Case Report
Vulvar Endometriosis: A Case Report
- Samia Bennaceur
- Nassima Ouguerzi
- R. Laaboudi
- Jaouad Kouach *
Department of Gynecology-Obstetric, Military Training Hospital Med V, Faculty of Medicine and Pharmacy, Mohammed V University, Rabat, Morocco.
*Corresponding Author: Jaouad Kouach, Department of Gynecology-Obstetric, Military Training Hospital Med V, Faculty of Medicine and Pharmacy, Mohammed V University, Rabat, Morocco.
Citation: Bennaceur S., Ouguerzi N., Laaboudi R., Kouach J. (2024). Vulvar Endometriosis: A Case Report, Clinical Obstetrics and Gynecology Research, BioRes Scientia Publishers. 3(2):1-11. DOI: 10.59657/2992-9725.brs.24.014
Copyright: © 2024 Jaouad Kouach, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: April 24, 2024 | Accepted: June 25, 2024 | Published: July 03, 2024
Abstract
Endometriosis is a rare pathological entity. It is defined by the presence of endometrial tissue in the vulva. It most often occurs at the level of episiotomy scars. The clinical symptomatology was characterized by a vulvar nodule accompanied by cyclical perineal pain. Imaging has to be performed by an operator trained to confirm the diagnosis. Surgery is the standard treatment. To prevent recurrences, it can be preceded or accompanied by hormonal treatment. The aim of this work is to specify the peculiarities of this rare pathology through A case reports.
Keywords: vulvar endometriosis; diagnosis; surgery; episiotomy scar
Introduction
Vulvar endometriosis is the presence of endometrial tissue in the vulva. History such as episiotomy, obstetrical tearing or perineal interventions often associated with intrauterine manipulation are frequently found. Vulvar endometriosis is often the subject of a few sporadic articles in the literature in the form of small case series or generally a single clinical case.
Case Report
A 31-year-old woman, gravida 3 para 2, with a history of early miscarriage without curettage and 2 vaginal deliveries with mediolateral episiotomy, the latter performed six years before. She reported cyclical onset of painful perineal swelling progressing over the last 5 years. Clinical examination, carried out on day 9 of the menstrual cycle, revealed bluish mass measuring about 1 cm at the level of the episiotomy scar, slightly painful to palpation.
Figure 1: Endometrial nodule at the level of the episiotomy scar
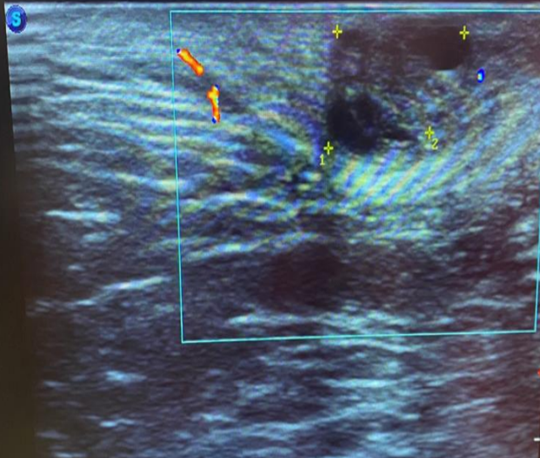
A transperineal ultrasound showed superficial heterogeneous hypoechoic lesion measuring 13.65 x 10.34 mm, with no vascularization on the doppler. The patient underwent a mass resection.
Figure 2: Transperineal ultrasound showing an endometriosis nodule.
Histological examination confirmed the diagnosis of scar endometriosis with a wide 1 cm margin of surrounding normal tissue. The postoperative course was simple, and the patient reported complete resolution of symptoms.
Figure 3: Excised endometriotic mass.
Discussion
The first observation of vulvar endometriosis was reported in 1923 and that of endometriosis of the anal canal in 1968. Endometriosis is a common gynecologic disorder characterized by the presence of endometrial glands and stroma outside the uterine cavity. Regarding vulvar endometriosis, there are no data on the specific prevalence in the general population. Nevertheless, the few studies conducted have demonstrated that the vulvar endometriosis represent less than 1% of cases of endometriosis that are surgically treated, as reported in the literature with episiotomy scars as the most common site.
It is important to remember that asymptomatic lesions represent 25% to 50% of cases [1]. The cyclic perineal pain is the main symptom [2,3], which was found in all our patients. Inspection may identify a purplish or bluish vulvar nodule or cyst. Its volume varies according to the menstrual cycle and its chocolate contents are pathognomonic. Vaginal examination searches for vulvar nodules preferably located at the level of the uterosacralligaments with a painful tensioning, on the posterior surface of the uterine isthmus, or on the rectovaginal septum.
