Review Article
Use of Platelet Rich Plasma in Otolaryngology-Review Article
1Intern, Acharya Vinoba Bhave Rural Hospital, Jawaharlal Nehru Medical College, India.
2Associate Professor, Department of ENT, Acharya Vinoba Bhave Rural Hospital, Maharashtra, India.
*Corresponding Author: Shweta Satpathi,Intern, Acharya Vinoba Bhave Rural Hospital, Jawaharlal Nehru Medical College, India
Citation: Shweta S, Sagar G. (2023). Use of Platelet Rich Plasma in Otolaryngology-Review Article, International Journal of Medical Case Reports and Reviews, BRS Publishers. 2(5); DOI: 10.59657/2837-8172.brs.23.029
Copyright: © 2023 Shweta Satpathi, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: July 17, 2023 | Accepted: August 02, 2023 | Published: August 26, 2023
Abstract
The process of replacing or regenerating human cells, tissues, or organs to restore or establish normal function is known as REGENERATIVE MEDICINE. It is a brand new, developing field of medicine that deals with the functional repair of tissues or organs damaged by severe trauma or degenerative conditions. Currently, platelet-rich plasma (PRP) and stem cell-based treatments are the two competing technologies that can heal and restore the injured tissues. Platelet-rich plasma (PRP) applications used in new autologous cellular therapeutics have the potential to supplement a range of regenerative medicine therapy regimens [1]. An emerging and effective treatment alternative in musculoskeletal therapy is platelet-rich plasma (PRP) PRP is an autologous plasma preparation that has been enhanced with platelet concentrations above those seen in whole blood ordinarily. High platelet concentration has therapeutic promise because of their ability to give supraphysiologic levels of vital growth factors, which operate as a regenerative stimulus to encourage repair in tissues with poor healing capabilities [2]. A concentration of platelet-rich protein generated from blood that has been spun to remove the red blood cells is known as platelet-rich plasma (PRP), or more accurately autologous conditioned plasma. Despite being advertised to cure a variety of medical ailments, there is conflicting evidence for profit as of 2020, with some evidence supporting usage in some circumstances and opposing use in other. A unique substance that is being employed in several surgical specialities is platelet-rich plasma. The aim of the article is to review the ongoing and prospective utilization of platelet-rich plasma in the field of Otolaryngology [3].
Keywords: regenerative medicine; platelet rich plasma; stem cell therapy; therapeutic potential; healing, growth factors
Introduction
Platelet Rich Plasma
Platelet-rich growth factor (GF)/ Platelet-rich fibrin matrix (PRF)/ Platelet _concentrate are the other names of Platelet rich plasma. Haematology started with the concept and description of PRP [4]. In 1970, haematologists created the term platelet-rich plasma so as to describe the plasma with platelet count above the peripheral blood used as a transfusion product for the treatment of thrombocytopenia [5]. PRP was first used in 1987 in an open-heart surgery ten years later, it started to be used in maxillofacial surgery as PRF. The haemostatic properties and ability of adherence was due to Fibrin. The cell proliferation was stimulated by the anti-inflammatory action of PRP [6]. With advancement, PRP was started to be used in the field of musculoskeletal system in sports injuries. The professional sportspersons experienced their early recovery hence PRP was attracted and widespread in the media and its uses grow exponentially. The other medical fields, namely Cardiology, Paediatric surgery, Gynaecology, Urology, Plastic surgery and Ophthalmology [7]. The recent interest of PRP is its application in dermatology, right from alopecia to skin rejuvenation, it has shown tremendous results due to its property of wound healing which revisions the scar and tissue regeneration [8]. PRP is nothing but a biological product having a fraction of plasma of autologous blood with a concentration of platelet above the baseline before centrifugation. The ability of action of PRP is due to the range of GFs, cytokines, chemokines plasma proteins along with high range of platelet and complement of clotting factors. In addition to high platelet levels, PRP requires consideration of other parameters such as the appearance of white blood cells and activation. It defines the type of PRP used in various pathologies. PRP preparation is made easier by a variety of commercially accessible instruments. The makers claim that PRP devices often obtain a PRP concentration that is 2–5 times higher than the baseline concentration. Based on the white blood cell and fibrin content, the production of platelet-rich plasma can be divided into four majors.
