Review Article
A Systematic Review on Acute Kidney Injury Following Cardiac Surgery: Clinical Outcomes with Preventive Strategies Over the Decades
- Chandana Sree Madala 1
- Mohammed Quader Naseer 2
- Kanakath Sanvi 3
- Krutika Mahendra Gohil 4
- Sinthujaa Velmurugan 5*
- Alisha Lakhani 6
- Kaarvi Khullar 7
- Richard Paul 3
1Narayana Medical College and Hospital, Nellore, Andhra Pradesh, India
2Ayaan Institute of Medical Sciences, Hyderabad, Telangana, India.
3Al Azhar Medical College and Superspeciality Hospital, Kerala, India.
4HBT Medical College and Dr. Rustom Narsi Cooper Municipal General Hospital, Mumbai, India.
5Mahatma Gandhi Medical College and Research Institute, Puducherry, India.
6Shantabaa Medical College, Amreli, Gujarat, India.
7Government Medical College, Gondia, Maharashtra, India.
*Corresponding Author: Sinthujaa Velmurugan, Mahatma Gandhi Medical College and Research Institute, Puducherry, India.
Citation: Madala C. S., Naseer M. Q., Sanvi K., Gohil K. M., Velmurugan S., et al. (2024). A Systematic Review on Acute Kidney Injury Following Cardiac Surgery: Clinical Outcomes with Preventive Strategies Over the Decades, Journal of Clinical Cardiology and Cardiology Research, BioRes Scientia Publishers. 3(2):1-16, DOI: 10.59657/2837-4673.brs.24.033
Copyright: © 2024 Sinthujaa Velmurugan, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: June 11, 2024 | Accepted: July 05, 2024 | Published: July 12, 2024
Abstract
Introduction: Acute kidney injury (AKI) is a common complication following cardiac surgery, contributing to increased morbidity and mortality. This systematic review aims to comprehensively evaluate the incidence, risk factors, and clinical outcomes associated with AKI post-cardiac surgery.
Methods: A systematic search of electronic databases was conducted to identify relevant studies published. Studies reporting on AKI incidence, risk factors, and clinical outcomes in adult patients undergoing cardiac surgery were included. Data were extracted and synthesized following PRISMA guidelines.
Results: A total of 23 studies were included in the review. AKI was associated with increased short and long-term morbidity and mortality, prolonged hospital stays, and higher healthcare costs. Encouraging outcomes were noted when dexmedetomidine, a highly selective α2-adrenergic receptor agonist, was administered during surgery. Two promising non-pharmacological strategies to reduce CSA-AKI are the use of a revolutionary renal guard (RG) system and the introduction of a KDIGO-based treatment bundle. Teprasiran, a new P2Y12 receptor antagonist, was found to significantly reduce the frequency and severity of AKI. The results of this review further highlight the significance of customized preventative measures and risk stratification.
Conclusion: Acute kidney injury is a significant complication following cardiac surgery, with considerable variability in its incidence and associated risk factors. Implementation of preventive strategies is crucial in mitigating AKI-related morbidity and mortality. Further research is warranted to optimize patient outcomes and healthcare resource utilization in this population.
