Research Article
Utilization And Predictors of Postpartum Modern Family Planning Methods in Felegehiwot Referral Hospital, Northwest Ethiopia
- Fisseha Moges *
- Semira Abdelmenan
- Belete Tafesse
Addis Continental Institute of Public Health, Addis Ababa, Ethiopia.
*Corresponding Author: Fisseha Moges, Addis Continental Institute of Public Health, Addis Ababa, Ethiopia.
Citation: Moges F., Abdelmenan S., Tafesse B. (2024). Utilization And Predictors of Postpartum Modern Family Planning Methods in Felegehiwot Referral Hospital, Northwest Ethiopia. Journal of BioMed Research and Reports, BioRes Scientia Publishers. 5(3):1-9. DOI: 10.59657/2837-4681.brs.24.096
Copyright: © 2024 Fisseha Moges, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: June 26, 2024 | Accepted: July 20, 2024 | Published: August 03, 2024
Abstract
Achieving adequate spacing between pregnancies is a major pathway through which contraceptive practice can render benefits. Directing efforts to increase modern contraception among postpartum women could have a significant impact on increasing contraceptive prevalence rate and other health benefits. However, contraceptive use in the postpartum period is less emphasized by policymakers and program designers in Ethiopia. Therefore, information about the current utilization of modern contraceptives and its associated factors among postpartum women is needed to design strategies and improve service delivery practices in health institutions. The objective of the study is to assess the utilization and factors associated with modern contraceptives use among postpartum women in Felegehiwot referral hospital, Bahirdar city, Northwest Ethiopia. A facility-based cross-sectional study was employed from January 1-31, 2019 among postpartum women in Felegehiwot referral hospital. The data were collected through a face-to-face interview for 425 women who were attending basic maternal and child health services. Bivariable and multivariable logistic regression was employed to identify the association between the dependent variable, utilization of postpartum family planning, and the explanatory variables. The association was considered statistically significant when P-value was < 0.05. A total of 425 postpartum women participated in the study with a 100% response rate. Over half (53%) of women interviewed used modern contraceptives during the postpartum period. Women who are aware of PPFP during ANC and PNC visits (AOR, 16.99; 95% CI, 2.85 to 101.16); married (AOR 3.052; 95% CI, 1.644 to 5.667); and higher age (AOR, 5.825; 95%CI, 2.519 to 13.467) were more likely to use modern contraceptives in the postpartum period. However, educational status, parity, the spousal reaction for FP related discussions, and contraceptive education failed short of any statistically significant association with modern postpartum contraceptive use. The utilization of modern contraceptives in the postpartum period was found to be relatively lower. Proper counseling on available methods for postpartum women at different instances coupled with increasing contraceptive method mix, enhancing male engagement in family planning programs, and expanding contraceptive information during facility visits for antenatal and postnatal care using different media outlets are important measures to boost contraceptive use.
Keywords: postpartum; modern family planning; predictors; Ethiopia
Introduction
Ethiopia is ranked 12th in population size having a total of 107.5 million people and a total fertility rate of 4.4 in 2018 (1). Improving family planning services is believed to be a key intervention for enlightening the health of women, men, and children. Contraceptive methods prevent unintended pregnancies, reduce the number of abortions, and lower incidence of death and disabilities related to complications of pregnancy and childbirth. In addition to its health benefits, Family Planning inadequacy, in developing countries, contributed significantly to poverty and ill health. Around $5.7 billion could be saved by avoiding unintended pregnancies and unsafe abortions through Family Planning (2). The provision of quality family planning service is recognized as a human right. Every individual has the right to access, choose, and benefit from scientific progress in the selection of those methods [3,4]. Through providing contraceptive options and satisfying unmet needs on contraceptives, it is possible to prevent 44% and 29% of maternal deaths every year [5]. Post-Partum Family Planning is defined as the prevention of unintended pregnancy and closely spaced pregnancies through the first 12 months following childbirth [6,7]. While there is a meaningful opportunity of reaching women in their postpartum period while either they give birth at the hospitals or come to health facilities accompanying their babies for immunization, evidence shows that these opportunities are missed by health care providers to provide appropriate information, counseling, and service on family planning during the postpartum period for reasons usually not sound scientifically [7].