Categories
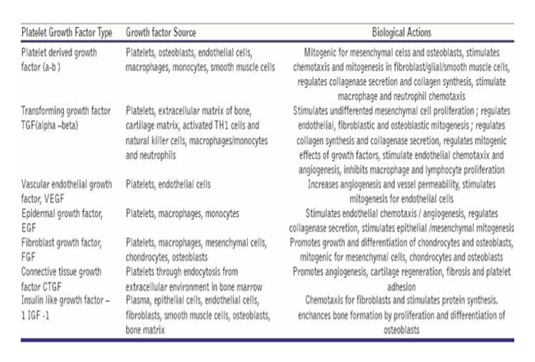
LEUKOCYTE-RICH PRP (L-PRP). WBC Reduced PRP (P-PRP); Leukocyte Platelet Rich Fibrin and Pure Platelet Rich Fibrin. The rationale for the use of PRP in tissue repair is the efficiency of these specific growth factors. Addition of thrombin and calcium chloride activates the collected platelets, thereby inducing the release of platelet growth factor, growth factor beta, fibroblast growth factor, insulin-like growth factors 1 and 2, vascular endothelial growth factor, Converts epidermal growth factor, interleukin-8, keratinocyte growth factor, binding tissue growth factor from alpha granules [9].
Method of Preparation
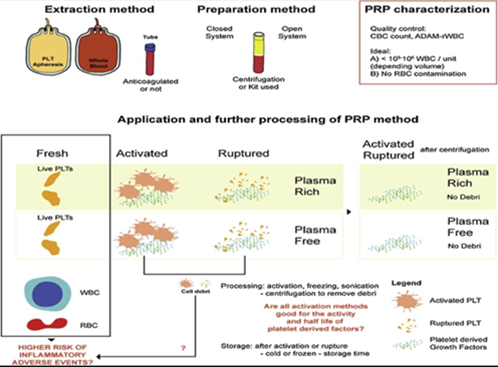
Figure 1: Scheme depicting applicable variables to keep in mind while describing PRP products. The additives related to destructive occasions also are highlighted (stay platelets, WBC -white blood cells, and RBC -purple blood cells-), which might be surely depending on the affected person subjacent circumstance or inflammatory state, and won't constantly pose hazard for destructive occasions.
Uses
With evidence of certain positive and negative effects, there is mixed evidence of benefit of PRP. It is shown to be tremendously effective in curing chronic tendinitis, osteoarthritis, and in Oral, faciomaxillary and plastic surgeries. Not only this but also according to a review in 2019, it is found useful in the rotator cuff disease. There is also evidence of its usefulness in osteoarthritis. Another meta-analysis made in 2019, found that in compared to hyaluronic acid, PRP is found more effective as an analgesic as well as improving function in osteoarthritis of knee [10]. Few randomized controlled trials in a review in the year 2009 evaluated that PRP was a definite promising treatment option for various orthopaedic illnesses such as treatment option for joints, ligament, tendon, muscle injuries such as lateral epicondylitis, muscle strain, Anterior cruciate ligament tears unless proven otherwise.[11]. More recently there are evidence showing positive effects of PRP in promoting the endometrial and follicular growth factors not only this but also it is found assisting in gestation and reproductive cycles [12]. Due to the release of growth factors and biologically active protein there occurs a cascade of mechanisms stimulating neo angiogenesis and production of collagen. Hence due to this property it can be used for facial rejuvenation in the form of dermal injection and as a topical applicant in micro needling [13]. In a literature review done in 2015, PRP has shown positive results as a treatment option in Lymphedema. However, they suggest a deeper level of study to apply this in a large scale [14].
There is no evidence of effectiveness of PRP in conservative management in disease such as plantar fasciitis, Achilles’ tendinopathy, based on a meta-analysis conducted in 2019. A Cochrane review in
2010 states that there is no clue of benefit in use of sinus lifts during dental implant placement. [15]. Keeping all these clinical uses aside, PRP has also been utilized greatly by the bio technicians in various tissue engineering applications in reference to bone, cartilage, akin and soft tissue repair. It has been serving as a source for delivery of growth factors or cells along with tissue engineered construction including bio materials.
Review
In several surgical specialities, Platelet-rich-plasma is an idiosyncratic substance that is frequently brought in use. Safety (because it is autologous material), enhanced platelet and growth factor deposition in the healing region, and quick preparation time are only a few of its many benefits.
