Case Report
Uterine Necrosis Following Conservative Treatment for Postpartum Haemorrhage in A Case and Literature Review
- R. Sabiri *
- K. Benhaddougua
- K. Fadil
- Z. Lebdaoui
- A. Assal
- M. Jalal
- A. Lamrissi
- S. Bouhya
Service de maternité gynecologie obstetrique hôpital mère enfant Abderahim El Harouchi, Casablanca, Morocco.
*Corresponding Author: R. Sabiri, Service de maternité gynecologie obstetrique hôpital mère enfant Abderahim El Harouchi, Casablanca, Morocco.
Citation: Sabiri R., Benhaddougua K., Fadil K., Lebdaoui Z., Assal A., et al. (2024). Uterine Necrosis Following Conservative Treatment for Postpartum Haemorrhage in A Case and Literature Review, International Journal of Clinical and Surgical Pathology, BioRes Scientia Publishers. 1(2):1-11. DOI: 10.59657/3067-0462.brs.24.006
Copyright: © 2024 R. Sabiri, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: June 19, 2024 | Accepted: August 05, 2024 | Published: August 12, 2024
Abstract
Delivery hemorrhage remains the leading cause of death in most countries, including Morocco. Its management must be multidisciplinary and rapid. Uterine compression techniques have not been widely evaluated, but have been rapidly disseminated throughout the world due to their ease of application. Nevertheless, secondary complications have been reported in the literature, including uterine necrosis. We report a case of uterine necrosis following conservative surgical treatment of delivery hemorrhage using a combination of the B-Lynch uterine compression technique and Tsirulnikov triple vascular ligation. The patient presented with sepsis on postpartum day 2, with fever, pelvic pain and a biological inflammatory syndrome that worsened 48 hours later. Pelvic CT showed no enhancement of the myometrium after injection of PDC, suggesting myometrial necrosis. An exploratory laparotomy was performed, which revealed complete necrosis of the uterus.
The surgical technique of uterine compression sutures plays a major role in the therapeutic arsenal of post-partum hemorrhage, enabling the patient's fertility to be preserved, but it also requires maximum caution and monitoring for complications, the most serious of which is uterine necrosis.
Keywords: uterine necrosis; conservative surgical treatment; patient's fertility
Introduction
Postpartum hemorrhage remains the leading cause of maternal mortality, which is estimated at 227 maternal deaths per 100,000 births in Morocco [1]. It is an obstetric emergency that requires rapid, effective and multidisciplinary care. Primary PPH (within 24 hours after delivery) occurs in 4 to 6% of pregnancies, and is caused by uterine atony in 80% of cases [2]. Various medical and surgical techniques are used to control it. In cases of severe postpartum hemorrhage that is resistant to medical treatment, advances in interventional radiology and especially surgical techniques have provided safe and effective alternatives to hemostasis hysterectomy. Uterine compression surgical techniques are part of the therapeutic strategy adopted in the face of hemorrhage of delivery, their rapid spread is due to their ease of implementation. However, some secondary complications, including uterine necrosis, have been reported in the literature [3]. We report a rare case of uterine necrosis following a combination of uterine compression sutures and vascular ligation.
Case Presentation
This is a 39-year-old patient with no significant medical history. Fifth gesture, fourth part (1MFIU; context?), the four ancient deliveries were by way of low voice. The current pregnancy has taken place without abnormalities. The patient presented to the maternity ward at the beginning of labour with a pregnancy presumed to be at term, the course of labour was harmonious until a dilation of the cervix of 8 cm or she presented acute fetal distress with severe bradycardia objectified by the recording of the fetal heart rhythm. An emergency caesarean section was indicated, which allowed the extraction of a female newborn Apgar 6/10th, birth weight: 3100 grams. The patient presented intraoperatively with a delivery hemorrhage due to uterine inertia. Uterine massage supplemented by oxytocin infusion and administration of 5 intrarectal tablets of misoprostol (due to the unavailability of sulprostone) did not correct the uterine atony, and since the embolization technique is not available in our center, Tsirulnikov's triple ligation and hypogastric artery ligation associated with uterine compression using the B-Lynch technique using a Vicryl 1 absorbable thread were used. The bleeding stopped and the patient received a red blood cell transfusion.