Given the fact that providing comprehensive family planning counseling and proactively offering contraception from a range of choices as part of childbirth care prior to leaving the health facility is very crucial in averting maternal and child deaths, evidence shows that there is a missed opportunity of offering them with methods of their preference [7]. Achieving adequate spacing between pregnancies is a major pathway through which contraceptive practice can render benefits. Pregnancies conceived less than 20 months following a prior birth are at considerably higher risk of prematurity, low birth weight, fetal death, and early neonatal death. Studies revealed that children born within 24 months of their elder sibling have a 60% increased risk of dying before their first birthday and those born 2–3 years later have only a 10% increased risk, compared with those born after an interval of 3–5 years [8]. An analysis of Demographic and Health Survey data from 21 low- and midle-income countries between 2005 and 2012 revealed that almost all (95%) women 0-12 months postpartum wanted to avoid pregnancy in the following 24 months, but less than one-third (31%) were using any method of contraception and this indicates that 61% of postpartum women had an unmet need for family planning [4]. The 2016 EDHS showed that the total demand for family planning nationwide and in the Amhara region is 40.5% and 45.9% where only 61.4% and 73.4% of the demand for family planning is satisfied with modern contraceptives respectively. The current national and regional (Amhara) unmet need for family planning is 15.2% and 11.8% respectively (4,9,10). Postpartum women are among those with the greatest unmet need for family planning and yet they often do not receive the services they need to support longer birth intervals or reduce unintended pregnancy and its consequences [7].
Community-based cross-sectional studies conducted in Dabat district (2012), Gondar town (2013), Addis Ababa city (2014), and Axum town (2015) showed a 10.3%, 48.4%, 80.3%, and 48.0% respectively of modern contraceptive use in the postpartum period. The studies also indicated that injectable contraceptive was the most commonly used method and women who delivered with the assistance of a skilled attendant and attended postnatal care services were more likely to use contraceptives. [11–13]. In other institutional cross-sectional study conducted in Gondar town in 2015, 45.8% of mothers used modern contraceptives during their postpartum period, where Injectable contraceptive was the most frequently used method [14]. The relationship between modern contraceptive use in the postpartum period and its associated potential explanatory factors in the postpartum period can be grossly divided into demographic characteristics, socioeconomic characteristics, fertility preferences, and use of maternal health services [15]. A mixed method study on contraceptive use among postpartum women in a county hospital in rural Kenya showed a significant association (p ≤ 0.05) between uptake of postpartum family planning and lower age, being married, higher education level, being employed and getting contraceptives at a health facility [16]. A population-based cross-sectional study on predictors of modern contraceptive use during the postpartum period among women in Uganda showed a significant association of postpartum modern contraceptive use with primary and higher education; richest wealth status; protestant religion; age of woman. In addition, number of surviving children; exposure to media; skilled birth attendance; and 1–2 days timing of post-delivery care were also associated with modern contraceptive use in the postpartum period [17].
Studies done in different parts of Ethiopia showed that postpartum modern contraceptive use is significantly associated with women’s educational level, family planning counseling during ANC and PNC, utilization of PNC services, menses having returned after birth, resuming sexual activities, living with their sexual partners, and having experienced problem with previous contraceptive use and these indicate that facility delivery can be taken as an important window of opportunity to provide access to family planning messages and to offer women with various contraceptive methods. These findings underline the needs for service integration within the public sector to take advantage of the facility delivery to increase the uptake of family planning during the critical postpartum period [18,19]. Resumption of menses, Secondary and tertiary education levels; [20] Menstruating, and resumption of sex [14]; skilled deliveries and postnatal care services; [21] having no plan to have another child and undecided plan to have another child [22]; richest wealth status, protestant religion and age of woman [17]; Contraceptive counselling, getting information from the health facility, and partner support [23] were indicated to be predictors of modern contraceptive use in the postpartum period. Even though directing efforts to increase modern contraception among postpartum women could have a significant impact on increasing contraceptive prevalence rate and other health benefits, contraceptive use in the postpartum period is less emphasized by policy makers and program designers in Ethiopia [25]. While there is an opportunity of reaching women in their postpartum period either during their time of giving birth at the health facilities or while coming to health facilities accompanying their babies for immunization, evidence show that these opportunities are missed by health care providers to provide appropriate information, counseling, and service on family planning for reasons usually not proved scientifically (26).
