Case Report
Varied Manifestations of Artery of Percheron Stroke: A Clinical Case Series
- Rakshand Shetty *
- Madhu
- Udit Umrani
SDM College of Medical Sciences and College, Karnataka, India.
*Corresponding Author: Rakshand Shetty, SDM College of Medical Sciences and College, Karnataka, India.
Citation: Shetty R., Madhu, Umrani U. (2024). Varied Manifestations of Artery of Percheron Stroke: A Clinical Case Series, Clinical Case Reports and Studies, BioRes Scientia Publishers. 7(2):1-11. DOI: 10.59657/2837-2565.brs.24.175
Copyright: © 2024 Messay Gebrekidan, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: August 07, 2024 | Accepted: September 25, 2024 | Published: October 01, 2024
Abstract
Artery of Percheron (AOP) stroke, a rare anatomical variant resulting in bilateral thalamic infarction, presents with diverse clinical manifestations. We present a case series of six patients, highlighting the variability in clinical presentation, diagnostic challenges, management strategies, and outcomes associated with this condition. Variants in stroke presentation include altered sensorium, involuntary movements, and respiratory compromise. Imaging findings reveal bilateral paramedian thalamic infarcts, often involving adjacent structures. Management involves multidisciplinary care with emphasis on early recognition, supportive measures, and tailored rehabilitation. Our series underscores the importance of considering AOP stroke in patients presenting with atypical neurological symptoms, facilitating prompt diagnosis and intervention.
Keywords: percheron; thalamic infarction; bilateral thalamus; paramedian thalami
Introduction
Artery of Percheron stroke, characterized by occlusion of a single common arterial supply to the bilateral thalami and other adjacent structures, is a rare but clinically significant entity. The anatomical variability predisposes to a wide spectrum of neurological deficits ranging from altered consciousness to focal neurological signs, posing diagnostic challenges often requiring advanced neuroimaging and multidisciplinary management.
Materials and Methods
We conducted a retrospective review of six cases diagnosed with AOP stroke at our tertiary care facility between 2017 and 2021. Clinical data including demographics, presenting symptoms, physical examination findings, diagnostic imaging (CT, MRI, and angiography), laboratory investigations, treatment modalities, and outcomes were analyzed. Diagnostic criteria included characteristic neuroimaging findings confirming bilateral paramedian thalamic infarction consistent with AOP involvement.
Case 1
A 72-year-old woman with a history of hypertension presented to the emergency department with fever and four episodes of involuntary limb movements lasting 4 to 6 hours, during which she remained unconscious. After initial assessment at a primary healthcare center, she was transferred to our tertiary care facility.
On admission, vital signs were stable, but she exhibited altered sensorium with a Glasgow Coma Scale (GCS) score of 8/15 (E2 V2 M4). Lumbar puncture yielded normal cerebrospinal fluid (CSF) results. Neurological examination revealed elicited reflexes, reduced power in both upper and lower limbs, and sluggishly reactive bilateral pupils (2-3mm on the right, 3-4mm on the left). Bilateral lung crepitations were noted on auscultation. A 9-lead electrocardiogram showed no abnormalities.
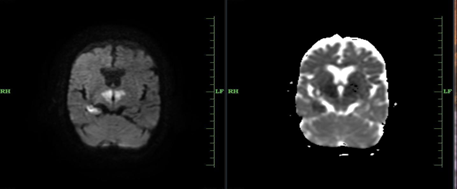
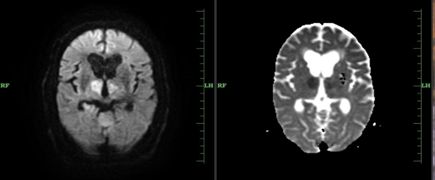
High-resolution CT brain imaging performed 20 minutes post-admission revealed ill-defined hypodense areas in the bilateral medial aspect of the pons. Subsequent MRI brain imaging showed bilateral symmetrical areas of altered signal intensity: hypointense on T2-weighted and FLAIR images, and hypointense on T1-weighted images with restricted diffusion, involving the bilateral basal ganglia, paramedian thalami, and right temporal lobe. Neurology consultation initiated anti-edema and antiepileptic medications. EEG findings indicated mild abnormal activity.
During hospitalization, the patient experienced one episode of focal seizure with nystagmus. A follow-up CT brain scan revealed persistent ill-defined hypodense areas in the right thalamic and temporal regions, with focal gliotic changes noted in the right cerebellar lobe and left thalamus. Detailed neurological examination identified downward gaze palsy. The patient clinically improved, achieving a Glasgow Coma Score of 14/15 (E4V4M6). Despite recommendations for a CT angiogram to localize the pathology related to the artery of Percheron (AOP), financial constraints led to the declination of this investigation. Consequently, the patient chose to discharge against medical advice on June 17, 2021, following admission on June 6, 2021.
