uptake. The overall prevalence of normal thyroid uptake in their population was 31% [5]. In addition, Sucupira et al. has evaluated a population of 18 patients with hyperthyroidism where (total 18 patients) and four of them reported a pooled prevalence of normal Tc-99m thyroid uptake of (22%) [6].
Another study by Ikekubo et al., has evaluated 201 of untreated thyrotoxic patients who underwent Tc-99m thyroid pertechnetate scan. Of these, 24 patients (11.9%) had normal thyroid uptake which is the lowest rate reported compared to our study and to Al-Muqbel et al. and Sucupira et al. The researchers in this study, have found that the patients with normal uptake were more likely to have early stage of Graves' disease which is a possibility that has not described in previous studies [7]. These studies suggest that a significant proportion of thyrotoxic patients may have normal thyroid uptake on Tc-99m scintigraphy and the reasons behind this phenomenon could be multifactorial. It can be due to recovering subacute thyroiditis, factitious thyrotoxicosis (8), transient thyrotoxicosis or early Graves’ disease [7]. Moreover, the use of iodinated contrast agents, amiodarone, and lithium can also lead to normal thyroid uptake [9,10].
Interestingly, in our study the most common cause of normal thyroid uptake among thyrotoxic patients was multiple cold nodules (eight patients) which can reduce the thyroid uptake by occupying a significant portion of the gland and decreasing the overall function of the thyroid gland. Additionally, recovering thyroiditis and COVID-19 associated thyroiditis was another common cause of normal thyroid uptake, which agree with previous studies’ results. In contrast, factitious thyrotoxicosis was not a common cause of normal thyroid uptake in our study. This finding is inconsistent with some previous reports which suggested factitious thyrotoxicosis as a possible reason for normal thyroid uptake in some patients. However, our study had a limited sample size, which might have affected the results. Regarding COVID-associated thyroiditis, is a newly recognized phenomenon that warrants further investigation and careful long-term follow-up Lania et al. has shown in their study that COVID-19 can affect the thyroid gland, leading to thyroid dysfunction and inflammation in some patients. A study of hospitalized COVID-19 patients found that significant number of them had thyrotoxicosis due to a form of subacute thyroiditis related to SARS-CoV-2 (Muller et al., 2020). Another study by Brancatella et al. has described 4 patients with subacute thyroiditis related to SARS-CoV-2 infection. [11,12 &13].
Overall, the findings of this study analysis suggested that COVID-associated thyroiditis may be a potential complication of COVID-19 infection and patients who report thyroid symptoms after COVID-19 infection should be evaluated and monitored for thyroid dysfunction or autoimmune thyroid disease. Our study had some limitations, including the limited sample size. Furthermore, the study population was limited to a single center, which might limit the generalizability of our findings. Larger multicenter studies are needed to confirm our results and further assess the effect of normal thyroid uptake on the thyrotoxic patients' management.
Conclusion
The results of this study will provide valuable information on the prevalence and causes of normal Tc-99m thyroid uptake among thyrotoxic patients in Oman, which will contribute to the body of knowledge on thyroid disorders and help improve the diagnostic accuracy of thyroid uptake scan and patient management. Our study indicates that normal Tc-99m thyroid uptake is prevalent among thyrotoxic patients, and its causes are diverse. Therefore, Nuclear medicine physicians should consider the possibility of underlying colds nodules, thyroiditis, and other causes of normal thyroid uptake when interpreting thyroid uptake scans in thyrotoxic patients. Further studies with larger sample sizes are needed to investigate the impact of normal thyroid uptake on the management and prognosis of thyrotoxic patients.
Disclosure: No potential conflict of interest relevant to this article was reported.
References
- Kannan CR, Seshadri KG. (1997). Thyrotoxicosis. Dis Mon. 43(9):601-677.
Publisher | Google Scholor - Chaudhary V, Bano S. (2012). Imaging of the thyroid: Recent advances. Indian J Endocrinol Metab. 16(3):371-376.
Publisher | Google Scholor - Kane SM, Davis DD. (2023). Technetium-99m. In: StatPearls Publishing.
Publisher | Google Scholor - De Leo S, Lee SY, Braverman LE. (2016). Hyperthyroidism. Lancet. 388(10047):906-918.
Publisher | Google Scholor - Al-Muqbel KM. (2022). Utility of 99m Technetium Pertechnetate Thyroid Scan and Uptake in Thyrotoxic Patients: Jordanian Experience. World J Nucl Med. 22(1):7-14.
Publisher | Google Scholor - Sucupira MS, Camargo EE, Nickoloff EL, Alderson PO, Wagner HN Jr. (1983). The role of 99mTc pertechnetate uptake in the evaluation of thyroid function. Int J Nucl Med Biol, 10(1):29-33.
Publisher | Google Scholor - Ikekubo K, Hino M, Ito H, Koh T, Ishihara T, Kurahachi H, Kasagi K, Hidaka A, Mori T. (1990). Thyrotoxic Graves' disease with normal thyroidal technetium-99m pertechnetate uptake. Ann Nucl Med. 4(2):43-48.
Publisher | Google Scholor - Abdel-Nabi H, Falko JM, Olsen J. (1982). The value of technetium Tc 99m pertechnetate thyroid scanning in the diagnosis of factitious thyrotoxicosis. Arch Intern Med. 142(3):644-645.
Publisher | Google Scholor - Narayana SK, Woods DR, Boos CJ. (2011). Management of amiodarone-related thyroid problems. Ther Adv Endocrinol Metab. 2(3):115-126.
Publisher | Google Scholor - Kibirige D, Luzinda K, Ssekitoleko R. (2013). Spectrum of lithium induced thyroid abnormalities: a current perspective. Thyroid Res. 6(1):3.
Publisher | Google Scholor - Lania A, Sandri M. T, Cellini M, Mirani M, Lavezzi E, Mazziotti G, degli Uberti E. C. (2020). Thyrotoxicosis in patients with COVID-19: the THYRCOV study. European Journal of Endocrinology, 183(4):381-387.
Publisher | Google Scholor - Muller I, Cannavaro D, Dazzi D, Covelli D, Mantovani G, Muscatello A, Ferrante E. (2020). SARS-CoV-2-related atypical thyroiditis. The Lancet Diabetes & Endocrinology, 8(9):739-741.
Publisher | Google Scholor - Brancatella A, Ricci D, Cappellani D, Viola N, Sgrò D, Santini F, Latrofa F. (2020). Is subacute thyroiditis an underestimated manifestation of SARS-CoV-2 infection? Insights from a case series. Journal of Clinical Endocrinology and Metabolism, 105(10):537.
Publisher | Google Scholor