Research Article
What Role Does Allergic Rhinitis Play in The Association Seromucous Otitis and Adenoids Hypertrophy in Children
1ENT and CCF service. Army Central Hospital. Algiers, Algeria.
2ENT and HNS service. Regional military university hospital, Algeria.
3B. Bensmaïl Faculty of Medicine, Boubenider University, Algeria.
*Corresponding Author: Mohamed Cherif, ENT and CCF service. Army Central Hospital. Algiers, Algeria.
Citation: Cherif M, Merdjana S, Benchaoui M. (2024). What Role Does Allergic Rhinitis Play in The Association Seromucous Otitis and Adenoids Hypertrophy in Children, International Journal of Biomedical and Clinical Research, BioRes Scientia Publishers. 1(4):1-5. DOI: 10.59657/2997-6103.brs.24.023
Copyright: © 2024 Mohamed Cherif, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: July 10, 2024 | Accepted: August 23, 2024 | Published: August 30, 2024
Abstract
Introduction: Sero-mucosal otitis (SMO) is one of the most common chronic ear conditions of childhood and is the leading cause of acquired hearing loss in children. It is a pathology recognized as multifactorial and several risk factors for this pathology have been studied and their association has been proven. However, the association with allergic rhinitis (AR) still remains controversial. The main objective of this study is to determine the prevalence of allergic rhinitis in children suffering from seromucous otitis associated or not with hypertrophy of the adenoids. This study also aims to identify common respiratory allergens associated with allergic rhinitis.
Material and Methods: This is a prospective, descriptive study, targeting a group of 80 children, aged between 4 and 14 years old and presenting confirmed SMO, persistent after 3 months of monitoring, with or without hypertrophy of the adenoids and in whom the decision to install ATT alone or in combination with an adenoidectomy has been made. This study spanned 24 months, from January 2020 to January 2022. Allergic skin tests (Prick tests) were requested in all children who presented rhinological signs suggestive of allergic rhinitis.
Results: In the 59 children suspected of having allergic rhinitis, the prick tests came back positive in 81.36% of cases (n= 48). The almost majority of patients were allergic to dust mites (DPT, DF and blomia), molds and 5-grasses.
Discussion: Our results are close to those of other studies in the world literature, supporting that this factor seems to be determining in the etiopathogenesis of SMO.
Conclusion: The role that allergic rhinitis plays in the etiopathogenesis of SMO seems to be decisive, but a larger study with, if possible, a control group would be necessary to confirm these findings in our population.
Keywords: seromucous otitis; allergic rhinitis; skin tests
Introduction
Sero-mucous otitis (SMO) is an extremely common pathology since almost all preschool children are affected at some point in their development. It is estimated that 80% of children have had an episode of SMO before the age of 10 [1,2]. It is a complex, multifactorial pathology where different processes are self-sustaining to create the vicious circle of intra-tympanic effusion [3]. Several risk factors have been studied such as age, passive smoking, insufficient breastfeeding, GERD, attendance at daycare and many others also with their proven association. However, the association with allergic rhinitis (AR) still remains controversial. In children with seromucous otitis (SMO), the prevalence of allergic rhinitis differs from one country to another, varying between 28% and 92% [4]. The main objective of our study is to determine the prevalence of allergic rhinitis in children suffering from seromucous otitis associated or not with hypertrophy of the adenoids (AH). This study also aims to identify common respiratory allergens associated with allergic rhinitis.
Material and Methods
This is a prospective, descriptive study, targeting a group of 80 children (160 ears) aged between 04 and 14 years, presenting confirmed seromucous otitis, persistent after 03 months of monitoring, associated or not with hypertrophy. adenoids. This study spanned 24 months, from January 2020 to January 14, 2022, and it took place at the ENT and HNS department of the Constantine Regional Military University Hospital and the ENT department and HNS of the Benbadis University Hospital Center of Constantine.
A questionnaire was completed by the parents of all patients, looking for different risk factors (according to international literature) and especially for signs of allergic rhinitis (rhinorhea, sneezing, nasal obstruction, etc.).
All patients underwent an otoscopic examination, a tympanogram and an endoscopic examination of the nasopharynx with classification of adenoids according to the Clemens & Mcmurray Score. Allergic skin tests (Prick tests) were requested in all children who presented rhinological signs suggestive of allergic rhinitis. These children were put on anti-allergic treatment (oral antihistamines + nasal corticosteroids) for 3 months and then they received a second examination.
