Review Article
Visual Changes in Preeclampsia, Eclampsia and HELLP Syndrome
- Andri Teesalu *
- Maris Oll
Ophthalmologist, East Tallinn Central Hospital, Tallinn, Estonia.
*Corresponding Author: Andri Teesalu, Ophthalmologist, East Tallinn Central Hospital, Tallinn, Estonia.
Citation: Teesalu A, Oll M. (2024). Visual Changes in Preeclampsia, Eclampsia and HELLP Syndrome, Clinical Case Reports and Studies, BioRes Scientia Publishers. 7(3):1-11. DOI: 10.59657/2837-2565.brs.24.185
Copyright: © 2024 Andri Teesalu, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: September 12, 2024 | Accepted: September 27, 2024 | Published: October 18, 2024
Abstract
Preeclampsia, eclampsia, and HELLP syndrome (hemolysis, elevated liver enzymes, and thrombocytopenia syndrome) are pregnancy-related complications that occur before, during, or after childbirth and can be dangerous for both the mother and fetus.
The main diagnostic criterion for preeclampsia and eclampsia is hypertension and, in addition, the failure of an organ or organs caused by hypertension and vascular autoregulation. The pathology can manifest itself in varying degrees of severity in several organs, including the eyes and brain. Changes in the vision can also be the first and only complaint of preeclampsia.
The main symptom is a decrease in visual acuity. In the majority of patients, complaints resolve spontaneously and visual acuity recovers. Unfortunately, in rare cases, the disease can also end in blindness. Since preeclampsia can have a rapid course, manifesting within hours, timely diagnosis of ocular complications is important to ensure correct patient management.
This article provides an overview of the three most frequent eye and vision-related complications associated with preeclampsia, eclampsia and HELLP syndrome, their interrelationships, diagnostics and treatment. In addition, the case history is presented to characterize the course, management and treatment of an ocular complication in preeclampsia.
Keywords: central serous chorioretinopathy; cortical blindness; purtscher-like retinopathy; preeclampsia; eclampsia; HELLP
Introduction
Preeclampsia is a pregnancy-associated pathology, including hypertension and (multiple) organ failure, which starts after the 20th week of gestation. At the same time, the patient has not had these problems before pregnancy or in the early stages of pregnancy [1,2]. According to the previous classification, preeclampsia was diagnosed in the presence of hypertension (systolic blood pressure ≥140 mmHg and diastolic blood pressure ≥90 mmHg) and proteinuria (≥ 0.3 mg/mg urine protein to creatinine ratio). In the new classification, proteinuria has been replaced by the occurrence of organ failure [2]. It is the main complication during pregnancy, which occurs in an estimated 4-5% of pregnancies worldwide [2]. When ocular and cerebral complications appear, preeclampsia is immediately classified as severe [2]. Preeclampsia can also be accompanied by HELLP syndrome, which includes hemolysis, elevated liver alanine and aspartate aminotransferase (ALT and AST), and concomitant thrombocytopenia [3]. In the case of eclampsia, tonic-clonic seizures appear in addition to preeclampsia [2]. Change in vision can be a prodromal symptom in the development of the disease, and organ damage can occur after the development of hypertension [4]. Symptoms may include decreased visual acuity, double vision (diplopia), amaurosis fugax, visual field scotomas, and homonymous hemianopsia [4].
Complete vision loss is rare in preeclampsia, eclampsia, and HELLP syndrome, occurring in 1-3% of patients. Other visual symptoms occur in about 25% of patients with severe preeclampsia and as many as 50% of patients with eclampsia [5,6]. In addition to subjective symptoms, the most common finding on examination is marked spasm of fundus arterioles, occurring in 70% of patients with preeclampsia [6]. Retinal changes, such as central serous chorioretinopathy (CSC) and Purtscher-like retinopathy are ocular complications that reduce visual acuity and cause blindness. However, from extraocular causes, posterior reversible encephalopathy syndrome (PRES) and cortical blindness are the main causes for decreased visual acuity and blindness [4]. The most effective and only definitive treatment for preeclampsia, eclampsia and HELLP syndrome and related complications is delivery of the baby [2].