Keywords: acute kidney injury; dexmedetomidine; cardiac surgery; preventive measure
Introduction
Acute Kidney Injury (AKI) is a prevalent and frequently encountered complication following cardiac surgery, presenting a significant challenge to patient recovery and prognosis owing to its association with amplified morbidity, mortality, and prolonged hospital stays. CSA-AKI is characterized by an abrupt worsening in kidney function following cardiac surgery as demonstrated by a reduction in the glomerular filtration rate. These patients often have risk factors for kidney disease, such as diabetes, hypertension, and hypercholesterolemia. In addition, cardiac surgery is a major surgical procedure which may contribute to an increased risk for AKI. Susantitaphong et al reported that CBP-associated AKI was associated with an 8-fold increase in mortality in a subgroup analysis within a global incidence study of AKI, based on results from 23 studies [1]. A recent meta-analysis reported that irrespective of the diverse criteria used to define AKI, its occurrence following cardiac surgery is consistently correlates with a 2-4 times higher likelihood of early mortality among patients [2]. The RIFLE criteria defined AKI by a 25% reduction in GFR (this was equated with a 50% increase in creatinine level or low urine output [3]. The AKIN definition reserved the urine output criterion of the RIFLE definition, dropped the change in GFR per se, and altered the creatinine definition such that a small increase of 0.3 mg/dL also could diagnose AKI. The AKIN definition also reduced the time over which AKI was to be diagnosed from 7 days to 48 hours [4]. The KDIGO definition united RIFLE and AKIN by allowing the relative change of 50% in creatinine level to be over 7 days, whereas absolute change is restricted to 48 hours [5].
The intricate interplay of multifactorial mechanisms, including reduced cardiac output, ischemia-reperfusion injury, renal vasoconstriction, nephrotoxic results like Cardiopulmonary bypass-induced systemic inflammatory response leading to interstitial inflammation and coagulopathy, and patient specific risk factors, contributes to the development of AKI in this setting [6]. Despite advancements in surgical techniques and perioperative care, the incidence of AKI following cardiac procedures remains substantial, impacting patient outcomes, length of hospital stays, and healthcare costs. Studies have reported the risk factors for AKI, for example, female gender, reduced left ventricular function, the presence of congestive heart failure, diabetes, chronic obstructive pulmonary disease, and elevated preoperative serum creatinine [7]. A meta-analysis of 307 studies involving 1200 patients, reported that plasma NGAL (pNGAL) can be considered to be a sensitive and specific early marker of AKI and can be detected up to 48 h before a diagnostic rise in serum creatinine [8]. Greenwood et al reported that pulse wave velocity, a non-invasive measurement tool to assess arterial stiffness, has been shown to predict kidney disease progression, and cardiovascular and all-cause mortality in patients with chronic kidney disease [9].
CSA-AKI increases the risk of death during admission, which can increase to 50% when there is a need for RRT. In 2017, Legouis D et al. studied a cohort of 4,791 patients and found that the risk of CKD was higher in patients who had experienced CSA-AKI than in the AKI-free population [10]. In the absence of precise biomarkers, it seems that even a mild instance of AKI can lead to a poorer prognosis concerning the likelihood of developing CKD and long-term survival in patients. Therefore, it might be more beneficial to prevent, and detect AKI risks rather than focusing solely on a cure. This becomes especially crucial when taking into account the 2009 NCEPOD, which reported that 30% of cases of AKI were preventable and identified a deficiency of care in 50% of cases [11]. Despite published studies detailing the link of CBP-associated AKI and unfavorable outcomes, there have been few attempts to systematically summarize the prognostic consequences of AKI. This review aims to explore the multifactorial etiology, risk factors, and preventive strategies associated with AKI post-cardiac surgery. Understanding these intricate facets is vital in developing targeted interventions to mitigate the incidence of AKI, ultimately benefitting patient care and reducing the load on healthcare systems.
Methodology
This Comparative study was performed in accordance with published guidelines for systematic review, analysis, and reporting for meta-analysis of Observational studies.
Literature Search Strategy
A comprehensive search was done by the investigators in PubMed, Google Scholar and Scopus using appropriate subject headings and keywords. After an extensive search process, studies from all over the world focusing on Preventive Strategies of AKI and their outcomes were selected. The reference lists of included studies and relevant reviews were manually searched to avoid missing relevant studies. All identified articles were systematically assessed using the inclusion and exclusion criteria. All the selected studies were carefully reviewed once again individually by the team of investigators and then 23 studies matching inclusion criteria were shortlisted for the final comparison. Investigators independently reviewed the retrieved articles and evaluated the quality assessment. All data regarding the articles retrieved were entered into Excel software.