Though few studies on utilization of modern contraception and its determinants during the postpartum period (PPP) are done in some parts of Ethiopia including the Amhara region, where the study site is located, there still remains to support program strategies and service delivery modalities of the study area with context-specific evidences of the magnitude of the service utilization and its determinants in a hospital set-up considering the high volume of institutional deliveries and the opportunities of well-baby and sick baby child care visits for immunization and growth monitoring in such facilities during the postpartum period. As to the researcher’s knowledge, there is no published literature regarding utilization and predictors of modern contraceptives in postpartum women in Bahirdar city. This study, therefore, addressed the knowledge gap in generating evidence for postpartum modern contraceptive use and its predictors in postpartum women and suggested plausible and workable recommendations to health care providers, programmers, policy makers, and other relevant stakeholders for policy revisions and strategies design to maximize postpartum contraceptive use for the betterment of both women's’ and children's’ health. This study was designed to assess the utilization and predictors of modern family planning in the postpartum period in Felegehiwot referral hospital, Bahirdar city, Northwest Ethiopia.
Methods
Study setting and design
study was conducted in Felegehiwot referral hospital, Bahirdar city administration, the capital of Amhara Regional State, Northwest Ethiopia from January 1-31, 2019. The city is located at 565 km Northwest of Addis Ababa, the capital city of Ethiopia. According to Amhara regional bureau of finance and economic Development (BoFED) 2016 report, Bahirdar city administration is divided into 9 sub-cities. The total population of the city is estimated to be 311,724 in 2016 with a female population representing 52.6% of the total. Women of reproductive age comprise 23.6% in the region and the total number of estimated pregnancies / Births in the regions is estimated to be 3.4%.
In Bahir Dar city, there are two government hospitals, one private general hospital, ten health centers, ten higher and 20 medium private and NGO clinics and 60 private drug retails. Although all public and private health facilities are expected to provide family planning services, postpartum family planning is not being provided well in most of the private health facilities due to various reasons including service fees and staff capacity issues and hence most deliveries and postnatal services are provided in the public health facilities. Felegehiwot referral hospital is the only referral hospital in the city serving the surrounding urban and rural areas as a center for better maternal and child health services among the public health facilities. Therefore, all postpartum women who have had a visit in Felegehiwot referral hospital during the study period were included in the study. A facility based cross-sectional study was employed.