Central Serous Chorioretinopathy
Central Serous Chorioretinopathy (CSC) occurs in about 1% of patients with severe preeclampsia and in 10% of patients with eclampsia [4,5]. In CSC, the neurosensory part of the retina separates from the underlying tissues. The cause is believed to be systemic vascular regulation deficiency, which manifests in peripheral vasospasm and arterial blood circulation maladjustment [6]. In addition, there is a decreased response to vasoactive agents in preeclampsia [6]. Spasm of the arterioles causes ischemia of the choroid, resulting in impaired function of the retinal pigment epithelium (RPE) [7,8]. The role of the RPE is to transport water, salts, nutrients and metabolites between the choroid and the retina. In addition, RPE intercellular tight junctions form a barrier between blood and retina, which is damaged in the event of ischemia [4]. Subretinal swelling separates the RPE from the neurosensory retina and that causes visual complaints [6,7]. In the case of HELLP syndrome, the breakdown products resulting from hemolysis can also clog the capillaries and create an ischemic focus of the retina [7].
CSC has been observed before, during and after delivery [4,9]. In a retrospective multicenter study comparing the occurrence of CSC among patients with preeclampsia and malignant hypertension, it was found that among 29 patients with preeclampsia (53 eyes examined), CSC occurred in 9 patients during pregnancy (CSC was diagnosed in 16 eyes) and after delivery in 20 patients (CSC diagnosed in 37 eyes) [9]. There were 24 patients in the group with malignant hypertension (45 eyes were observed), and it was additionally found that the central thickness of the macula and choroid decreased more pronounced in the group with preeclampsia after CSC resolution compared to the malignant hypertension group [9]. The main symptoms in CSC are decreased visual acuity and visual field defects. Symptoms usually appear in both eyes at the same time, less often in one eye [4]. CSC does not rule out other vision-affecting conditions associated with preeclampsia, eclampsia, or HELLP syndrome, such as cerebral cortical edema [4].
The diagnosis of CSC is based on the symptoms and examination of the fundus [8]. When confirming the diagnosis, optical coherence tomography (OCT) is indicated as an additional examination, which allows visualization at the time of examination and the progression of CSC [8]. For an even more precise overview and evaluation of the dynamics both at the level of the retina and the choroid, an OCT angiography (OCT-A) study is recommended [9].
The previously mentioned study also looked at the visual acuity of patients with preeclampsia, in which the average logMAR was 0.24 ± 0.37 at the development of complaints [9]. During follow-up visit 1.83 ± 2.16 months later, visual acuity had improved to 0.11 ± 0.16 on the logMAR scale [9]. Visual acuity was below logMAR 0.3 in only 4 out of 53 eyes in the study group [9]. In addition, the risk factors for poor recovery of visual acuity are the presence of retinopathy and detachment of the retina in the macular area [9]. In most cases, vision returns to pre-CSC levels after fluid absorption and ocular treatment is not necessary [6]. On the other hand, it is not possible to predict the extent and development of CSC depending on the severity of preeclampsia, eclampsia or HELLP syndrome, as several different pathological processes occur simultaneously [7]. CSC caused by preeclampsia has a good prognosis for recovery, and the fluid resolves within 1-2 months after delivery [8]. Full recovery to the previous level of visual acuity occurs approximately 2-12 weeks after delivery [7].
Cortical Blindness
Cortical blindness is caused by posterior reversible encephalopathy syndrome (PRES) and includes cerebral edema, which is accompanied by acute neurological symptoms: convulsions, altered consciousness and visual disturbances [10]. Cortical blindness is a fairly common complication of preeclampsia and eclampsia, occurring in up to 15% of preeclamptic patients [11] and manifests both before and after childbirth (8). In the past, changes in vision due to preeclampsia and eclampsia were considered to be only ocular, mainly caused by the retina and choroid, but in the last 20-30 years PRES and cortical blindness have become more known, therefore their actual frequency may be higher [11,12].
In the case of cortical blindness, the autoregulation of blood vessels in the supply area of the posterior cerebral artery is affected [11] and blood vessels respond to a sudden increase in blood pressure with vasospasm [11,12]. According to the hypothesis, cytotoxic cerebral edema and ischemia occurs after this [11] and at a later stage, cerebral infarction is also possible [8,12]. According to the second theory, autoregulation of cerebral blood vessels decreases during a sudden increase in blood pressure, areas of vasoconstriction and dilatation are formed and vasogenic cerebral edema develops as a result of increased hydrostatic pressure, hyper perfusion, and extravasation of blood plasma and blood elements [8,11,12]. This theory is supported by the fact that the supply area of the posterior arteria cerebri is more sensitive to high blood pressure and the permeability of the brain-blood barrier is greater, because the supply area has less sympathetic innervation and less neurogenic regulation [10-12]. Cortical blindness is thus caused by swelling of the posterior part of the brain, involving the visual pathway and visual cortex, hence the name of the condition [4,12].