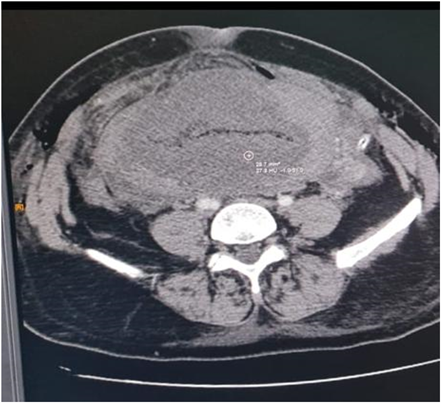
The postoperative course was normal until the 2nd postoperative day when the patient presented with a febrile peak associated with abdominal pain and diffuse abdominal tenderness, the squints were not fetid and were without metrorrhagia. A The WBC blood count = 1670/mm3, Hb = 7.1 g/dl and a CRP >160 mg/L. A pelvic ultrasound was performed showing a globular uterus, of heterogeneous echo structure with a thin and central Endo cavitary line, site of hyperechoic spots generating a comet-tailed artefact related a priori to air bubbles. Absence of detectable intraperitoneal effusion. A pelvic CT scan was performed showing myometrial necrosis, in the absence of enhancement after PDCI injection; this hypothesis was supported by the notion of bilateral ligation of the hypogastric arteries (Figure 1).
Figure 1: Pelvic CT Showing Multiple Air Bubbles in Endo Cavitary with Absence of Myometrium Enhancement After PDC Injection, Suggestive of Myometrial Necrosis.
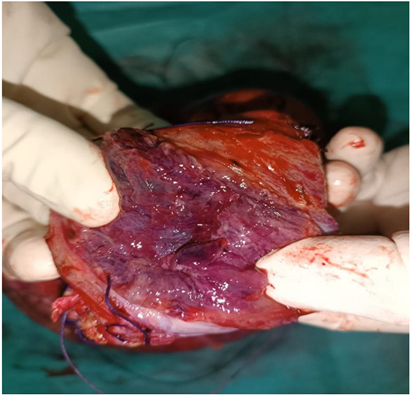
Functional hail distension. The patient was put on a broad-spectrum antibiotic to treat possible endometritis. Forty-eight hours later, the evolution was marked by no clinical-biological improvement; Hb: 5.6 and a CRP >160 mg/L. An exploratory laparotomy was indicated as an emergency. Surgical exploration found extensive uterine necrosis especially in its anterior surface, a hysterography partially open in the center and superinfected with the presence of false membranes occupying the entire anterior surface of the uterus. The necrosis was definitive despite the removal of the sutures of the vascular ligatures previously performed. A total hysterectomy was performed (Figure 2) with abundant serum lavage of the peritoneal cavity with placement of a pelvic tube removed two days later. The post-operative course was favorable and the histopathological examination confirmed the diagnosis of uterine necrosis.
Figure 2: The Hysterectomy Specimen Showing the Extent of Necrosis and Superinfection of The Uterus.
Discussion
Deliverance haemorrhage is the leading cause of maternal mortality in Morocco [1], it is an obstetric emergency that quickly puts the maternal prognosis at stake. Management of severe postpartum hemorrhage should be as quick, simple, and conservative as possible.[5] The first measures are always associated and concomitant. Its classic treatment consists of a certain number of procedures (uterine massage, uterine revision, indwelling bladder catheterization, examination of the genital tract, infusion of oxytocin, or even prostaglandins) and resuscitation measures (vascular filling, transfusion of red blood concentrates) which must be carried out systematically before considering a therapeutic escalation. If these measures fail, and/or if the patient's condition is unstable, surgical treatment is necessary, there are many surgical techniques for the management of postpartum hemorrhage and hysterectomy remains the reference solution in this context. Many advances have been made in conservative treatment (vascular ligations, folding’s and uterine pimples); radical surgical treatment (hemostasis hysterectomy) is sometimes the last step in saving the patient.