Figure 1: Bilateral symmetrical areas of altered signal intensity involving the bilateral basal ganglia, paramedian thalami, and right temporal lobe.
Case 2
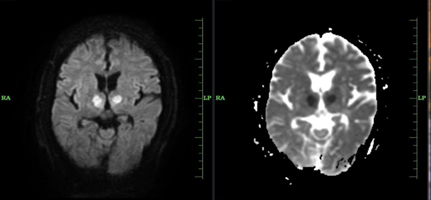
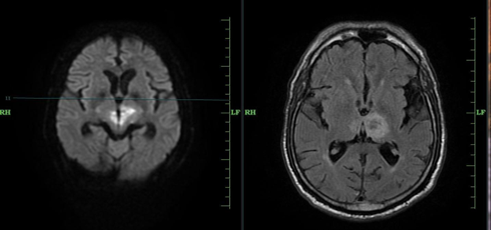
A 65-year-old retired army veteran, with a history of alcohol cessation six months prior, presented to the emergency department due to four hours of unresponsiveness despite preserved limb movement and a four-day history of headaches. He had a longstanding medical history of diabetes mellitus and hypertension under medical management. On admission, the patient required invasive mechanical ventilation with a Glasgow Coma Scale of 6 (E1 V1 M4). Neurological examination revealed diminished reflexes and sluggishly reactive bilateral pupils (2-3mm on the right, 3-4mm on the left), accompanied by bilateral lung crepitations on auscultation. Initial investigations included computed tomography (CT) and magnetic resonance imaging (MRI), which demonstrated bilateral symmetrical areas of altered signal intensity affecting the paramedian thalami, cerebral peduncles, and midbrain. Despite initial management, including supportive care and antibiotic treatment for unexplained fever spikes during hospitalization, all microbiological cultures returned negative, and routine blood tests remained within normal limits. The patient showed gradual clinical improvement, reflected in an improved Glasgow Coma Scale of 12/15 (E4 V2 M6), leading to his discharge on prescribed medications. Subsequently, he was referred to the neurology department for further evaluation. Date of admission: May 9, 2020; Date of discharge: May 28, 2020.
Figure 2: Bilateral symmetrical areas of altered signal intensity involving bilateral paramedian thalami extending into cerebral peduncles and anterior aspect of midbrain.
Case 3
A 71-year-old woman with a history of hypertension for three years, managed with medications, was brought to the emergency department in an unresponsive state with frothing at the mouth since 8 am, following sleep the previous night. She had been initially evaluated at a local hospital where a CT scan was performed (report unavailable) before referral to our facility for further management. There was no history of prior involuntary limb movements.
Upon arrival, her pulse was irregularly irregular at 106 beats per minute, with normal blood pressure and no fever detected. She presented with a Glasgow Coma Scale score of 6/15 (E1 V1 M4), necessitating invasive mechanical ventilation. Neurological examination revealed normal tone with un assessable power, decreased upper and lower limb reflexes, and flexor response on the right and withdrawal on the left on eliciting the plantar reflex. Bilateral pupils were sluggishly reactive, measuring 2-3mm on the right and 3-4mm on the left. Bilateral lung crepitations were auscultated. An electrocardiogram showed fibrillatory waves, consistent with atrial fibrillation. Transthoracic echocardiography revealed atrial fibrillation with rapid ventricular response, dilated left atrium, trivial aortic regurgitation, and grade 2 tricuspid regurgitation with moderate pulmonary artery hypertension. Lumbar puncture for cerebrospinal fluid analysis ruled out viral encephalitis, showing normal results.
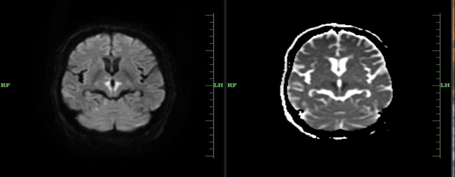
MRI brain imaging demonstrated acute infarcts involving bilateral thalamic regions, midbrain, and the right cerebellar hemisphere. Consultations with cardiology and neurology teams led to the initiation of appropriate medical therapies.
Due to financial constraints and prolonged intensive care unit needs, the patient opted for discharge against medical advice on January 15, 2019, following admission on January 7, 2019.
