Research Article
Visual Evoked Potential After Levodopa in Amblyopic Eyes
- Mona Abdelkader MD *
- Sameh Saleh MD
- Ayman Fawzy MD
Department of Ophthalmology, Faculty of Medicine, Mansoura University, Egypt.
*Corresponding Author: Mona Abdelkader, Department of Ophthalmology, Faculty of Medicine, Mansoura University, Egypt.
Citation: M Abdelkader, S Saleh, A Fawzy. (2022). Visual Evoked Potential After Levodopa in Amblyopic Eyes. Journal of BioMed Research and Reports, BRS Publishers. 1(1); DOI: 10.59657/2837-4681.brs.22.003
Copyright: © 2022 Mona Abdelkader, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: August 01, 2022 | Accepted: August 26, 2022 | Published: September 05, 2022
Abstract
Purpose to study the clinical and electrophysiological changes after Levodopa in amblyopic eyes.
Methods: Fifty patients with amblyopia (20 hypermetropic anisometropia and 20 myopic anisometropic amblyopia,10 astigmatic amblyopic) were included in this study, Levodopa was administered daily for 6 weeks associated with occlusion therapy and visual training. The drug was stopped and patients continued on occlusion therapy associated with visual training for another 6 weeks. Then gradual reduction of occlusion time and visual training was performed for another 6 weeks, and finally all treatments were stopped for 6 weeks. Visual acuity and visual evoked potentials (VEP), including both multifocal VEP (MFVEP) and Pattern VEP (PVEP) were recorded before the treatment, at 1,6,12,18,24weeks after beginning of treatment.
Results: Significant improvement of visual acuity (mean 0.50), with stabilization at the end of the 6th week associated with improved PVEP and MFVEP parameters was reported. Stabilization of the visual improvement after stoppage the treatment without any deterioration of vision or VEP parameters.
Conclusion: Improved visual acuity with stabilization can be achieved with combined Levodopa, occlusion and visual training therapy confirmed with VEP improvement.
Keywords: levodopa; amblyopic; eyes; visual acuity; hypermetropic; myopic; astigmatic; amblyopia
Introduction
Amblyopia (lazy eye) is the condition in which reduced visual function exists despite full optical correction and in the absence of observable ocular pathology. It represents a developmental disorder due to anomalous visual experience that occurred during the sensitive period in early visual development [1]. This result from physiological alternation and dramatic changes occurring in the cortical function (cortical area 17) with a competitive interaction between the cortical afferents from the two eyes resulting in loss of cortical binocularity and a shift in cortical eye dominance away from the affected eye [2]. It is often successfully treated by patching of the sound eye in infants and young children, but has been widely considered untreatable in adults. However, a growing number of recent studies have suggested that there is substantial plasticity in the visual system of adults and the connection from the amblyopic eye may be suppressed rather than destroyed [3-5]. Levodopa has been shown to improve visual acuity in amblyopic eyes [6]. A number of studies have shown visual evoked responses (VEP) in amblyopia to be abnormal [7-9].
The purpose of this study was to find the effect of Levodopa with occlusion therapy on the visual acuity and optic nerve electrophysiological performance of adult amblyopic eyes.
Patients and Methods
This study was approved by the Medical Research Ethics Committee of Mansoura University. Fully informed, signed consent was obtained from each subject before participation. sixty patients of anisometropic amblyopia participated, but 10 patients were excluded after one week because of intolerated side effect
All patients underwent complete history taking, including the age of patient, previous treatment, general history and family history.
A full ophthalmological examination including uncorrected and best corrected visual acuity measurements, slit lamp examination, fundus examination, and cycloplegic refraction. Amblyopia was defined as a difference of two or more lines in the visual acuity between the two eyes while fixing at 6 meters.
Refractive errors were initially determined by the autorefractomer (Topcon) and then confirmed by retinoscopy, all were fully corrected and had no other ocular pathology than amblyopia, Snellen visual acuity of the amblyopic and dominant eye for each patient was measured, converted to decimal notation and recorded. All patients were diagnosed as having anisometropic amblyopia with more than three diopters difference between both eyes in hypermetropic patients and over than 6 diopters difference between both eyes in myopic patients, spherical equivalent was used to facilitate statistical analysis.