First: n=
Sample size calculation and sampling procedure
sample size for the study was computed by using the single population proportion formula with the following assumptions: The proportion of women using modern contraceptive in their postpartum period taken from a previous facility based cross sectional study conducted in Debreberhan town in 2016 to be 41.6% (27), 95% confidence level and 5% margin of error. For the second objective of the study, resumption of sexual intercourse after 6 weeks postpartum (≈50%) was reported by the same study as an important predictor of modern contraceptive use in the postpartum period. Considering a 10% non-response rate, a final sample size of 425 women was taken. Where: n= the required sample size
Z = the standard score corresponding to 95% CI, and is equal to 1.96 P = the proportion of modern contraceptive use which is 41.6%
d2 = level of precision (margin of error) which is taken 5%
The sample size for the second specific objective was calculated using two population proportion formula for the variables which have significant association in a previous study and hence resumption of sexual intercourse and resuming of menses were reported to be important predictors for modern postpartum contraceptive use. The sample sizes using the two-population proportion formula is shown in the table below
Where: n= the required sample size
Z1 = the standard score corresponding to 95% CI, and is equal to 1.96
P1 = the proportion of modern contraceptive use which is 53.7% (resuming sex) Z2 = the standard score corresponding to 95% CI, and is equal to 1.96
P2 = the proportion of modern contraceptive use which is 72% (resuming menses)
d2 = level of precision (margin of error) which is taken 5% for both
Hence, the sample size which is calculated for the resumption of sex is greater than that of the first specific objective and the second factor for the second objective i.e., resuming menses. Therefore, the largest sample size for one of the predictors i.e., “resuming sex” was 425 was taken as a final sample size. Considering the possible homogeneity of MCH and RH/FP services provision in all public health facilities in Bahirdar city administration, Felegehiwot referral hospital, the only referral hospital in the city administration was selected purposely for this research among the 12 public health facilities for having higher service volume and serving as a referral point for other facilities. Again, since the socio-demographic characteristics of the clients visiting the hospital for MCH and RH/FP services has homogenous nature and clients coming from rural areas use opportunities like market days, study participants fulfilling the inclusion criteria were consecutively interviewed until the maximum required sample size is achieved.
Data collection and analysis
Data was collected using a structured questionnaire which was adapted from the Reproductive Health Assessment Toolkit for Conflict-Affected Women, due to absence of other tools, prepared by division of reproductive health, National Center for Chronic Disease Prevention and Health Promotion, Coordinating Center for Health Promotion, Centers for Disease Control and Prevention, Department of Human Services, 2007 through a face-to face interview. The questionnaire was translated to the local language, Amharic, and pretested in one of the health centers and finally re-translated back to English by another translator to check consistency. Four data collectors, that are clinical nurses by profession, and one health officer were deployed and trained on data collection procedures, data quality, and ethical issue. The data collection process was supervised by the principal investigator.
Training was provided to data collectors on the overall data collection procedures and the techniques of interviewing daily to ensure data quality. The data collection tool was pretested among 5% of the calculated sample population in similar settings of postpartum women. The collected data was checked for completeness, consistency, accuracy, and clarity by the principal investigator daily. Moreover, the necessary and timely corrective measures were taken for missing values, irregularities, inconsistencies, unlikely values, and suspicious irregularities.
After the completion of data collection, all completed questionnaires were checked for completeness and consistency of responses manually, data were categorized and coded by the PI and epi-info version 7.2.2.6 software were used for data entry, cleaning and checking. The entered data was exported to SPSS version 22.0 for analysis. Finally, descriptive statistics was done to summarize the study variables. Both bi-variate and multivariate logistic regressions were used to identify associations. Variables having P-value < 0>Ethical considerations
Before commencing the study, ethical clearance was received from the Ethical Clearance Committee of Addis Continental Institute of Public Health (ACIPH), a formal letter obtained from ACIPH was submitted to Amhara Public Health Institute and a copy to Felegehiwot referral hospital. Permission was also obtained from the Amhara Public Health Institute and Felegehiwot referral hospital medical director. Informed verbal consent was taken from each study participant to ensure their willingness for participation after explaining the objective of the study. Respondents’ name and personal identifiers were not included in the study. Key messages about the importance of postpartum contraceptive use during the postpartum period were provided to mothers who didn’t get appropriate information on modern contraceptives at the end of each interview.
Results
Socio-demographic characteristics
A total of 425 mothers in the postpartum period who visited Felegehiwot referral hospital for various maternal and child health services have participated in the study with 100% response rate. The median age (+ IR10) of the study participants was 27 years with age range of the 18-42 years. Most of the participants (2 7.8%) fall in the age segment between 25 and 29 years. The majority, 347 (81.6%) of the mothers reported that they were in marital union. Of the total respondents, the vast majority, 263 (61.9%) were Orthodox Christian followers; followed by 103 (24.2%) Muslims, 35 (8.2%) Protestants, and 24 (5.6%) Catholics. Four in ten (39.1%) respondents and nearly two third (63%) of their partners have attended tertiary education. Moreover, most of the study participants 188 (44.2%) were employed and the rest 158 (37.2%) and 79 (18.6%) were unemployed and students respectively (Tab 2).