Figure 3: Acute infarcts noted involving bilateral thalamic regions, mid brain and right cerebellar hemisphere.
Case 4
A 28-year-old postpartum woman, with a history of pregnancy-induced hypertension managed with medications, underwent lower segment Cesarean section on March 3, 2019. She also had a history of hypothyroidism for two years, with discontinued medications. The patient presented with sudden-onset slurring of speech, progressive in nature since 2:30 pm on March 21, 2019. She reported inability to eat or drink, right-sided mouth deviation, excessive sweating, and salivation since noon on the same day. There were no complaints of chest pain, blurred vision, fever, involuntary limb movements, or frothing at the mouth. Initially evaluated by a physician, she was referred to our tertiary care center for suspected cerebral venous thrombosis or posterior reversible encephalopathy syndrome.
On admission, her vital signs were stable with a pulse rate of 101 beats per minute (regular rhythm), blood pressure of 150/100 mmHg, respiratory rate of 18 cycles per minute, and body temperature of 98.4°F. Systemic examination revealed dysarthria with absent gag reflex. Plantar reflexes were flexor, and upper and lower limb reflexes were normal with normal tone and power.
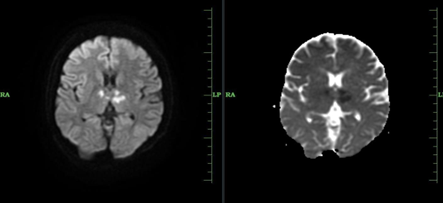
Diagnostic workup included a 9-lead electrocardiogram showing no abnormalities. CT brain imaging revealed an ill-defined hypodense area in the left thalamus region. Limited stroke screening MRI brain reported multifocal areas of acute infarcts in bilateral thalami and cerebellar hemispheres, suggestive of artery of Percheron involvement. Neurology consultation led to the initiation of appropriate medications. Ophthalmologic assessment via fundoscopy showed no evidence of retinopathy.
Transthoracic echocardiogram indicated trivial aortic or mitral regurgitation with a 60% ejection fraction. ANA profiling for autoimmune disorders returned negative. Carotid and vertebral artery Doppler ultrasound showed no abnormalities. MR angiogram revealed multifocal acute infarcts in bilateral thalami and cerebellar hemispheres, fetal origin of the right posterior cerebral artery, hypoplastic left vertebral artery, fetal origin of the right posterior cerebral artery, mild stenosis of the left posterior cerebral artery near its origin, absent/hypoplastic left anterior inferior cerebellar artery, and significant stenosis of the right superior cerebellar artery.
After a week of hospitalization, the patient improved symptomatically and was discharged on March 27, 2019, with a referral to the neurology department for further evaluation.
Figure 4: Multifocal areas of acute infarcts in bilateral thalami and cerebellar hemispheres.
Case 5
A 60-year-old male with a history of type 2 diabetes mellitus and hypertension for 4 to 5 years, as well as ischemic heart disease under medical management, presented to the emergency department at 5 pm on May 16, 2017, with a history of unresponsiveness since 2:30 pm on the same day. The event occurred while he was seated in a vehicle, leading to his immediate transfer to a local hospital and subsequent referral to our tertiary care center. Upon admission, on May 16, 2017, the patient was stuporous, with a right pupil dilated to 2-3mm and left pupil dilated to 4-5mm, both sluggishly reactive. Vital signs were stable, with a random blood sugar of 335 mg/dl. Neurological examination revealed increased tone in both upper and lower limbs, decreased reflexes bilaterally, and extensor plantar reflexes.
A 9-lead electrocardiogram showed no abnormalities. Due to a low Glasgow Coma Scale score, the patient required mechanical ventilation. MRI brain limited stroke screening, conducted on admission, revealed persistent areas of altered signal intensity: hyperintense on T2-weighted and FLAIR images, hyperintense on T1-weighted images, with mild restricted diffusion and areas of blooming on GRE images involving bilateral paramedian thalami and the left midbrain, suggestive of an artery of Percheron infarct. Neurology consultation was sought, and the patient was initiated on appropriate medications before transfer to the neurology ICU. Despite intensive care management, the patient showed no clinical improvement and experienced a protracted hospital course exceeding three months. Unfortunately, he succumbed to multiple comorbidities during this period, including aspiration pneumonia with septicemia, acute vertebra-basilar insufficiency with septicemia, and acute-on-chronic kidney disease, compounded by his longstanding type 2 diabetes mellitus and ischemic heart disease.
The patient was discharged on September 28, 2017, following a prolonged hospitalization period.