Both MFVEP and PVEP were performed for the sound and amblyopic eyes before receiving the drug and occlusion therapy. General medical consultation was performed for assessment of cardiovascular, respiratory and gastrointestinal systems; also, a neuropsychiatric consultation was performed.
Exclusion criteria
Patients with bronchial asthma, history of peptic ulcer, renal or hepatic patients, patients with psychosis, history of convulsion or receiving neuroleptic drugs, or positive history of previous amblyopia therapy were excluded.
Amblyopia therapy protocol
In the first visit, Snellen's best visual acuity was measured for amblyopic and sound eyes and converted to decimal notation, which were recorded in a separate sheet for each patient associated with their refractive errors and visual evoked potentials results (PVEP, MF-VEP). Full optical correction was prescribed (in the form of contact lenses).
Oral tablets Carbidopa-Levodopa, MSD (Sinemet ® 25/250 Merch & Co.,Inc Whitehouse Station, NJ), was prescribed; to be administered orally in a dose of (4mg/kg body weigh twice a day), associated with part time occlusion of the sound eye (patch occlusion) for 6 hours per day. This continued daily for one week (until the 2nd visit). Patients were instructed to do active visual training during occlusion, from just painting or coloring pictures up to playing video games according to the patient's visual acuity at the start of treatment. Also, patients were informed about the possible side effects of the drugs.
In the second visit (after one week), measuring the visual acuity started with the amblyopic eye then the sound eye and recorded in each sheet, recording any side effects of the drug, (the most common side effects were nausea, vomiting, muscle twitching and blepharospasm. These reactions occurred in 15 patients and were diminished by reduction of the dose (2 mg/kg body weight twice a day)). Ten patients did not continue in this study due to severe adverse reaction of the drug (severe vomiting not reduced with reduction of the dose (three patients), dyskinesia (four patients) and syncope with hypotensive episodes (three patients).
Fifty patients (twenty patients had hypermetropic anisometropia, twenty patients had myopic anisometropia and ten patients had astigmatic amblyopia) continued on the drug administration and occlusion of the sound eye. They were examined (both visual acuity and VEP) regularly at one week interval, till establishment of improved visual acuity. So, the drug administration was stopped.
#The patients then continued on occlusion therapy (6 hours per day) and visual training for another 6 weeks (end of 6th week to end of 12th week), this was to avoid regression of the improved visual acuity.
#Gradual reduction of occlusion time (one hour \ week) was prescribed for another 6 weeks (from 12th to 18th week), followed by stoppage of all treatments for the last 6 weeks (from the end of the 18th week to the end of the 24th week).
#VEP (PVEP and MF-VEP) were performed at the first visit before starting the treatment and regularly at 1,6,12,18 ,24 weeks.
#At the end of 24 weeks (6th month), both visual acuity and visual evoked potentials were compared with previous records.
VEP was recorded using Roland Consult, Brandenburg, Germany,
The electrodes were placed after cleaning the skin and placing conductive plast (TEN20). The signals were fed into an amplifier and band-pass filtered at 1–30 Hz.
PVEP
The stimulus was a reversing checkerboard displayed on a CRT color monitor at 21 sizes. The luminance of the white checks was 120 cd/m2 and for the black checks was 1.0 cd/m2, producing a Michelson contrast of 98%. The background luminance was kept constant all over the test period. To obtain PVEP, the signals were fed into an amplifier and band-pass filtered at 1–30 Hz. The amplifier range was ± 100 µV.
The size of the checkerboard stimuli were 15 minutes reversal of checks was done at a rate of two reversals per second. The recording procedure was repeated if the artifacts percentage was more than 10%.
Subjects were comfortably sitting in chairs and were asked to fixate on the red spot at the center of checkerboard. The patient monitor distance was 1 meter. All subjects were refracted optimally. Pupils weren't dilated, with a dim room light. Each eye was examined separately with the other eye patched.
The positive electrode was connected to the midline of the head at two fingers breadth above the inion (projection at the back of the head). The ground electrode was connected in the midline of the head at the level of the ear lobule. The negative electrode was connected to the middle of the forehead.