Table 1: Socio-demographic characteristics of postpartum women attending in Felegehiwot referral Hospital, Northwestern Ethiopia, 2019 (n=425)
| Variable | Frequency | % | |
| Age | 15-19 | 26 | 6.10% |
| 20-24 | 105 | 24.70% | |
| 25-29 | 118 | 27.80% | |
| 30-34 | 104 | 24.50% | |
| Above 35 | 72 | 16.90% | |
| Marital Status | Married | 347 | 81.60% |
| Not married | 78 | 18.40% | |
| No formal education | 88 | 20.70% | |
| Respondent’s Education | Primary education (1-8) | 22 | 5.20% |
| Secondary education (9-12) | 149 | 35.10% | |
| Tertiary education | 166 | 39.10% | |
| Spouse’s Education | No formal education | 33 | 7.80% |
| Primary education (1-8) | 19 | 4.50% | |
| Secondary education (9-12) | 41 | 9.60% | |
| Tertiary education | 266 | 62.60% | |
| Employment | Employed | 188 | 44.20% |
| Unemployed | 158 | 37.20% | |
| Student | 79 | 18.60% | |
| Orthodox | 263 | 61.90% | |
| Muslim | 103 | 24.20% | |
| Religion | Protestant | 35 | 8.20% |
| Catholic | 24 | 5.60% |
Reproductive and maternal health services- related characteristics
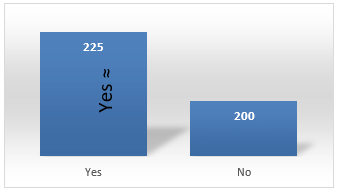
The median parity (± IR 2) of the study participants was 2 with 410 (96.5%) of the study participants having 1-4 births and the median number of children intended to have been 4 per women (IR, ±1). Out of 361 women, only 195 (54%) of them responded that they have discussed with their spouse on modern contraceptive use and majority of them 170 (87.2%) had a positive discussion with their spouse. Nearly half, 225 (52.9%) of the postpartum women were using modern contraceptives prior to their last child (Fig 1).
Figure 1: Modern contraceptive users among postpartum women in Felegehiwot referral hospital, North West Ethiopia, January 2019 (n = 425).
Of the total study participants, 380 (89.4%) had received family planning counseling during their ANC and delivery service visits (Table 2). Modern contraceptive use in the postpartum period was reported by 225 women (52.9%; 95% CI, 44.0 to 57.6). The following chart depicts the contraceptive methods by the study participants. Out of the study participants, 153 (69.2%) used modern contraceptive methods for spacing. Among those women who were using modern contraceptive methods in their postpartum period, 174 (78.7%) received their contraception choices from government health facilities. The postpartum women pointed out various reasons for currently not using modern contraceptive methods, such as Breast feeding (32.8%), not having sex (21.1%), Knows no method (12.7%), Wants a child soon (11.3%), and Fear of side effects (8.3%).
Factors associated with modern family planning use
During the bivariate logistic regression, ten variables that means educational status of the respondents, spouses’ educational status, current marital status, age of the respondents, employment status, Parity, Gravidity, awareness about PPFP, spousal reaction for FP related discussion and contraceptive education during ANC and PNC were associated with modern contraceptive use among postpartum women. However, only the following four variables were identified as independently associated with postpartum modern contraceptive use in the multivariate logistic regression analysis. These were current marital status, age of the respondents, Gravidity, and awareness about postpartum modern contraceptives.