Results
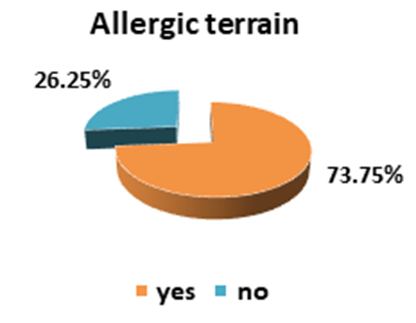
At the first examination we found in all our patients otoscopic aspects suggestive of MSO (dull, bluish appearance, retrotympanic bubbles), a type B tympanogram according to the Jerger classification, and the endoscopic appearance of the adenoids was classified according to the Clemens & Mcmurray Score: grade I (15%, 12/80), grade II (16.25%, 13/80), grade III (61.25%, 49/80) and grade IV (07.5 %, 6/80). Respiratory allergy (associated or not with bronchial asthma) represents 73.75% (n=59) of cases (Figure 1).
Figure 1: Distribution of patients according to the presence of allergic signs.
Nasosinusal allergy was suspected in the presence of suggestive clinical symptoms (watery rhinorrhea, tilting nasal obstruction, nasal and/or conjunctival pruritus). Diagnostic confirmation was based on skin reaction to allergens (Prick Test). In the 59 children suspected of having allergic rhinitis, the prick tests came back positive in 81.36% of cases (n= 48). (Table 1).
Table 1: Prick test results.
| Prick Test | Frequency | % |
| Negative | 11 | 18,64% |
| Positive | 48 | 81,36% |
| Total | 59 | 100,00% |
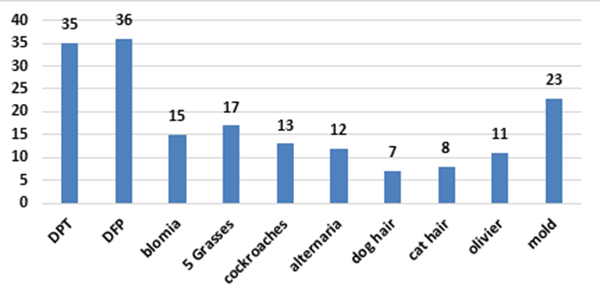
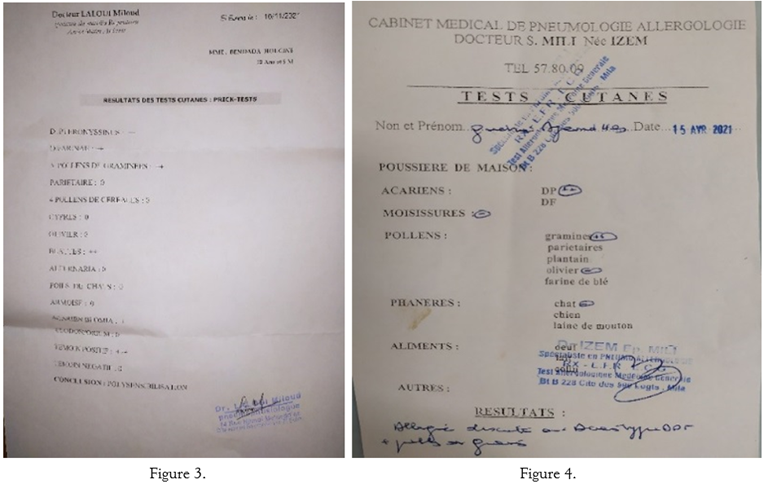
The almost majority of patients were allergic to dust mites (DPT, DF and blomia), molds and 5-grasses. We also noted several cases of polysensitization (several allergens) (Figures 2,3,4).
Figure 2: Prick test results (allergens found).
Figures 3,4: Positive prick tests. Personal iconography.