MFVEP
The stimulus array consisted of 60 sectors arranged in dartboard-pattern, each with 16 checks, comprising 8 black and 8 white. The stimulus array was cortically scaled and displayed on a CRT color monitor of 21 size driven at a frame frequency of 75 Hz/sec. The luminance of the white checks was 120 cd/m2 and for the black checks was 1.0 cd/m2, producing a Michelson contrast of 98%. The background luminance was kept constant all over the test period. The diameter of the first stimulus ring was 0.5–3.0° of arc, 3.0–7.0° for the second stimulus ring, 7.0–12.0° for the third stimulus ring, 12.0–18.0° for the fourth stimulus ring and 18.0–26.0° for the fifth stimulus ring.
The reversal of the 60 segments was controlled by binary pseudorandom sequences named M-sequence (its length 1024 elements/reversals) derived from a family of sequences called Kasami sequences. Duration of the run or frame was 13.3 ms (1/75 Hz), the number of frames used was 5. So, a cycle of stimulation duration would be (1024×13.3×5) ms, the recording procedure was repeated if artifacts percentage was more than 10%.
Subjects were comfortably sitting in chairs and were asked to fixate on lines at the center of the dartboard-pattern. The distance to the monitor was 31 cm, producing 31° viewing angle. All subjects were refracted optimally. Pupils were not dilated, and a dim room light was always on. Each eye was examined separately with the other eye patched.
Signals picking up was done through electrodes placed on specific regions of the patient's head. The electrodes were active, reference and ground electrodes. The active and reference electrodes were bipolar occipital inion straddle electrodes using a special holding system. It consists of two electrodes positioned 4 cm from the inion on either side of midline and two placed 3.5 cm above and 3 cm below the inion in the midline. Electrical signals were recorded along four channels; each channel being the difference in electrical signal between two electrodes. The vertical and horizontal channel recordings were derived from the vertical and horizontal electrodes respectively. The left and right oblique channels were recorded as the difference between the lower electrode and the left and right horizontal electrodes respectively. The reference electrode was placed at Fp1 point of the international 10/20 system.
Statistical analysis
Statistical analysis was performed using SPSS program version 23. The comparison of results was done at the end of the first week, end of the 6th week (after stoppage of levodopa), end of 12th week (after occlusion and training therapy alone), end of 18th weeks (after gradual reduction of occlusion and training time), and the end of 24th week (after stoppage of all treatments).
Results
The study included 50 patients; with the aged 15-25 years the mean was 19.8 (± 4.5) years. 15(30%) were males and 35 (70%) were females. Fifteen patients had hypermetropic anisometropia, fifteen patients had myopic anisometropia, ten patients had astigmatic amblyopia Mean visual acuity of amblyopic eyes was 0.10 ± .05, mean visual acuity of fellow eyes was 1.00, the difference of visual acuity between both eyes was statistically significant (p = 0.001). The mean visual acuity of hyperopic anisometropic amblyopia was 0.10 ± .02, the mean visual acuity of myopic anisometropic amblyopia was 0.10 ± .03and the mean visual acuity of astigmatic amblyopia was 0.09 ± .03. There was no statistically significant difference between different types of amblyopia.
Compared to the first examination before therapy, an increase of the mean visual acuity was obtained (0.25 ± .03) after one week of levodopa administration and occlusion therapy, which was statistically significant. Gradual increase of the mean visual acuity occurred in the next 3 weeks (2nd, 3rd and 4th weeks), at the end of the 5th and 6th weeks no further improvement of visual acuity occurred, the mean visual acuity was 0.50 ± 0.11, so levodopa was stopped at the end of 6th week.
On occlusion therapy and visual training, minimal non-significant improvement occurred during the next two weeks (7th and 8th) and was maintained for the next 6 weeks, the mean was 0.50 ± 0.17, and lasting to the end of the 24th week (end of 6 months), as shown in table 1. No significant difference was found between improved visual acuity of hypermetropic, myopic and astigmatic amblyopia.
Table 1: Visual acuity along treatment and follow up periods.