Women who had awareness about modern contraceptive methods were about 17 times more likely to use modern contraceptives in the postpartum period as those who did not (AOR, 16.99; 95% CI, 2.85 to 101.16). Married women were three times more likely to use modern contraceptives than those who are currently alone (AOR, 3.052; 95% CI, 1.644 to 5.667). Postpartum women of age 31-35, >35, and 25-30 years are almost 6 (AOR, 5.825; 95% CI, 2.519, 13.467), 4.5 (AOR, 4.521; 95%CI 1.821, 11.226), and 4 (AOR, 4.153; 95%CI, 2.069, 8.338) times more likely to use modern contraceptives in the postpartum period than those of less than 24 years of age. Being a student was found to be 22% protective in using modern contraceptives than being unemployed (AOR, 0.216; 95% CI, 0.085, 0.546). Being a woman of gravidity more than 5 was also found to be 15% protective for postpartum modern contraceptive use than those who are gravida of 1-4 (AOR, 0.19; 95% CI, 0.05 to 0.72) (Table 2). The main reasons for non-use of modern contraceptives in the postpartum period identified in this study were not having sex, need for more children, partner disapproval, breast feeding, fear of side effects, lack of knowledge on the methods and source where to find the contraceptives. The 2016 Ethiopian Demographic and Health Survey [10] and other studies conducted in Gondar [14], Axum (33), Kebribeyah (18) and Dembia district [2] revealed similar reasons.
Discussion
About two‐thirds of women would like to avoid pregnancy in the first year after a delivery but are not using contraception [29]. This unmet need is an important public health concern, because approximately 20% of obstetric deaths are attributable to non‐ use of modern contraception [30]. Additionally, family planning has the potential to avert maternal and child morbidity by allowing couples to space their pregnancies more than 2 years apart [31].
The prevalence of modern contraceptive use among postpartum women was 52.9% [48.0, 57.9] in this study. The finding of this study was comparable with previous studies reported in northern Ethiopia (48.0%), Gondar town (48.4%), Kenya and Zambia (46%), Mexico (47%) [32] and in Rwanda (50%) [29-31]. On the other way, this study indicates slightly higher acceptance and use compared with the magnitude of modern contraceptive use among postpartum women in Dabat district (10.3%) [33]. The discrepancy might be due to the study period, sample size differences and socio-demographic characteristics between the current and the previous studies. This study finding also became lower compared with a study reported in Addis Ababa (80.3%) which might be because of the differences in the study setting (community based versus facility based), and sample size which is lower for the current study [34].
Injectable contraceptives are the most widely used methods in this study (44.3%) followed by implants (38.5%) and IUCD (13.6%). The finding shows that there is a skewness in the utilization of modern contraceptives in the postpartum women towards injectable contraceptives. This finding is consistent with a study done in Dabat district [11], Gondar town [14,35], Addis Ababa city [34], the 2016 national data [10]. These studies revealed that 77%, 86.5%, 55.62.2% and 23% of women used injectable contraceptives respectively. This can be explained by the preference and contraceptive choices of study participants, availability of trained health workforce, attitudes of service providers and availability of mix of contraceptive choices in the facility. Married postpartum women were three times [AOR=3.052, 95% CI: 1.644, 5.667] more likely to use modern contraceptive method as compared with women who are not in marital union. The Ethiopian Demographic and Health Survey shows a show a 10.4% increase in use of modern contraceptives among married women than all women [10]. This may be because married women have more frequent sexual contacts than those who are not in marital union.
This study found that contraceptive use in the lower age range is minimal. This finding is comparable with a study conducted in Uganda [17] and the 2016 Ethiopian Demographic and Health Survey [10] where lower age women are less likely to use contraceptives and contradicts the finding from a study conducted in Kenya where it revealed the reverse [36]. This can be justified by low access to information and services, fear of side effects, providers and societal attitudes towards use of modern contraceptives by young women, high expectations of frequent deliveries from family members, and weak counseling services during ANC. Postpartum women who have had awareness about postpartum family planning were about seventeen [16.99, 95% CI: 2.85- 101.16] times more likely to use modern contraceptive during their postpartum period as compared with their counterparts. This indicates that having the information and knowing where to go to get contraceptives services matters a lot for a woman to use modern contraceptives during the postpartum period. Being aware about the method choices, the cons and prons of contraceptives positively affects women’s perception towards the myths and misconceptions about contraceptives. Which in turn might help women opt to use modern contraceptives of their choice either to space or limit their pregnancies. This finding is in agreement with a previous study done in Addis Ababa [23].