Figure 5: Persistent area of altered signal intensity of bilateral paramedian thalami and midbrain on left side.
Case 6
A 71-year-old male with a history of type 2 diabetes mellitus and hypertension for 12 years, as well as ischemic heart disease status post-coronary artery bypass grafting, presented to the casualty at 11:05 am on June 18, 2018, with sudden onset unresponsiveness since 5 am on the same day. One day prior, he was asymptomatic before developing altered sensorium, which was sudden and gradually progressive. There was no history of involuntary movements of limbs, head trauma, syncope, chest pain, or similar complaints in the past. He was initially managed at a local hospital in his village where his blood pressure was 150/100 mmHg and random blood sugar was 236 mg/dl. The patient also had a history of tobacco abuse and last consumed alcohol 15 years ago.
Upon examination on admission, his vital signs showed stable blood pressure of 150/100 mmHg and random blood sugar of 203 mg/dl. The Glasgow Coma Scale was 8/15 (E1 V2 M5). Bilateral emphysematous lung fields were noted on auscultation, and bilateral conducted sounds were heard. Neurologically, the patient was stuporous, localizing to painful stimuli, with deviation of the angle of the mouth to the left. There was decreased tone in the right upper and lower limbs, with decreased power (4/5) in these limbs. Plantar reflex was elicited on the right-side showing withdrawal and on the left side showing decreased reflex.
Initial evaluation with MDCT Brain revealed hypodense areas in bilateral thalami (left > right), consistent with acute infarcts. Further assessment with MRI Brain Screening demonstrated areas of altered signal intensity in the bilateral medial thalamic regions (left > right) and midbrain, appearing iso to hyperintense on T2-weighted and FLAIR images, and hypointense on T1-weighted images, indicative of restricted diffusion and ADC reversal. Additionally, areas of GRE blooming were noted within the left thalamus with T1 iso intensity and T2/FLAIR hypo intensity.
The patient was promptly transferred to the medical intensive care unit for ongoing management. Despite efforts, cardiopulmonary resuscitation initiated at 7:40 am on June 21, 2018, for 30 minutes failed to revive the patient, and he was pronounced dead at 8:15 am.
Cause of death was attributed to acute coronary syndrome in the setting of ischemic heart disease with an ejection fraction of 30%, compounded by bilateral thalamic and midbrain infarcts.
Figure 6: Altered signal intensities noted in bilateral medial thalamic region (left>right) and midbrain.
Results
All six patients presented with acute onset neurological deficits consistent with AOP stroke. Clinical manifestations ranged from altered sensorium, involuntary movements, to respiratory compromise. Neuroimaging demonstrated bilateral paramedian thalamic infarcts in conjunction with involvement of adjacent brain structures in all cases. Management strategies encompassed acute medical stabilization, neuroprotective measures, and rehabilitation. Despite varied presentations, clinical outcomes were generally favorable in terms of neurological recovery, though mortality was observed in one case.
Conclusion
Our case series underscores the diagnostic complexity and diverse clinical presentations associated with AOP stroke. Early recognition facilitated by characteristic imaging findings is crucial for prompt intervention and optimizing outcomes. Multidisciplinary collaboration involving neurology, neuroradiology, and intensive care teams is essential for comprehensive management. Further studies are warranted to elucidate optimal treatment strategies and long-term prognostic factors in this rare stroke variant.
Declarations
Source(s) of Support
We did not receive any support in the form of grants, equipment, drugs, etc. from any individual or organization.
Acknowledgements
None.
Consent
Written Informed consent was taken from the Patient’s legal guardian from the family presented at the Emergency. For retrospective cases, medical records from past patients who received similar imaging and management are reviewed with approval from the hospital administration.
Conflict of Interest
Authors declare no conflict of interest for this article. The manuscript has been read and approved by all the authors, the requirements for authorship as stated earlier in this document have been met, and each author believes that the manuscript represents honest work.
Data Availability
No additional data is available for this case series.
References
- Liang F, Alsherbini K, Tauheed S, et al. (2023). Artery of Percheron Infarction: A Comprehensive Review. J Stroke Cerebrovasc Dis. 32(4):106078.
Publisher | Google Scholor - Lazzaro NA, Wright B, Castillo M, Fischbein NJ, Glastonbury CM, et al. (2010). Artery of Percheron Infarction: Imaging Patterns and Clinical Spectrum. Am J Neuroradiol. 31(7):1283-1289.
Publisher | Google Scholor - Chang R, Friedman DP. (2013). Artery of Percheron Thrombolysis. Am J Neuroradiol. 34(4):847-850.
Publisher | Google Scholor