| Type of Amblyopia | Best corrected visual acuity | |||||
| Before treatment | End of 1st week | End of 6th week | End of 12th week | End of 18th week | End of 24th week | |
| Myopic | 0.10±.03 | 0.16±0.4 | 0.25±0.3 | 0.33±0.2 | 0.33±0.2 | 0.33±0.2 |
| Hypermetropic | 0.10±.02 | 0.10±0.3 | 0. 5±0.2 | 0.50±0.2 | 0.50±0.14 | 0.50±.16 |
| Astigmatic | 0.09±.03 | 0.25±0.2 | 0.50±0.1 | 0. 50±0.1 | 0.67±0.2 | 0.67±18 |
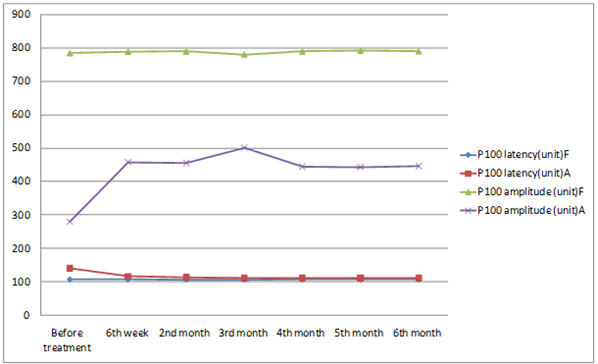
Regarding PVEP, P100 amplitudes and latencies were statistically significant with (p = 0.001) between the amblyopic eyes and the fellow eyes. There were statistically significant prolongation of latencies and reduction of amplitudes between amblyopic and sound eyes. There was improvement of latencies and amplitudes after treatment through first 6 weeks, then stabilization of PVEP parameters till the end of follow up period in amblyopic eyes. While in fellow eyes no significant difference was noticed between pre-treatment & post-treatment. (Table 2, figures 1,2).
Table 2: PVEP Changes during follow up period
| P1 amplitude (n ( | P1 latency) ms) | |||
| Amblyopic eye | Fellow eye | Amblyopic eye | Fellow eye | |
| Before treatment | 280.2±27.7 | 784±40.3 | 140.2±10.5 | 106.6±5.7 |
| 6 weeks | 458±21.7 | 788.2±41.2 | 116±8.6 | 106.6±5.8 |
| 12 weeks | 455± 22.7 | 789.4±39.8 | 113.6±7.8 | 106.4±5.41 |
| 18 weeks | 448± 23.7 | 779.9±39.5 | 111.6±6.4 | 106.3±5.54 |
| 24 weeks | 444± 22.5 | 789±39.7 | 111.2±5.9 | 106.6±5.46 |
This table shows increase in amplitude and decrease in latency of amblyopic eyes after treatment, while no change in fellow eyes.
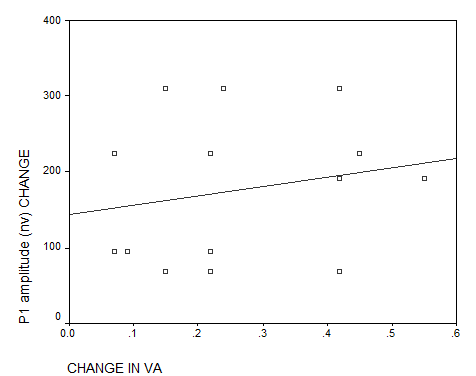
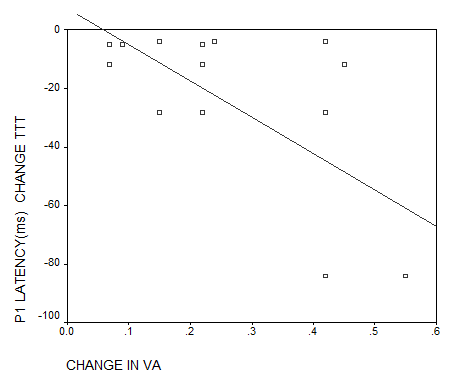
There was a weak positive correlation between visual acuity improvement in amblyopic eyes at the end of the follow up period with P100 amplitudes change of PVEP, and a strong negative correlation with P100 latencies change (figures 3, 4).