The main reasons for non-use of modern contraceptives in the postpartum period identified in this study were not having sex, need for more children, partner disapproval, breast feeding, fear of side effects, lack of knowledge on the methods and source where to find the contraceptives. The 2016 Ethiopian Demographic and Health Survey [10] and other studies conducted in Gondar [14], Axum [33], Kebribeyah (18) and Dembia district [2] revealed similar reasons. Due to time and resource constraints, the study focused on women attending major MCH services at Felegehiwot referral hospital and study participants were interviewed consecutively until the maximum sample size attained. This limited inclusion of women from other public health institutions and hinders randomization of study units. Moreover, having a qualitative component in the study design would also have added the flavor in identifying intrinsic barriers and facilitators for modern FP use in the postpartum period.
Table 2: Factors associated with postpartum modern contraceptive use in Felegehiwot Referral Hospital, North Western Ethiopia, January 2019 (n = 425)
| Factor | Modern Contraceptive Use | COR | AOR | ||
| Yes | No | ||||
| Educational status of the spouse the respondents | No formal education | 38 | 5000.00% | 0.453 [0.268, 0.767] | 2.423 [0.814, 7.216] |
| Primary education | 12 | 1000.00% | 0.715 [.292, 1.753] | 3.864 [1.006, 14.845] | |
| Secondary education | 71 | 7800.00% | 0.543 [0.346, 0.851] | 1.505 [0.730, 3.103] | |
| Tertiary education | 104 | 6200.00% | 1 | 1 | |
| Educational status of the spouse | No formal education | 19 | 3300.00% | 0.390 [0.268, 0.767] | 0.588 [0.252, 1.371] |
| Primary education | 12 | 2300.00% | 0.384 [0.292, 1.753] | 0.911 [0.374, 2.215] | |
| Secondary education | 27 | 3100.00% | 0.589 [0.346, 0.851] | 0.982 [0.495, 1.948] | |
| Tertiary education | 167 | 11300.00% | 1 | 1 | |
| Marital status | Married | 199 | 14800.00% | 2.689 [1.064, 4.508] | 3.052 [1.644, 5.667] * |
| Not married | 26 | 5200.00% | 1 | 1 | |
| Age of the respondents | Less than 24 years | 49 | 8200.00% | 1 | 1 |
| 25-30 years | 92 | 5200.00% | 2.961 [1.812, 4.837] | 4.153 [2.069, 8.338] * | |
| 31-35 years | 52 | 3000.00% | 2.901 [1.637, 5.139] | 5.825 [2.519, 13.467] * | |
| Greater than 35 years | 32 | 3600.00% | 1.488 [1.822, 2.692] | 4.521 [1.821, 11.226] * | |
| Employment Status | Employed | 127 | 6100.00% | 3.058 [1.776, 5.264] | 1.055 [0.385, 2.888] |
| Unemployed | 66 | 9200.00% | 1.054 [0.608, 1.825] | 0.189 [0.054, 0.656] | |
| Student | 32 | 4700.00% | 1 | 1 | |
| Parity | 01-Apr | 212 | 198 | 1 | 1 |
| > 5 | 13 | 2 | 6.071 [1.35-27.24] | 0.12 [0.12-1.24] | |
| Gravidity | 01-Apr | 199 | 190 | 1 | 1 |
| > 5 | 26 | 10 | 2.482 [1.17-5.29] | 0.19 [0.05-0.72] * | |
| Aware about PPFP | Yes | 223 | 150 | 37.167 [8.90-155.06] | 16.99 [2.85-101.16] * |
| No | 2 | 50 | 1 | 1 | |
| Spousal Reaction for | Positive | 5 | 20 | 0.065 [0.015-0.118] | 0.42 [0.14-1.25] |
| FP related discussion | Embarrassing | 135 | 35 | 1 | 1 |
| Contraceptive education during | Yes | 157 | 223 | 0.033 [0.013-0.079] | 2.79 [0.55-14.18] |
| ANC and PNC | No | 43 | 2 | 1 | 1 |
COR - crude odds ratio; AOR - adjusted odds ratio; *p value<0>
Conclusion
Generally, utilization of modern contraceptive in the postpartum period is lower and this might result in putting women at risk of being pregnant in the first year of their childbirth. Modern contraceptive use among postpartum women is affected by being younger, single, multigravida, and having low awareness. Health facility visits in the postpartum period is the most critical window of opportunity for women to receive appropriate counseling and services on family planning. However, there appears to be major missed opportunity that significant number of clients were left unaware of modern postpartum contraceptives.