Inclusion and Exclusion Criteria
Various articles related to Acute Kidney Injury following Cardiac Surgery were searched through PubMed, Google Scholar, and Scopus. Studies concentrating on preventive strategies of Acute Kidney Injury (AKI) were shortlisted.
The following articles were excluded from the study: 1) Abstracts 2) Studies in non-English Language Literature 3) Animal studies 4) Studies published before 2000. All other standard studies in English Literature dated from 2000 to 2023 were included. All analyses were based on previously published studies; thus, no ethical approval and patient consent are required. The reviewers performed independent manual screening of all the articles by firstly the titles/abstracts and secondly the full texts. Besides, other relevant literature and references of the included studies were also manually screened.
Data Extraction
Four independent review authors extracted relevant study characteristics and outcomes from the 23 included studies using a standardized and piloted data extraction form. The information collected from each study included: Name of the Study, Author details, Citation, year of Publication, Study design, Methodology used, Results, Preventive strategy used, Conclusion and Limitations of the study. The collected data were thoroughly reviewed again, and the information was cross verified again to prevent any mistakes during data processing. All the collected data were pooled together and the preventive strategies of AKI from all the studies were analyzed and reviewed.
Quality Assessment
Two independent reviewers assessed study quality according to criteria outlined by Downs and Black using the 27-point checklist included within 5 main sections.
The five sections include questions about:
1. Reporting (10 items);
2. External validity (3 items);
3. In- ternal validity/Bias (7 items);
4. Confounding (selection bias) (6 items);
5. Power of the study (1 item).
Studies were graded as excellent quality if their score was between 24-28 points, good if between 19-23 points, fair if between 14-28 points and poor if less than 14 points.
Outcome Measures
The primary outcome measure for this systematic review is the incidence of acute kidney injury (AKI) following cardiac surgery, categorized according to severity stages outlined in the kidney disease: Improving Global Outcomes (KDIGO) guidelines. Secondary outcome measures include evaluating risk factors associated with AKI, assessing preventive strategies' efficacy, analyzing short and long-term clinical outcomes post-AKI, exploring the utility of biomarkers, assessing healthcare resource utilization, documenting adverse events, and performing subgroup analyses to identify potential sources of heterogeneity.
Results
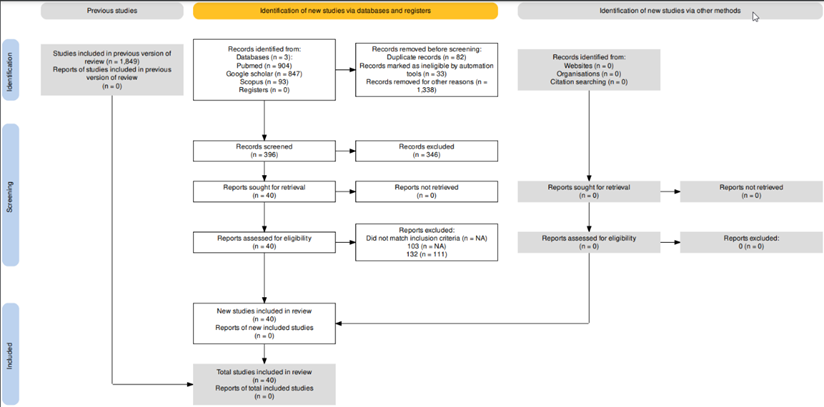
Screening
Of 1849 potential studies, 1338 were excluded because they did not assess patients or had titles and abstracts that were not related to the purpose of this review, 82 were excluded because they were duplicates and 33 records were marked as ineligible by automation tools. After careful screening of the remaining 396 articles, 363 were excluded since they fail to meet the inclusion criteria. The 23 retrieved studies were assessed for eligibility. This review is based on the remaining 23 studies that fully met the inclusion criteria.
Table 1: Characteristics of The Studies Included in The Systematic Review.
