Case Report
Villamentous Cord Insertion: A Case Report
- Yismaw Yimam *
- Addisu Alem Negatu
College of Medicine and Health Sciences, Debere Tabor University, Debre Tabor, Ethiopia.
*Corresponding Author: Yismaw Yimam, College of Medicine and Health Sciences, Debere Tabor University, Debre Tabor, Ethiopia.
Citation: Yimam Y, Addisu A. Negatu. (2024). Villamentous Cord Insertion: A Case Report. Journal of Women Health Care and Gynecology, BioRes Scientia Publishers. 3(6):1-3. DOI: 10.59657/2993-0871.brs.24.047
Copyright: © 2024 Yismaw Yimam, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: May 25, 2024 | Accepted: June 24, 2024 | Published: July 08, 2024
Abstract
Introduction: A velamentous cord insertion occurs when the umbilical cords Wharton jelly fails to reach the placenta, due to early placental atrophy around the insertion site, leaving a segment of unprotected vessels running through the thin membranes of the amniotic sac. This area of weakness exposes a threat to the well-being of the fetus through acute hemorrhage and both acute and chronic restriction.
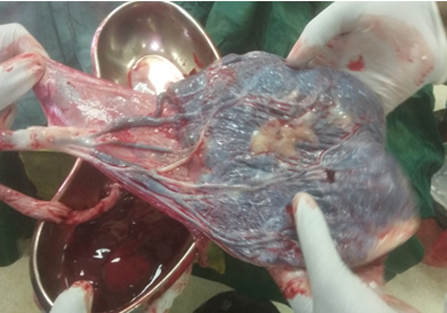
Case presentation: A 24-year-old para-1 Ethiopian woman came to our hospital with a complaint of pushing down pain and passage of liquor of 1-hour duration. She was referred from local health center with diagnosis of cord prolapse. Immediately, C/S was done to effect delivery of 3.2-kilogram male neonate with APGAR score of 9 and 10. Gross examination of placenta showed cord vessel was divided away from placenta run through the membrane.
Conclusion: There is a correlation between aberrant cord insertions and a higher incidence of abnormal FHR tracings and cesarean deliveries. Specifically, a VCI should be considered a high-risk pregnancy and a warning indication of a potential vasa previa. Even though this case had a positive outcome, it serves to emphasize how crucial it is to diagnose a VCI early in pregnancy. and perhaps enhance obstetric care.
Keywords: velamentous cord insertion; cord prolapse
Introduction
The placenta, membranes and umbilical cord constitute essential elements for normal development of the pregnancy. Altered development of any of these constituents may result in adverse outcome for the fetus and the mother. In pregnancies with anomalous cord insertion (velamentous (VCI) or marginal (MCI)) the risks of preeclampsia, abruption of the placenta, placenta previa, fetal growth restriction, preterm birth and fetal death are increased, as well as the risk of maternal complications in the third stage of labor [1]. Velamentous and marginal cord insertions occur in 1 and 6.3% of all singleton pregnancies, respectively, with both conditions being associated branes and from there traverse unprotected (by Wharton’s jelly) to reach the placenta. A marginal cord insertion (i.e., less than 2.5 cm from the placental edge) has a scanty placental tissue support. Vessels are also termed velamentous when they run in the chorioamniotic membranes between parts of bi-lobate placentas or link with a bi-placenta. In pregnancies with velamentous cord insertion the perinatal mortality at term is tripled, and anomalous cord insertion is associated with increased risks for preeclampsia, placenta previa and placental abruption. Various risk factors for anomalous cord insertions have been identified, and targeted ultrasound examination of the cord insertion, which is feasible, has been suggested as a method of improving perinatal care with an increased risk of adverse pregnancy outcome [2].