Acknowledgements
We would like to pass our heartfelt gratitude to Addis Continental Institute of Public Health and Amhara Public Health Institute for the approval of the ethical clearance and the support provided during the study. We are also very thankful for all women who participated in this study and show their commitments.
References
- G. Eason, B. Noble, and I. N. Sneddon. (1955). On certain integrals of Lipschitz-Hankel type involving products of Bessel functions, Phil. Trans. Roy. Soc. London, A247:529-551.
Publisher | Google Scholor - J. Clerk Maxwell, A. (1982). Treatise on Electricity and Magnetism, 3rd ed., Oxford: Clarendon, 2:68-73.
Publisher | Google Scholor - S. Jacobs and C. P. Bean. (1963). Fine particles, thin films and exchange anisotropy, in Magnetism, vol. III, G. T. Rado and H. Suhl, Eds. New York: Academic, 271-350.
Publisher | Google Scholor - K. Elissa, Title of paper if known, unpublished.
Publisher | Google Scholor - R. Nicole, Title of paper with only first word capitalized, J. Name Stand. Abbrev., in press.
Publisher | Google Scholor - Y. Yorozu, M. Hirano, K. Oka, and Y. Tagawa. (1987). Electron spectroscopy studies on magneto-optical media and plastic substrate interface, IEEE Transl. J. Magn. Japan, 2:740-741:301, 1982.
Publisher | Google Scholor - M. Young, The Technical Writer's Handbook. Mill Valley, CA: University Science, 198.
Publisher | Google Scholor - Krejcie, R. V. and D. W. Morgan (1970) Determining Sample Sizes for Research Activities. Educational and Psychological Measurement, 30:607-610.
Publisher | Google Scholor - Kass, R. E. and A. E. Raftery (1995). Bayes Factors. Journal of the American Statistical Association, 90:773-794.
Publisher | Google Scholor - Spiegelhalter, D. J., N. G. Best, B. P. Carlin, and A. van der Linde (2002). Bayesian Measures of Model Complexity and Fit (with discussion). Journal of the Royal Statistical Society:Series B, 64:583-639.
Publisher | Google Scholor - Ebenebe, C. I., Anigbogu, C. C., Anizoba, M. A. and Ufele, A. N. (2013). Effect of various levels of Moringa Leaf Meal on the Egg Quality of Isa Brown Breed of Layers. Advances in Life Sciences and Technology, 14:45-49.
Publisher | Google Scholor - Fahey, J. W., Zakmann, A. T., and Talalay, P. (2001). The chemical diversity and distribution of glucosinolates and Isothiocyanates among plants. Corrigendum Phytochemistry, 59:200-237.
Publisher | Google Scholor - Greg, M. E. (2008). Effect of enzymes on cellulose, European Journal of Applied Microbiology Biotechnology, 40:167 -171.
Publisher | Google Scholor - Onunkwo, D. N and George, O. S (2015). Effects of Moringaoleifera leaf meal on the growth performance and carcass characteristics of broiler birds. IOSR Journal of Agriculture and Veterinary Science, 8 (3II): 63-66.
Publisher | Google Scholor - El Tazi, S. M. A. (2014). Effect of feeding different levels of Moringaoleifera leaf meal on the performance and carcass quality of broiler chicks. International Journal of Science and Research, 3 (5):147-151.
Publisher | Google Scholor