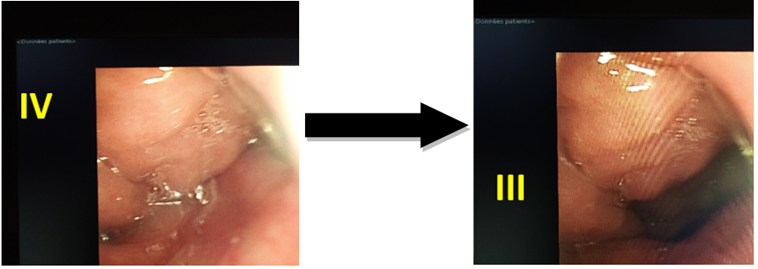
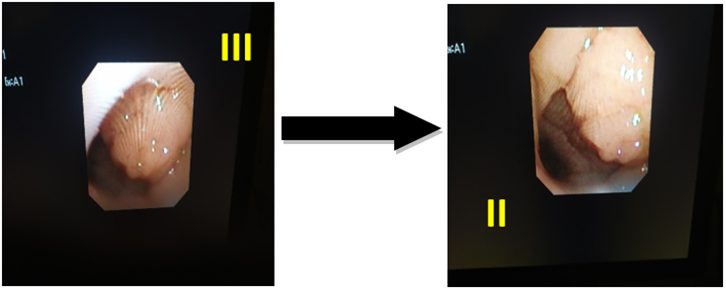
Among the 11 children with a negative prick test, we were able to perform specific IgE in only 4 of them and they came back positive. Finally, 4 children in whom bronchial asthma was suspected (wheezing ++), were referred to our pulmonologist colleagues, who after clinical and paraclinical examination (RFE), confirmed the diagnosis of bronchial asthma and the children were placed under appropriate treatment. During the second nasal endoscopic examination, a slight decrease in the volume of the adenoids was noted with transformation of seven (07) cases from grade III to grade II and two (02) cases from grade IV to grade III (Figure 5.6).
Figure 5: transformation of two (2) cases from grade IV to grade III.
Figure 6: transformation of seven (7) cases from grade III to grade II.
Discussion
Séro-mucus otitis (SMO) is an extremely common condition, which in the vast majority of cases affects children under 10 years old. Its frequency is difficult to assess and differently described in world literature. It is the most common cause of deafness in children [5]. Allergy is probably involved in the pathogenesis of SMO and its role has been proposed following several mechanisms, especially through inflammation of the mucosa of the middle ear and the Eustachian tube. Several authors have been interested in the role that allergic rhinitis (AR) and allergy in general can play in the pathogenesis of SMO, such as: Fernandez and McGovern, who among 113 children with SMO found 83 % of them allergic based on history and 92% had a positive skin test [4]. Alles R et al also found a similar rate, because in 209 children with OSM they found that 89% had AR. Lecks et al also tested 82 children with SMO using a skin test and found that 72 (88%) of the children had positive results [4].
Jordan et al reported a rate of 74% (91/123) of AR in children with SMO, while Norhafizah S et al found a prevalence of AR of 52.3% (68/130) [4]. A fairly recent meta-analysis investigating the causal link between RA versus SMO supports the fairly important role that RA plays in the pathogenesis of SMO [6]. In our study, respiratory allergy (allergic rhinitis associated or not with bronchial asthma) represents 73.75% (n=59) of cases, which was quite close to the previous results. Other authors have demonstrated lower AR prevalence rates, such as Chul Kwon et al, who found an AR prevalence rate of 33.8% in 370 children with SMO [7], as well as the team of Melanie Anne Souter, who by studying a group of 89 children suffering from SMO, found a prevalence of AR of around 38.2% [8]. Passali D et al reported that out of 100 children aged 04 to 09 years presenting with AR, 45 had SMO and 25 had tubal dysfunction [9], while Benjamin C. Pau, by examining 159 children aged 04 to 12 years old and presenting allergic rhinitis, found a prevalence of SMO of around 7.5% (12/159) [10].
Y. Yazibane [11], in his study had a respiratory allergy rate of 26% of cases. Prick tests were positive in all 26 cases, with 70% allergic to dust mites. For the association of SMO and AH, Bemanian et al found in 122 patients aged under 18 years suffering from SMO and adenoid hypertrophy, an allergy prevalence of 28% (34/122) [12] and the African meta-analysis by Choffor-Nchinda et al, in 2020, confirms the causal link between SMO and RA with AH [13]. In our study, the use of anti-allergic treatment contributed to the reduction in the volume of the adenoids and this could contribute to the resolution of the intra-tympanic effusion. Among the aeroallergens studied in skin tests, dust mites were the most frequently found, as in the study by Norhafizah S et al who found Dermatophagoides pteronyssinus (DP) 87.7%, Dermatophagoides farinae (DF) 86.2% and Blomia tropicalis 63.1% [4]. In our study, we found a fairly similar result: Dermatophagoides pteronyssinus (DPT) 35 (72.91%), Dermatophagoides farinae (DFP) 36 (75%), as well as grass pollens 5 (10.41%) and molds. 23 (47.91%).