The main symptoms in cortical blindness are a progressive deterioration of visual acuity in both eyes: initially blurring of vision and then a decline over hours to hand movement, light perception [4] or blindness [13]. Blindness may be preceded by prodromal symptoms: nausea, vomiting and severe headache, most often in the frontal region [4,12]. Severe headache is the most common prodromal symptom, which may be a sign of vascular autoregulation loss [12]. Also, sudden loss of vision can be the first sign of eclampsia, requiring immediate medical attention [11,13]. In such cases, patients with preeclampsia experienced a complete loss of vision 4-7 hours before the onset of eclamptic seizures [11]. Therefore, pregnant women with sudden vision loss should be considered as potential eclamptic patients [8]. It is also important to distinguish cortical blindness and its accompanying symptoms from migraine, another cause of headache [14] and epilepsy [15]. Epilepsy occurs in 2/3 of patients with PRES, and in some cases, epilepsy may persist for a long period of time [15].
Cortical blindness does not affect the eye itself: there is no ocular pathology, pupillary reflexes and fundus examination is normal [16]. Swelling of the occipital part of the brain may not be the only reason for a decrease in visual acuity as the fundus changes described above in the article may also occur as a combination [11]. Since cortical blindness is caused by edema in the posterior part of the brain, computed tomography (CT) or magnetic resonance imaging (MRI) are appropriate to confirm the diagnosis [4,6,11,12]. The foci are hypodense on the CT scan and hyperdense on the T2-sequence MRI scan [6]. The T2-sequence MRI is considered to be more accurate than the CT scan, because in cases where the CT was without pathological findings, the MRI still showed changes [4]
Changes may not be limited to the parietal or occipital lobes, but may also occur in the frontal and temporal lobes or even in the brainstem [4,10]. Brainstem and cerebellar swelling occurred more frequently in patients with eclampsia [10]. In addition, magnetic resonance angiography (MRA) may be considered, as hemorrhagic complications have also been observed in PRES syndrome (10). The MRA study also shows diffuse vasospasm [8].
Laboratory tests monitor the levels of hematocrit (Hct), serum creatinine (S-Crea), aspartate aminotransferase (AST), alanine aminotransferase (ALT) and lactate dehydrogenase (LDH), as the values of these markers are significantly increased in PRES patients compared to those who did not have a pathological finding on MRI [10].
The prognosis of vision is good in PRES and cortical blindness, and the length of vision loss can vary from 4 hours to 8 days [11]. It is important to treat preeclampsia and eclampsia: lowering blood pressure and preventing seizures with magnesium sulfate [4]. Since blood pressure spikes are the main cause of vasogenic cerebral edema, controlling hypertension is extremely important [12]. The prognosis is worse if PRES and cortical blindness are accompanied by other ocular pathology, such as CSC or Purtscher-like retinopathy, which can cause permanent visual impairment and, in rare cases, blindness [4,8].
Purtscher-Like Retinopathy
Purtscher-like retinopathy is a pathology which results in variable deterioration or complete loss of vision in one or both eyes and is caused by trauma, acute pancreatitis, fat emboli, renal failure, connective tissue diseases, or childbirth [17]. The exact cause of postpartum Purtscher-like retinopathy is unknown, but it is thought that when amniotic fluid enters the mother's bloodstream, the complement system is activated and factor C5a causes the formation of emboli [18]. In previously described cases, a decrease in visual acuity or complete loss of vision has occurred after childbirth [18-21].