Discussion
Acute kidney injury (AKI) remains a significant and frequently encountered complication following cardiac surgery, presenting a formidable challenge to patient recovery and prognosis. This systematic review underscores the substantial burden of cardiac surgery-associated AKI (CSA-AKI), with reported incidence rates ranging from 14% to 50
Limitations
Variability in study designs, patient populations, and interventions across included studies may contribute to heterogeneity. Despite quality assessment, the variability in methodological quality among included studies introduce bias and affect the robustness of the findings. The findings of the systematic review may not be fully generalizable to all patient populations or healthcare settings. The availability of high-quality interventional studies targeting AKI prevention or management post-cardiac surgery were limited, potentially restricting the ability to make firm recommendations for clinical practice.
Conclusion
In conclusion, this systematic review sheds light on the significant burden of acute kidney injury (AKI) following cardiac surgery, emphasizing its detrimental impact on patient outcomes and healthcare systems. Despite advancements in surgical techniques and perioperative care, the incidence of AKI remains substantial, necessitating targeted interventions to mitigate its occurrence. While pharmacological agents such as aminophylline, vitamin C, and selenium did not demonstrate significant efficacy in reducing AKI, promising results were observed with dexmedetomidine administration, the use of renal guard systems, and implementation of KDIGO-based treatment bundles. Furthermore, novel therapeutics like Teprasiran show potential in reducing the frequency and severity of AKI, providing hope for targeted interventions to alleviate the inflammatory cascades and microvascular dysfunction associated with cardiac surgery. Additionally, the identification of early biomarkers such as urinary NGAL and [TIMP-2] × [IGFBP7] offers opportunities for early intervention and preventive strategies, enabling clinicians to identify high-risk individuals and initiate timely interventions. Overall, this review underscores the complexity of AKI pathophysiology, the need for multidisciplinary approaches, and the importance of evidence-based standards in improving renal outcomes post-cardiac surgery. Future research should focus on conducting larger, multicenter trials to validate the efficacy and cost-effectiveness of innovative technologies and therapeutic interventions, ultimately enhancing patient care and reducing the burden of AKI on healthcare systems.
References
- Susantitaphong P., Cruz D.N., Cerda J., et. al. (2013). World Incidence of AKI: A Meta-Analysis. Clin J Am Soc Nephrol. 8:1482-1493.
Publisher | Google Scholor - Pickering JW, James MT, Palmer SC. (2015). Acute Kidney Injury and Prognosis After Cardiopulmonary Bypass: A Meta-Analysis of Cohort Studies. Am J Kidney Dis. 65(2):283-293.
Publisher | Google Scholor - Bellomo R., Ronco C., Kellum J.A., Mehta R.L., Palevsky P.M. (2004). Acute Dialysis Quality Initiative Workgroup Acute Renal Failure—Definition, Outcome Measures, Animal Models, Fluid Therapy and Information Technology Needs: The Second International Consensus Conference of The Acute Dialysis Quality Initiative (ADQI) Group. Crit Care. 8:204-212.
Publisher | Google Scholor - Mehta R.L., Kellum J.A., Shah S.V. et al. (2007). Acute Kidney Injury Network: Report of An Initiative to Improve Outcomes in Acute Kidney Injury. Crit Care. 11:31.
Publisher | Google Scholor - KDIGO. (2012). Clinical Practice Guideline for Acute Kidney Injury Section 2: AKI Definition. Kidney Int Suppl. 1:19-36.
Publisher | Google Scholor - Boldt J, Brenner T, Lehmann A, Suttner SW, Kumle B, et al. (2003). Is Kidney Function Altered by The Duration of Cardiopulmonary Bypass? Ann. Thorac. Surg. 75(3):906-912.
Publisher | Google Scholor - Rosner, M.H., Okusa, M.D. (2006). Acute Kidney Injury Associated with Cardiac Surgery. Clin. J. Am. Soc. Nephrol. 1:19-32.