Conclusion
Seromucous otitis (SMO) remains an extremely common pediatric condition, constituting the main cause of hearing loss in children and whose etiopathogenesis is multifactorial.
Allergic rhinitis seems to be a determining factor in the etiopathogenesis of SMO associated or not with hypertrophy of the adenoids, but a larger study with a control group would be necessary to confirm these findings in our population (perspectives of our work).
Such findings would be favorable to the management of seromucous otitis associated with allergic rhinitis, using adequate anti-allergic therapy, starting with an avoidance of allergens, through medical treatment and possibly specific immunotherapy, which would be perhaps a definitive treatment.
Conflicts of Interest
The authors declare that they have no conflict of interest regarding the publication of this article.
References
- Rosenfeld RM, Shin JJ, Schwartz SR, et al. (2016). Clinical Practice Guideline: Otitis Media with Effusion (Update). Otolaryngology-Head and Neck Surgery. 154(1_suppl):S1-S41.
Publisher | Google Scholor - Zernotti, M.E., Pawankar, R., Ansotegui, I. et al. (2017). Otitis Media with Effusion and Atopy: Is There a Causal Relationship? World Allergy Organ J. 10:37.
Publisher | Google Scholor - Kubba, H., Pearson, J.P., Birchall, J.P. (2000), The Aetiology of Otitis Media with Effusion: A Review. Clinical Otolaryngology and Allied Sciences, 25(3):181-194.
Publisher | Google Scholor - Norhafizah S, Salina H, Goh BS. (2020). Prevalence of Allergic Rhinitis in Children with Otitis Media with Effusion. Eur Ann Allergy Clin Immunol. 52(3):121-130.
Publisher | Google Scholor - Triglia J, Roman S, Nicollas R. (2003). Seromucosal Otitis. Encycl Med Chir (Scientific and Medical Editions Elsevier SAS, Paris, Oto-rhino-laryngology.
Publisher | Google Scholor - Cheng X, Sheng H, Ma R, Gao Z, Han Z, et al. (2017). Allergic Rhinitis and Allergy Are Risk Factors for Otitis Media with Effusion: A Meta-Analysis. Allergol Immunopathol. 45(1):25-32.
Publisher | Google Scholor - Kwon C, Lee HY, Kim MG, Boo SH, Yeo SG. (2013). Allergic Diseases in Children with Otitis Media with Effusion. Int J Pediatr Otorhinolaryngol. 77(2):158-161.
Publisher | Google Scholor - Souter MA, Mills NA, Mahadevan M, Douglas G, Ellwood PE, et al. (2009). The Prevalence of Atopic Symptoms in Children with Otitis Media with Effusion. Otolaryngol Head Neck Surg. 141(1):104-107.
Publisher | Google Scholor - Passali D, Passali GC, Lauriello M, Romano A, Bellussi L, et al. (2014). Nasal Allergy and Otitis Media: A Real Correlation? Sultan Qaboos Univ Med J. 14(1):e59-e64.
Publisher | Google Scholor - Pau BC, Ng DK. (2016). Prevalence Of Otitis Media with Effusion in Children with Allergic Rhinitis, A Cross Sectional Study. Int J Pediatr Otorhinolaryngol. 84:156-160.
Publisher | Google Scholor - Y. Yazibane. (2012). OSM Clinical, Evolutionary and Management Aspects. THESIS For Obtaining the Degree of Doctor in Medical Sciences.
Publisher | Google Scholor - Bemanian MH, Rezaei K, Atighechi S, Shafiei A. (2020). The Relation of Allergy to Adenoid Hypertrophy and Otitis Media with Effusion: A Cross-sectional Study. Iran J Allergy Asthma Immunol. 19(5):529-533.
Publisher | Google Scholor - Choffor-Nchinda E, Bola Siafa A, Nansseu JR. (2020). Otitis media with effusion in Africa-prevalence and associated factors: A systematic review and meta-analysis. Laryngoscope Investig Otolaryngol. 5(6):1205-1216.
Publisher | Google Scholor