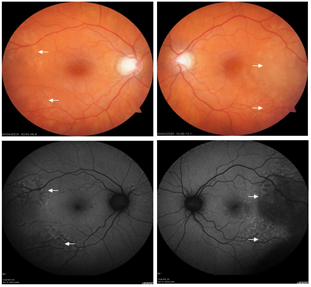
Purtscher-like retinopathy is a rare complication of preeclampsia that has been described in only a few cases [4]. Characteristic are Purtscher flecken on ophthalmoscopy - collections of soft exudates (cotton wool spots) around the optic disc and between arterioles and venules, retinal hemorrhages and papilledema (Figure 1) [17]. Purtscher-like retinopathy with serous retinal detachment, treated with corticosteroids, has been reported in some cases in preeclamptic patients [19,20]. However, treatment with corticosteroids has not shown a better outcome compared to watchful waiting [22].
Case Report
A 35-year-old female presented to the emergency room due to lower abdominal pain and irregular contractions that had lasted for several hours. It was a twin pregnancy (dichorionic and diamniotic) resulting from in vitro fertilization (IVF). Previously the patient had another IVF pregnancy without complications. The beginning of the pregnancy was normal, but from the 6th month a sudden weight gain of 5 kilograms per month was observed for two consecutive months. During a routine check-up, gestational age (GA) 33 weeks and 3 days (33+3), the patient was diagnosed with elevated blood pressure (repeated measurements of 160/85 mmHg and 140/80 mmHg) and treatment with labetalol (100 mg twice a day) was started. After one week (GA 34+3), the patient had a follow-up visit to examine fetal growth and the effect of labetalol treatment. During this visit, everything was as expected.
Next time the patient presented to the emergency room at 36 weeks and 0 days (36+0). The blood pressure values were 177/111 mmHg and later 147/105 mmHg. Overall, the patient was in a satisfactory general condition but complained of a headache. There were no visual disturbances. Cardiotocographic examination showed normal fetal heart activity and irregular uterine contractions. A further plan was established: urinalysis, blood analysis with preeclampsia markers, labetalol 100 mg three times per day. In addition, the first fetus was in breech position, so it was decided to terminate the pregnancy by caesarean section when labor began. In urinalysis, the patient had a highly elevated protein to creatinine ratio of 8.647 mg/mg (reference value <0>
The patient had a history of one miscarriage, one ectopic pregnancy that ended with a laparoscopic right salpingectomy and one in vitro fertilization (IVF) resulting in a pregnancy that proceeded normally and ended in spontaneous delivery (GA 37+1). In addition, the patient had been diagnosed with polycystic ovary syndrome (PCOS) and bilateral infertility. The patient had had no ophthalmic complaints in the past, and no procedures or operations done other than laser vision correction of both eyes (LASIK). The first visual complaints occurred on the day of admission to the hospital, 9 hours after the caesarean section. The patient noticed double vision when looking up close after waking up, but this resolved spontaneously after a few hours. The next morning, she complained that her distance vision had become blurred. This resolved by the evening of the same day. The next morning, however, distance vision had become blurry again, and patient saw spots in front of her eyes when the gaze was fixed. The patient did not have a headache in connection with visual disturbances. By the evening of the same day, the visual complaints had not subsided. In addition, the perception of straight lines as crooked when looking near had developed. An ophthalmologist’s consultation was planned for the next morning.
Ophthalmologist’s Consultation:
Best corrected visual acuity (BCVA) - Snellen
OD 0.8 -0.5 Dsph -0.5 Dcyl 155* = 1.0 (-1); OS 0.9
Intraocular pressure (IOP) OD 5 and OS 4 mmHg.
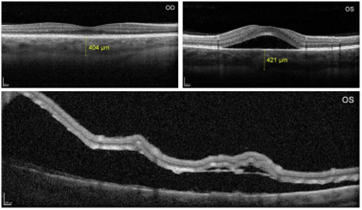
Examination showed no changes in the anterior segment. The optic nerve heads had a normal appearance and the arteries and veins were normal. However, there was serous detachment in the macular and temporal retinal areas (Figures 2 and 3). To clarify the diagnosis, OCT of the optic disc and macula (Photo 3A and B) and fundus autofluorescence (FAF) (Photo 2C and D) were done. Based on the clinical findings and OCT, the patient was diagnosed with CSC in both eyes due to preeclampsia. The patient was kept under observation and had an ophthalmologist’s follow-up appointment to evaluate the dynamics after a month. In total, the patient was hospitalized for 6 days, and on the day of discharge the visual acuity had subjectively improved. The blood pressure had also decreased to normal range with labetalol treatment, and the patient discharged.