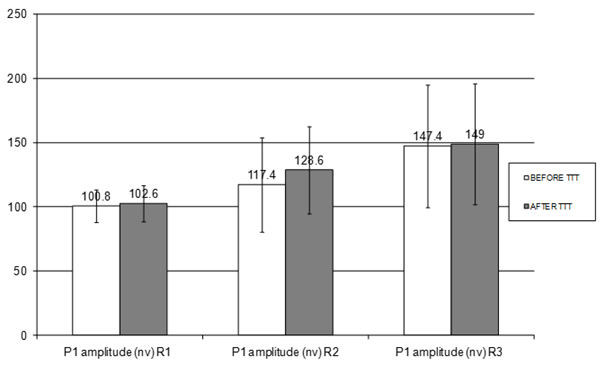
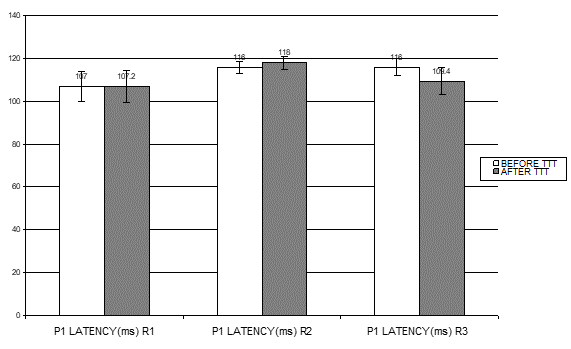
Regarding mfVEP records, P1 amplitudes, along the three studied rings showed statistically significant difference with (p = 0.001, 0.001. 0.01) respectively between the amblyopic eyes and the fellow eyes. There was statistically significant difference between. P1 amplitudes along the second and third studied rings before and after treatment at the end of follow up period, MFVEP amplitudes increased in rings 2 and 3, while the first ring which corresponds to the most central part of visual field (central 3°) showed no change (figure 5). There were no changes in latencies before and after treatment in central ring with minimal reduction of latencies of rings 2 and 3 as shown in (figure 6, table 3).
Table 3: MFVEP Changes of latencies in amblyopic eyes before and after treatment.
This table shows no significant reduction in latencies after treatment
| Latency | Mean | Std. Deviation |
| P1 latency(ms) R1 before treatment | 117.0000 | 6.92820 |
| P1 latency(ms) R1 after treatment | 117.2000 | 7.44696 |
| P1 latency(ms) R2 before treatment | 116.0000 | 2.77746 |
| P1 latency(ms) R2 after treatment | 118.0000 | 3.13961 |
| P1 latency(ms) R3 before treatment | 116.0000 | 3.87298 |
| p1 latency(ms) R3 after treatment | 109.4000 | 6.23126 |
| P | 0.75 |
Figure 1: pVEP, P100 amplitudes and latencies along treatment and follow up period. At 6 weeks pVEP recordings improved significantly with (P≤0.05). pVEP recordings showed stability tell the end of follow up period (P≥0.05). The fellow eye showed no change, amblyopic eye showed increased amplitude (p=0.0001) and decreased latency (P=0.005).
F: fellow eye, A: amblyopic eye. Unit of latency is ms(milli-second), and unit of amplitude is nv (nano-volt).
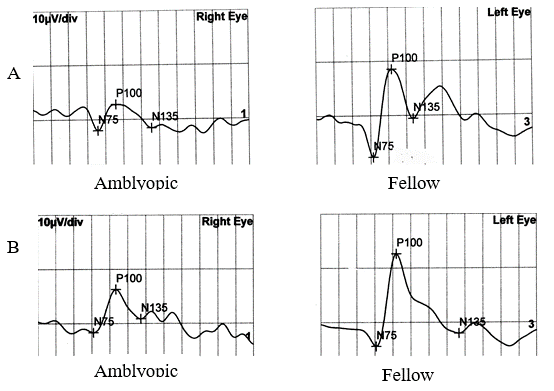
Figure 2: pVEP of both amblyopic and fellow eyes, A: before treatment. B: after treatment. There is improvement of latency and increase of amplitude in amblyopic eyes after treatment, while there are no changes in the fellow eyes.
Figure 3: correlation between changes of visual acuity in amblyopic eyes and P100 mplitudes change of pVEP. (p=0.45), VA: Visual Acuity, nv: nano-volt.
Figure 4: correlation between changes of visual acuity in amblyopic eyes and P100 latencies change of pVEP, (p=0.01), VA: Visual Acuity, ms: milli-second
Figure 5: MFVEP, P1 amplitudes along the three studied rings before and after treatment of the amblyopic eyes at the end of follow up period, showed an increase of amplitudes in amblyopic eyes after treatment in R 2 and minimal increase in R 3 but no increase in R1 (p= 0.49, 0.001, 0.001 respectively).
R1: first studied ring, R2: second studied ring and R3: third studied ring.
Figure 6: MFVEP, P1 latency along the three studied rings before and after treatment of the amblyopic eyes at the end of follow up period, showed no change in latencies after treatment in R1, minimal changes in R2 and R3.