Rectal touch is required in vulvar endometriosis, because it must look for an anorectal infiltration and a rectovaginal septum. Therefore, the touch must be bi-manual. Transperineal ultrasound must be performed by an operator trained in endometriosis and during the first part of the cycle [4]. The lesions of the vulvar endometriosis are not specific. They can be hypoechoic and heterogeneous (depending on their solid and/or liquid component), sometimes hyperechoic (haemorrhagic forms) with irregular limits.
RMI, like the ultrasound, it must be performed by an operator trained in endometriosis. It is the essential imaging for the diagnosis of endometriosis, because it establishes the necessary mapping of endometriotic lesions [5]. It explores areas that are not easily accessible to ultrasound, in particular the rectovaginal septum. It visualizes the smallest lesions, which are around 4 to 5 mm [6]. Endometriotic lesions on episiotomy scars are characterized on MRI by fibrous thickening in hypo signal on T2 sequences [7].
Vulvar endometriosis may be confused with desmoid tumour, abscess, lipoma, hematoma, granuloma, lymphoma, or even primary cancer or metastases. For the medical treatment, it is recommended to use paracetamol or NSAIDs as an analgesic, alone or in combination for a short trail (for example 3 months) [8]. Hormone treatment includes combined hormonal contraceptives, progestogens, GnRH agonists, or GnRH antagonists. It provides only short-term relief of symptoms, and recurrence was common after the treatment was stopped.
So, the hormone therapy could be used only as a neoadjuvant therapy, when the lesion is massive or has anal sphincter involvement, to reduce the size of the mass, or adjuvant therapy when the excision is incomplete, or an alternative to surgery for recurrent lesions. The surgical treatment of vulvar endometriosis includes complete surgical excision. It can be performed under local [9], loco regional or general [10] anesthesia, depending on the size of the nodule.
Wide excision of the endometrial tissue with a good healthy margin is necessary even if this necessitates primary sphincteroplasty when the anal sphincter is involved. An incomplete excision with hormonal suppression may be advantageous in older patients nearing the menopause to lessen the risk of incontinence with sphincter resection.
Conclusion
Vulvar endometriosis is a relatively rare pathology. Establishing the diagnosis of this pathology remains very equivocal. Perineal ultrasound remains an essential and inexpensive morphological examination for diagnosing vulvar endometriosis, and eliminating any differential diagnosis. If in doubt about the diagnosis before surgery, MRI remains the examination of choice for vulvar endometriosis. Surgery is the standard treatment. To prevent recurrences, it can be preceded or accompanied by hormonal treatment. the diagnosis of certainty is only confirmed by histological study.
Declarations
Conflict of Interest
No conflict of interest.
Funding
No funding.
Consent Informed
Written consent obtained from the patient.
References
- Luisi S, Lazzeri L, Ciani V, Petraglia F. (2009). Endometriosis in Italy: from cost estimates to new medical treatment. Gynecol. Endocrinol. 25(11):734-740.
Publisher | Google Scholor - Juanqing Li, Yifu Shi, Caiyun Zhou, Jun Lin. (2015). Diagnosis and treatment of perineal endometriosis: review of 17 cases, Archives of Gynecology and Obstetrics. 292:1295-1299.
Publisher | Google Scholor - Na Chen, Lan Zhu, Zhufeng Liu, Dawei Sun, (2012). The clinical features and management of perineal endometriosis with anal sphincter involvement: a clinical analysis of 31 cases. Human Reproduction, 27(6):1624-1627.
Publisher | Google Scholor - Maubon A, Bazot M. (2007). Endometriosis Imaging. J Gynecol Obstet Biol Reprod. 36(2):129-134.
Publisher | Google Scholor - M. Canis, A. Fauconnier. (2006). Recommendations for clinical practice: Management of endometriosis. CNGOF (National College of French Obstetrician Gynecologists).
Publisher | Google Scholor - Takahashi K, Okada M, Imaoka I, Sugimura K. (1996). Studies on the detection of small endometrial implants by magnetic resonance imaging using a fat saturation technique. Gynecol. Obstet. Invest. 41(3):203-206.
Publisher | Google Scholor - Robert Y, Launay S, Mestdagh P. et al. (2002). MRI in gynecology. J Gynecol Obstet Biol Reprod. 31(5):417-439.
Publisher | Google Scholor - Kuznetsov, L., Dworzynski, K., Davies, M., & Overton, C. (2017). Diagnosis and management of endometriosis: summary of NICE guidance. BMJ, 358.
Publisher | Google Scholor - Watanabe M, Kaliyama G, Yamazaki K, et al. (2003). Anal endosonography in the diagnosis and management of perianal endometriosis: report of a case. Surg Today. 33(8):630-632.
Publisher | Google Scholor - Rakotomalala L, De Parades V, Parisot C. (1998). Ano-perineal endometriosis with external sphincter involvement: a rare disorder. Gastroenterol Clin Biol. 22(4):476-477.
Publisher | Google Scholor