Figure 2: Fundus images at the first ophthalmologist consultation. A and B. In the color fundus photography (CFP) of the right and left eye, the elevation of the neurosensory retina can be observed both as small foci and as a wide area. C and D. Fundus autofluorescence (FAF) imaging of the right and left eye shows hypo fluorescent areas characteristic of neurosensory retinal detachment.
Figure 3: OCT examination at the first consultation. A. The macular configuration is normal in the right eye, but there is choroidal thickening (404 µm, reference value 272 +/- 81 µm). B. A detachment of the neurosensory retina is visualized in the left eye of the macular area and thickening of the choroid (421 µm). C. An OCT image of the temporal periphery of the left eye shows extensive subretinal fluid, which is also present on the color photograph and autofluorescence image.
At the follow-up appointment 1 month later, the patient still complained of slight flickering in front of the left eye.
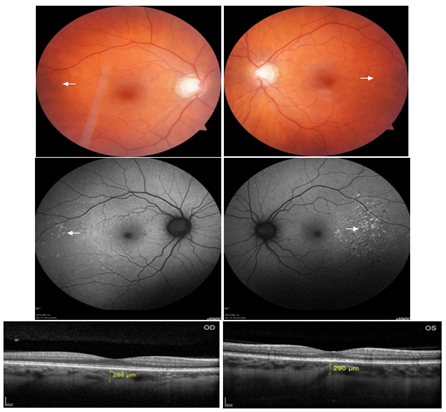
BCVA – Snellen; OD 0.9; OS 1.0.
Ophthalmoscopy showed small whitish-yellow foci temporal of the maculae in both eyes (Figure 4A and B), otherwise the peripheral retina was normal, as were the optic nerve heads and maculae of both eyes. The extensive detachment of the neurosensory retina in the temporal part of the left eye had regressed (Figure 4B). Fundus autofluorescence showed hyperfluorescent well-defined foci in both eyes (Figure 4C and D), and the OCT of the macula of both eyes was normal (Figure 4E and F). Based on findings the central serous chorioretinopathy had started resolving and the patient came back for a check-up after a month. By then the pathologic changes had subsided and visual acuity had fully recovered.
Figure 4: Fundus examinations performed one month after the first visit. A and B. CFP shows small yellowish-white foci are visualized temporal of the maculae. C and D. Corresponding foci on CFP are hyperfluorescent areas on FAF. E and F. On the OCT, the CSC had subsided and the choroidal thickness was normal.
This case report illustrates the CSC occurring with preeclampsia, which requires treatment for preeclampsia, but not active ophthalmic treatment. The vision recovered fully.
Conclusion
Visual changes due to pre-eclampsia, eclampsia and HELLP syndrome can be a predictive symptom of pre-eclampsia or eclampsia, but the symptoms can also appear later, after the hypertensive disorder has developed. Ocular complications with more serious consequences include Purtscher-like retinopathy, in which visual acuity will not reach the initial level. In contrast, both CSC and cortical blindness will usually not result in permanent vision loss or blindness, and complete recovery of visual acuity occurs in the majority of patients. Active treatment has not proven better than watchful waiting, so regular monitoring of disease progression is necessary. Although ocular complications occur less often in preeclampsia, eclampsia and HELLP syndrome than some other organ failures, prompt diagnosis is very important to ensure the necessary medical care and the best outcome for the mother and fetus.
Declarations
Acknowledgment
We thank Dr. Mall Parik for the cooperation.
Authors' Declaration of Potential Conflict of Interest
The authors confirm that they have no conflict of interest in relation to the article.
References
- Rana S, Lemoine E, Granger J, Karumanchi SA. (2019). Preeclampsia: Pathophysiology, Challenges, And Perspectives. Circ Res, 124:1094-1112.
Publisher | Google Scholor - Phipps EA, Thadhani R, Benzing T, Karumanchi SA. (2019). Pre-Eclampsia: Pathogenesis, Novel Diagnostics and Therapies. Nat Rev Nephrol, 15:275-289.
Publisher | Google Scholor - Wallace K, Harris S, Addison A, Bean C. (2018). HELLP Syndrome: Pathophysiology and Current Therapies. Curr Pharm Biotechnol, 19:816-826.
Publisher | Google Scholor - Roos NM, Wiegman MJ, Jansonius NM, Zeeman GG. (2012). Visual Disturbances In (Pre)Eclampsia. Obstet Gynecol Surv, 67:242-250.