R1: first studied ring, R2: second studied ring and R3: third studied ring.
Discussion
This study shows that improvement and stabilization of visual acuity in adult amblyopia is possible, this is confirmed by VEP changes. Adults’ amblyopia can improve and there is no clear upper age limit for recovery of acuity [10].
In this study, combined lines of treatment of adult amblyopia were used, with excellent compliance and good visual performance resulted in satisfactory results of improved visual acuity in all patients.
Clinical trials have suggested that patching 6 hours per day may be effective in older patients. Also, adults capable of improving performance on sensory tasks or perceptual learning and this considered to be a form of neural plasticity that exist in amblyopia due to anisometropia or strabismus [11,12]. Levodopa is an additional line of treatment of amblyopia. It was reported a slight increase in contrast sensitivity, visual acuity and amplitude of pattern visual evoked potential after single dose administration. Another recent study showed that longitudinal dosing of Levodopa and part-time occlusion yielded long-term improvement in visual acuity [6,13].
As most of our patients were old children and young adults (mean was 19.8 ± 4.5), Levodopa was used for a longer duration (6 weeks), Gottlob et al. reported more frequent improvement of visual acuity due to an administration period of one week, also they suggested that patients under 12 years are more susceptible to Levodopa than older patients, so a higher dose and a longer duration may be used in older patients [14]. However, the duration of Levodopa administration was variable in many studies ranging from a one single dose, divided doses for one week, for 3 weeks, 5 weeks up to 7 weeks [15-18]. So, the decision was taken to continue on the drug administration till stabilization of visual acuity occurred, this was achieved between the 5th and 6th weeks, so, the drug administration was stopped at the end of the 6th week.
Significant improvement of visual acuity at the end of 6 weeks might be due to Levodopa facilitates patient compliance to occlusion therapy and training, and enhances the neural plasticity that may last up to 9 weeks after stopping treatment as previously reported [19].
In this study combined therapy was performed to achieve maximum improvement of visual acuity, so, after stoppage of Levodopa, the same occlusion and visual training were continued for another 6 weeks.
This was to maintain improved visual acuity and avoid any regression. This achieved more stabilization with minimal improvement of visual acuity in some cases. Persistent visual acuity improvement might be due to persistent effect of Levodopa, or increased in the brain volume of activation, that approved by functional magnetic resonance which enhanced by occlusion [20.21].
Conclusion
For a successful treatment of amblyopia and to avoid regression of improved visual acuity, gradual reduction of occlusion time one hour weekly for 6 weeks was performed [22]. This was achieved in our results. However, there is no guarantee that amblyopia will not recur, which emphasizes the importance of monitoring amblyopic patients for a longer duration up to years [23].
A number of studies have shown VEP in amblyopia to be abnormal. Yu, et al, found marked prolongation of latencies and reduction of amplitudes of MFVEP in anisometropic amblyopia in the central field more than peripheral field [8,9,24].
This study found an actual functional improvement in the studied eyes through improved VEP and MFVEP parameters. VEP changes in the amblyopic eyes showed stability along the follow up period. The clinical and functional improvement in the studied eyes support dormant neural plasticity theory in the adult amblyopic eye [25]. However, further studies of longer duration more than 6 weeks are needed to be decided if it is permanent changes or reversible ones.
References
- Barrett BT, Bradley A, McGraw PV. (2004). Understanding the neural basis of amblyopia. Neuroscientist. 10:106-117.
Publisher | Google Scholor - Mintz-Hittner HA, Fernandez KM. (2000). Successful amblyopia therapy initiated after age 7 years: compliance cures. Arch Ophthalmol. 118: 1535-1541.
Publisher | Google Scholor - Kiorpes L. (2006). Visual processing in amblyopia: animal studies. Strabismus. 14: 3-10.
Publisher | Google Scholor - Lonngi M, Velez FG, Tsui I, Davila JP, Rahimi M. (2017). Spectral domain optical coherence tomographic angiography in children with amblyopia. JAMA Ophthalmol 35: 1086-1091.
Publisher | Google Scholor - Liu CH, Ong SJ, Huang CY, Wu WC, Kao LY. (2018). Macular thicknes, foveal volume and choroidal thickness in amblyopic eyes and their relationships to the treatment outcome. J Ophthalmol 6: 1967621.