Presentation of the Case
A 24-year-old prim gravida whose gestational age from LNMP was 39+4 weeks admitted to our hospital (FHCSH,Bahir dar, Ethiopia) on the 15th of december,2018 being referred from one of the surrounding health center after she presented with pushing down pain and passage of liquor of half hour duration . she had regular antenatal care at local health center, uneventful. She took TT vaccine and supplemented with iron for four months. She appreciate fetal movements as usual.She has no headache ,blurring of vision and epigastric pain . She has no personal or family history of any known chronic illness. Pregnancy was planned, wanted and supported. On presentation, her vital signs were normal. her weight was 56 Kg, on abdomen, term sized gravid uterus, longitudinal lie, cephalic presentation, has contraction, FHB was128 BPM. On inspection of external genitalia; there was a cord protrude per vagina, with active leakage of liquor. Upon digital vaginal examination, cord was pulsatile cervix was 3 cm vertex station high, cord was anterior. Cord was inserted to vagina, she was put on Trendelenburg position, taken to Operation theatre, under general anesthesia, lower uterine segment transverse C/S done, to effect delivery of male alive neonate with APGAR score of 9 and 10. placenta and membrane delivered by steady cord traction, cord has three vessels. It was examined, found that umbilical vessels divided ,13 cm away from placenta margin and runs through the membrane, un ruptured as shown in the(figures.) below. The lab investigation result showed normal. Mother and new born discharged well after 3 days.
Figure 1
Figure 2
Discussion
A velamentous insertion is a variant of considerable clinical importance. The umbilical vessels characteristically spread within the membranes at a distance from the placental margin, which they reach surrounded only by a fold of amnion. As a result, vessels are vulnerable to compression, which may lead to fetal hypo perfusion and acidemia. The incidence of velamentous insertion is approximately 1 percent, but it is more commonly seen with placenta Previa and multifetal gestations. When seen during prenatal sonography, cord vessels with velamentous insertion are seen traveling along the uterine wall before entering the placental disc [3]. The fact that prenatal diagnosis of the placental anomalies and of the mechanisms responsible for abnormal insertion of the umbilical cord are not known, but most probably these events are operative from the first trimester. One theory is trophotropism, in which the chorion frondosum or the early placenta “migrates” with advancing gestation to ensure a better blood supply from a more richly vascularized area [4].
Umbilical cord decreases the incidence of emergency C-section and of intrauterine fetal death with over 50%, the ultrasound exploratory demands should be increased by including rigid criteria addressed to the specific risk categories of patients. In the context in which the safety of giving birth to a child is a major objective of prenatal examination, both transvaginal and Doppler ultrasound examination of the cervix and umbilical cord placental insertion represent key elements for diagnosis of life [5]. To conclude, anomalous cord insertion was associated with a doubled risk of PROM and spontaneous preterm birth, and almost tripled risk of prom. The development of anomalous cord insertion and short cord length seem to have a common pathophysiology. The trend of spontaneous preterm birth and anomalous cord insertion was declining [1]. About one-third of women with VCI had a preterm delivery and about one-quarter had an early preterm delivery. A 1.38fold to a twofold greater risk of preterm delivery in pregnancies with VCI has already been reported. The main reasons for early preterm delivery in the VCI group were PROM and premature labor. Only one patient was delivered by acute Cesarean section, due to the combination of vasa Previa and PROM. It is difficult to comment on the obvious association of VCI with preterm PROM and premature labor. Previous reports did not list the causes for preterm delivery in pregnancies with VCI in detail, an association that has been reported previously [6].
References
- Ebbing C, Johnsen SL, Albrechtsen S, Sunde ID, Vekseth C, Rasmussen S. (2017). Velamentous or marginal cord insertion and the risk of spontaneous preterm birth, prelabor rupture of the membranes, and anomalous cord length, a population-based study. Acta obstetricia et gynecologica Scandinavica, 96(1):78-85.
Publisher | Google Scholor - Ebbing C, Kiserud T, Johnsen SL, Albrechtsen S, Rasmussen S. (2015). Third stage of labor risks in velamentous and marginal cord insertion: a population-based study. Acta obstetricia et gynecologica Scandinavica, 94(8):878-83.
Publisher | Google Scholor - (2014). Williams Obstetrics 24th Ed.
Publisher | Google Scholor - Velamentous Cord Insertion in a Singleton Pregnancy.
Publisher | Google Scholor - Rocha J, Carvalho J, Costa F, Meireles I, do Carmo O. (2012). Velamentous cord insertion in a singleton pregnancy: an obscure cause of emergency cesarean-a case report. Case reports in obstetrics and gynecology, 2012:308206.
Publisher | Google Scholor - Yerlikaya G, Pils S, Springer S, Chalubinski K, Ott J. (2016). Velamentous cord insertion as a risk factor for obstetric outcome: a retrospective case-control study. Archives of gynecology and obstetrics, 293(5):975-981.
Publisher | Google Scholor