Publisher | Google Scholor - Alizadeh Ghavidel L, Mousavi F, Bagheri M, Asghari S. (2018). Preeclampsia Induced Ocular Change. Int J Women’s Health Reprod Sci, 6:123-126.
Publisher | Google Scholor - Abu Samra K. (2013). The Eye and Visual System in The Preeclampsia/Eclampsia Syndrome: What to Expect? Saudi J Ophthalmol, 27:51-53.
Publisher | Google Scholor - Vigil-De Gracia P, Ortega-Paz L. (2011). Retinal Detachment in Association with Pre-Eclampsia, Eclampsia, And HELLP Syndrome. Int J Gynecol Obstet, 144:223-225.
Publisher | Google Scholor - Schultz KL, Birnbaum AD, Goldstein DA. (2005). Ocular Disease in Pregnancy. Curr Opin Ophthalmol, 16:308-314.
Publisher | Google Scholor - Lee CS, Choi EY, Lee M, Kim H, Chung H. (2019). Serous Retinal Detachment in Preeclampsia and Malignant Hypertension. Eye, 33:1707-1714.
Publisher | Google Scholor - Mayama M, Uno K, Tano S, Yoshihara M, Ukai M, et al. (2016). Incidence of Posterior Reversible Encephalopathy Syndrome in Eclamptic and Patients with Preeclampsia with Neurologic Symptoms. Am J Obstet Gynecol, 215.
Publisher | Google Scholor - Cunningham FG, Hernandez C. (1995). Blindness Associated with Preeclampsia and Eclampsia. Am J Obstet Gynecol, 172:1291-1298.
Publisher | Google Scholor - Zeeman GG. (2009). Neurologic Complications of Pre-Eclampsia. Semin Perinatol, 33:166-172.
Publisher | Google Scholor - Llovera I, Roit Z, Johnson A, Sherman L. (2005). Cortical Blindness, A Rare Complication of Pre-Eclampsia. J Emerg Med, 29:295-297.
Publisher | Google Scholor - Negro A, Delaruelle Z, Ivanova TA, Khan S, Ornello R, et al. (2017). Headache And Pregnancy: A Systematic Review. J Headache Pain, 18:106.
Publisher | Google Scholor - Fischer M, Schmutzhard E. (2017). Posterior Reversible Encephalopathy Syndrome. J Neurol, 264:1608-1616.
Publisher | Google Scholor - Mccormick AS, Wood A, Wee MY. (1999). Visual Disturbances and Seizures Associated with Pregnancy: A Diagnostic Dilemma and The Role of Radiological Techniques as An Aid to Diagnosis. Int J Obstet Anesth, 8:184-188.
Publisher | Google Scholor - Agrawal A, Mckibbin MA. (2006). Purtscher’s and Purtscher-Like Retinopathies: A Review. Surv Ophthalmol, 51:129-136.
Publisher | Google Scholor - Blodi BA, Johnson MW, Gass JDM, Fine SL, Joffe LM. (1990). Purtscher’s-Like Retinopathy After Childbirth. Ophthalmology, 97:1654-1659.
Publisher | Google Scholor - Erol YO, Inanc M. (2018). Purtscher-Like Retinopathy with Serous Macular Detachment in Pre-Eclampsia. Oxf Med Case Reports, 11:357-358.
Publisher | Google Scholor - Shukla D, Maheshwari R, Ramchandani B, Kanungo S. (2010). Purtscher-Like Retinopathy with Serous Retinal Detachment in Preeclampsia of Pregnancy: Complications and Management. Retin Cases Brief Rep, 4:332-335.
Publisher | Google Scholor - Singh K, Jain D, Wallang B. (2014). Purtscher’s Retinopathy in Pre-Eclampsia: A Blinding Combination. Int Ophthalmol, 34:103-106.
Publisher | Google Scholor - Xia D, Chen X, Zhou Q, Xiao S, Yu Y, et al. (2017). Efficacy of Purtscher’s Retinopathy Treatments: A Systematic Review. Curr Eye Res, 42:908-917.
Publisher | Google Scholor - Errera MH, Kohly RP, Da Cruz L. (2013). Pregnancy-Associated Retinal Diseases and Their Management. Surv Ophthalmol, 58:127-142.
Publisher | Google Scholor