The techniques of uterine folding, B-Lynch and uterine compression or dimpling (Cho) appear to be an interesting alternative, especially in the case of uterine atony, they make it possible to achieve hemostasis by compressing the anterior wall against the posterior wall by simple or framed transfixing points; These techniques are certainly promising, but they deserve more hindsight and reported cases [6]. Although these compression and uterine ligation techniques have been poorly evaluated, the ease of implementation has allowed them to be rapidly disseminated throughout the world. As a result, some complications have occurred: pyrometry, erosion of the strap through the uterine wall, uterine ischemia, uterine necrosis, synechia. However, the frequency of such complications remains uncertain given the absence of large reports in the literature concerning these procedures, but could be 5 to 7% [7]. The nature of the threads used (resorption time) and the initial degree of tension of the points are two elements that can explain the variations in terms of ischemia. The technique itself could have an influence on the occurrence of necrosis: uniform compression that does not interrupt the parietal vascularization in its entirety (in particular by avoiding sutures in the horizontal direction and by performing them only in the vertical direction) could reduce this risk [8]. It would appear that the correct placement of compression points (alone or in combination with other hemostatic procedures) in such a way that myometrial reperfusion through the collateral anastomotic network is preserved may decrease the risk of necrosis [9].
In our case, despite the realization of single stitches in the vertical direction, we had as a complication partial uterine necrosis. The technique of uterine folding and compression or padding is a simple procedure to perform. Imaging plays an important role in diagnosis. The ultrasound is the first line because it shows a large uterus with a redefined wall and a heterogeneous image is associated with the presence of air in the uterus. The use of CT scan is also often useful, because in our case it revealed uterine necrosis with the presence of gas bubbles in the myometrium and endometrium and a lack of myometrium enhancement. Systematic evaluation of the uterine cavity after this type of conservative treatment is necessary to make the diagnosis of uterine necrosis or synechia and to rule out retained placenta, which is the main differential diagnosis, until prognostic safety in terms of fertility and uterine frailty is established.
Conclusion
Conservative treatment by compression or uterine padding is an easy procedure to perform as part of the therapeutic strategy in the face of a hemorrhage of delivery. It allows, in addition to or as an alternative to vascular ligation, the preservation of the patient's fertility, but it also requires caution and maximum monitoring of complications, the most serious of which is uterine necrosis.
Declarations
Patient Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Ethical Approval
I declare on my honor that my establishment has exempted the ethical approval
Sources of Funding
None.
Author’s Contribution
All authors have read and approved the final version of the manuscript.
Declaration of Competing Interest
The authors declare having no conflicts of interest in this article.
References
- Alaoui Belghiti Z. (2011). The Hemorrhage of Deliverance About 170 Cases. University Editions. 1-216.
Publisher | Google Scholor - Akoury H, Sherman C. (2008). Uterine Wall Partial Thickness Necrosis Following Combined B-Lynch and Cho Square Sutures for The Treatment of Primary Postpartum Hemorrhage. J Obstet Gynaecol Can. 30(5):421-424.
Publisher | Google Scholor - Alaoui FZ, Jayi S, Bouguern H, Melhouf M, El Fatemi H, et al. (2013). Partial Uterine Parietal Necrosis After Hemostatic Padding During a Postpartum Hemorrhage. Pan Afr Med J. 15:32.
Publisher | Google Scholor - Benkirane S, Saadi H, Serji B, Mimouni A. (2017). Uterine Necrosis Following a Combination of Uterine Compression Sutures and Vascular Ligation During a Postpartum Hemorrhage: A Case Report. Int J Surg Case Rep. 38:5-7.
Publisher | Google Scholor - Brace V., Penney G., Hall M. (2004). Quantifying Severe Maternal Morbidity: A Scottish Population Study. BJOG. 111:481-484.
Publisher | Google Scholor - Ducarme G, Bargy S, Grossetti A, Bourgeois B, Levardon M, et al. (2007). Surgical Management of Postpartum Hemorrhages: A Retrospective Study. Gynecology, Obstetrics and Fertility. 35(12):1209-1214.
Publisher | Google Scholor - Sentilhes L, Gromez A, Descamps P, Marpeau L. (2009). Why Stepwise Uterine Vascularization Should Be the First-Line Conservative Surgical Treatment To control Severe Postpartum Hemorrhage. Acta Obst Gynecol Scand. 88:490-492.
Publisher | Google Scholor - Reyftmann L, Nguyen A, Ristic V, Rouleau C, Mazet N, et al. (2009). Partial Uterine Parietal Necrosis After Haemostatic Dimpling Using the Cho Technique During Postpartum Haemorrhage. Gynecology, Obstetrics and Fertility. 37(6):579-582.
Publisher | Google Scholor - Palacios-Jaraquemada J-H, Bretelle F. (2009). How To Avoid Complications During Hemostatic Sutures According To Cho. Gynecology, Obstetrics and Fertility. 37(10):844-845.
Publisher | Google Scholor