Publisher | Google Scholor - Haase M, Bellomo R, Devarajan P, Schlattmann P, Haase-Fielitz A. (2009). Accuracy Of Neutrophil Gelatinase-Associated Lipocalin (NGAL) In Diagnosis and Prognosis in Acute Kidney Injury: A Systematic Review and Meta-Analysis. Am. J. Kidney Dis. 54(6):1012-1024.
Publisher | Google Scholor - Greenwood, S. A., Mangahis, E., Castle, E. M., Wang, J., Campbell, J., et al. (2019). Arterial Stiffness Is a Predictor for Acute Kidney Injury Following Coronary Artery Bypass Graft Surgery. Journal of Cardiothoracic Surgery, 14.
Publisher | Google Scholor - Legouis D, Galichon P, Bataille A, Chevret S, Provenchère S, et al. (2017). Rapid Occurrence of Chronic Kidney Disease in Patients Experiencing Reversible Acute Kidney Injury After Cardiac Surgery. Anesthesiology. 126(1):39-46.
Publisher | Google Scholor - National Confidential Enquiry into Patient Outcomes and Death (NCEPOD) Report: Adding Insult to Injury. (2009).
Publisher | Google Scholor - Axelrod, David M., et al. (2016). A Double-Blinded, Randomized, Placebo-Controlled Clinical Trial of Aminophylline to Prevent Acute Kidney Injury in Children Following Congenital Heart Surgery with Cardiopulmonary Bypass. Pediatric Critical Care Medicine. 17(2):135-143.
Publisher | Google Scholor - Eslami, Pegah, et al. (2021). A Randomized, Double-Blind, Placebo-Controlled, Clinical Trial of High-Dose, Short-Term Vitamin D Administration in The Prevention of Acute Kidney Injury After Cardiac Surgery. Cardiorenal Medicine. 11(1):52-58.
Publisher | Google Scholor - McCullough, Peter A., et al. (2016). ABT‐719 for the prevention of acute kidney injury in patients undergoing high‐risk cardiac surgery: a randomized phase 2b clinical trial. Journal of the American Heart Association. 5(8):e003549.
Publisher | Google Scholor - Swaminathan, Madhav, et al. (2018). Allogeneic mesenchymal stem cells for treatment of AKI after cardiac surgery. Journal of the American Society of Nephrology. 29(1):260-267.
Publisher | Google Scholor - Küllmar, Mira, et al. (2020). Biomarker-Guided Implementation of The KDIGO Guidelines to Reduce the Occurrence of Acute Kidney Injury in Patients After Cardiac Surgery (Prev AKI-Multicenter): Protocol for A Multicenter, Observational Study Followed by Randomized Controlled Feasibility Trial. BMJ Open. 10(4):e034201.
Publisher | Google Scholor - Wetz, Anna J., et al. (2015). Does Sodium Bicarbonate Infusion Really Have No Effect on The Incidence of Acute Kidney Injury After Cardiac Surgery? A Prospective Observational Trial. Critical Care. 19:1-10.
Publisher | Google Scholor - Billings, Frederic T., et al. (2016). High-Dose Perioperative Atorvastatin and Acute Kidney Injury Following Cardiac Surgery: A Randomized Clinical Trial. Jama. 315(9):877-888.
Publisher | Google Scholor - Cho, Jin Sun, et al. (2016). Perioperative Dexmedetomidine Reduces the Incidence and Severity of Acute Kidney Injury Following Valvular Heart Surgery. Kidney International. 89(3):693-700.
Publisher | Google Scholor - Grundmann, Franziska, et al. (2018). Preoperative Short‐Term Calorie Restriction for Prevention of Acute Kidney Injury After Cardiac Surgery: A Randomized, Controlled, Open‐Label, Pilot Trial. Journal of the American Heart Association. 7(6):e008181.