Publisher | Google Scholor - Borrelli E, Lonngi M, Balasubramanian S, Tepelus TC, Baghdasaryan E. (2018). Increased choriocapillaris vessel density in amblyopic children: a case-control study. J AAPOS 22:366-370.
Publisher | Google Scholor - Gaier ED, Gise R, Heidary G. (2019). Imaging Amblyopia: Insights from Optical Coherence Tomography (OCT). Semin Ophthalmol 34: 303-311.
Publisher | Google Scholor - Simon JW, Siegfried GB, Mills MD. (2004). A new visual evoked potential system for vision screening in infants and young children. JAAPOS. 86:549-554.
Publisher | Google Scholor - Hamurcu M, Çelik A, Sarıcaoğlu M, Bulut AK. (2017). Electrophysiologic evaluation of amblyopia. Eye Care Vis 1:1-4.
Publisher | Google Scholor - Hamurcu M, Ekinci C, Koca S, Tugcu B. (2021). Evaluation of amblyopic eyes with optical coherence tomography angiography and electrophysiological tests. Indian J ophthalmology. 69:105-110.
Publisher | Google Scholor - Zele AJ, Pokorny J, Levi DM, et al. (2007). Anisometropic Amblyopia Spatial Contrast Sensitivity Deficits in Inferred Magnocellular and Parvocellular Vision. Invest Ophthalmol Vis Sci. 48:3622-3631.
Publisher | Google Scholor - Pediatric Eye Disease Investigator Group. (2005). A randomized pilot study of near activities versus non- near activities during patching therapy for amblyopia. JAAPOS. 9:129-136.
Publisher | Google Scholor - Buonomano D V, Merzenicch M M. (1998). Cortical plasticity: form synapses to maps. Annu Rev Neurosci. 21:149-186.
Publisher | Google Scholor - Leguire L E, Komaromy K L, Nairus T M, et al. (2002). Long-term follow-up of L-dopa treatment in children with amblyopia. J Pediatr Ophthalmol Strabismus. 39:326-330.
Publisher | Google Scholor - Gottlob I, Charlier J, Reinecke R D. (1992). Visual acuity and scotomas after one week levodopa administration in human amblyopia. Invest Ophthalmol Vis Sci. 33:2722-2728.
Publisher | Google Scholor - Leguire L E, Rogers G L, Brewer D L. et al. (1982). Levodopa and childhood amblyopia. J Pediatr Ophthalmol Strabismus. 29:290-298.
Publisher | Google Scholor - Leguire LE, Rogers GL, Bremer DL, et al. (1993). Levodopa \ carbidopa for childhood amblyopia. Invest Ophthalmol Vis Sci. 34:3090-3095.
Publisher | Google Scholor - Leguire L E, Walson P D, Rogers G L, et al. (1995). Levodopa\ carbidopa treatment of amblyopia in older children. J Pediatr Ophthalmol Strabismus. 32:143-151.
Publisher | Google Scholor - Levartovsky S, Oliver M, Gottesman N, et al. (1995). Factors affecting the long-term results of successfully treated amblyopia. Br J Ophthalmol. 79:225-228.
Publisher | Google Scholor - Pandey P K, Chaudhuri Z, Kumar M, et al. (2002). Effect of levodopa and carpidopa in human amblyopia. J Pediatr Ophthalmol Strabismus. 39:81-89.
Publisher | Google Scholor - Yang CI, Yang ML, Huang JC, et al. (2003). Functional MRI of amblyopia before and after levodopa. Neurosci Lett. 339:49-52.
Publisher | Google Scholor - Rutstein RP, Fuhr PS. Efficacy and stability of amblyopia therapy. Optom Vis Sci 1992; 69:747-754.
Publisher | Google Scholor - Caloroso EE, Rouse MW. (1993). Clinical management of strabismus. Boston: Butterworth-Heinemann. 7:113-125.
Publisher | Google Scholor - Yu M, Brown B, Edwards MH. (1998). Investigation of multifocal visual evoked potentials in anisometropic and esotropic amblyopes. Invest Ophthalmol Vis Sci. 39:2033-2040.
Publisher | Google Scholor - Levi DM, Li RW. (2009). Improving the performance of the amblyopic visual system. Phil Trans R. Soc. 364:399-397.
Publisher | Google Scholor