Publisher | Google Scholor - Osterholt, Thomas, et al. (2022). Preoperative Short‐Term Restriction of Sulfur‐Containing Amino Acid Intake for Prevention of Acute Kidney Injury After Cardiac Surgery: A Randomized, Controlled, Double‐Blind, Translational Trial. Journal of the American Heart Association. 11(17):e025229.
Publisher | Google Scholor - Zarbock, Alexander, et al. (2021). Prevention Of Cardiac Surgery–Associated Acute Kidney Injury by Implementing the KDIGO Guidelines in High-Risk Patients Identified by Biomarkers: The PrevAKI-Multicenter Randomized Controlled Trial. Anesthesia and Analgesia. 133(2):292-302.
Publisher | Google Scholor - Haase, Michael, et al. (2013). Prophylactic Perioperative Sodium Bicarbonate to Prevent Acute Kidney Injury Following Open Heart Surgery: A Multicenter Double-Blinded Randomized Controlled Trial. PLoS. 10(4):e1001426.
Publisher | Google Scholor - Tasanarong, Adis, et al. (2013). Prophylaxis With Erythropoietin Versus Placebo Reduces Acute Kidney Injury and Neutrophil Gelatinase-Associated Lipocalin in Patients Undergoing Cardiac Surgery: A Randomized, Double-Blind Controlled Trial. BMC Nephrology. 14:1-10.
Publisher | Google Scholor - Marrazzo, Francesco, et al. (2019). Protocol of a Randomized Controlled Trial in Cardiac Surgical Patients with Endothelial Dysfunction Aimed to Prevent Postoperative Acute Kidney Injury by Administering Nitric Oxide Gas. BMJ Open. 9(7):e026848.
Publisher | Google Scholor - Luckraz, Heyman, et al. (2021). Reduction In Acute Kidney Injury Post Cardiac Surgery Using Balanced Forced Diuresis: A Randomized, Controlled Trial. European Journal of Cardio-Thoracic Surgery. 59(3):562-569.
Publisher | Google Scholor - Song, J. W., et al. (2018). Remote Ischemic Conditioning for Prevention of Acute Kidney Injury After Valvular Heart Surgery: A Randomized Controlled Trial. British Journal of Anesthesia. 121(5):1034-1040.
Publisher | Google Scholor - Park, Sun-Kyung, et al. (2016). Risk Factors for Acute Kidney Injury After Congenital Cardiac Surgery in Infants and Children: A Retrospective Observational Study. PLoS One. 11(11):e0166328.
Publisher | Google Scholor - Amini, Shahram, et al. (2018). Selenium, Vitamin C And N-Acetylcysteine Do Not Reduce the Risk of Acute Kidney Injury After Off-Pump CABG: A Randomized Clinical Trial. Brazilian Journal of Cardiovascular Surgery. 33:129-134.
Publisher | Google Scholor - Soh, S., et al. (2016). Sodium Bicarbonate Does Not Prevent Postoperative Acute Kidney Injury After Off-Pump Coronary Revascularization: A Double-Blinded Randomized Controlled Trial. BJA: British Journal of Anaesthesia. 117(4):450-457.
Publisher | Google Scholor - Thielmann, Matthias, et al. (2021). Teprasiran, A Small Interfering RNA, For the Prevention of Acute Kidney Injury in High-Risk Patients Undergoing Cardiac Surgery: A Randomized Clinical Study. Circulation. 144(14):1133-1144.
Publisher | Google Scholor - Moriyama, Takahiro, et al. (2017). The Protective Effect of Human Atrial Natriuretic Peptide on Renal Damage During Cardiac Surgery. Journal of anesthesia. 31:163-169.
Publisher | Google Scholor - Meersch, Melanie, et al. (2014). Urinary TIMP-2 and IGFBP7 as early biomarkers of acute kidney injury and renal recovery following cardiac surgery. PloS One. 9(3):e93460.
Publisher | Google Scholor