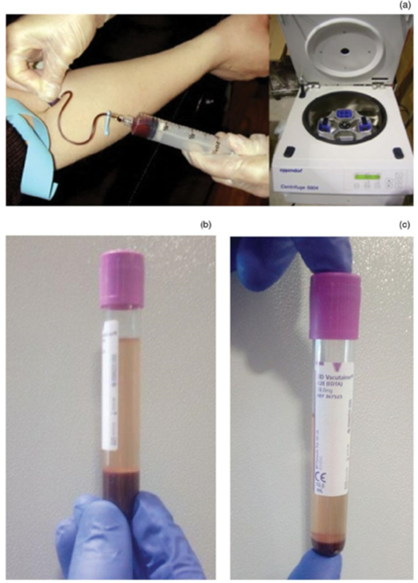
There is a slow development of research in PRP used in OTOLARYNGOLOGY, but it is surely easier to find. 10 years from now, a very renown clinical Practitioner attended a lecture on topical applications of PRP after ablative laser procedures. It was found that his patients had a lot of pain and needed a lot of time for healing. Surprisingly, with the application of PRP, they experienced less pain and improvement in healing time. He concluded that there were mostly opinion papers and non-randomized controlled trials then but now there is a broad spectrum of evidence on use of PRP in OTOLARYNGOLOGY and maxillofacial surgeries. It’s property of wound healing is the strongest evidence of its use. Dual speed centrifugation is the principal method of production of Platelet-rich plasma. The equipment needed for blood centrifugation is shown in Figure2a. There are two steps in the centrifugation. The first spin is a soft spin wherein blood is separates into red blood cells, platelet that is poor in plasma and a buffy coat. The second spin is termed as the hard spin where separation of platelet-rich plasma from the platelet poor plasma. The different layers produced by blood centrifugation is shown in figure2b. After these two steps of centrifugation, the platelet-rich plasma which was extracted after the spin is mixed with Calcium chloride and thrombin and there is formation of a gel like product. This product is 5-8% concentrated than the whole blood [16].
Figure 1
In addition to highly concentrated platelets, platelet-rich plasma contains a variety of growth factors beneficial for wound healing, including platelet-derived growth factor (PDGF), metabolic growth factor, and platelet-derived growth factor. Factors such as beta (TGF-β), epidermal growth factor (EGF), fibroblast growth factor (FGF), insulin-like growth factor, platelet-derived angiogenesis factor, as well as leukocytes, phagocytes, and high-concentration natural fibrinogen. In particular, PDGF and TNF promote haemostasis, scar reduction and faster wound healing. Platelet-rich plasma is an established treatment with promising results for a variety of medical conditions [17].
Table 1: Platelet Growth Factor and Their Specific Characteristics.
The healing capabilities of this substance make it particularly intriguing to ENT surgeons as a potential filling or grafting material. Plasma rich fibrin (PRF) is considered satisfactory in wound healing. PRF can increase the closure rate of acute perforations, enhance the survival rate of autografts in TM surgeries and reduce the incidence of infections. According to a case report in 2019, the introduction of platelet-rich plasma in treatment of Sensors Sensorineural hearing loss along with steroids and antioxidants is doing revolutionary wonder. Its application in ENT is not yet widespread, thus more research is necessary. The data on Using platelet-rich plasma in ENT surgery is discussed in this review.
Materials And Methods
A search was undertaken on the present and potential uses of platelet-rich plasma utilizing different publications linked to otolaryngology. It was conducted using the PubMed database. One such instance is a randomized controlled trial with 76 patients as the sample size. All patients diagnosed with persistent suppurative otitis media and under the age of 55 were scheduled for myringoplasty. By using block randomization, the individuals were divided into two groups at random (block of 4). Group II (n=38) was chosen as the control group and got saline-soaked gel foam intraoperatively. At the conclusion of the first and third months, a blinded examiner evaluated both groups. Group I (n=38) received platelet-rich plasma-soaked gel foam [18]. Another study was conducted on a group of 30 patients who had bilateral, generally symmetrical chronic rhinosinusitis that was unresponsive to any of the conservative management I.e., Medical treatment and would make them candidates for endoscopic sinus surgery. Patients with asymmetric disease or any additional confounding conditions were not taken into account. The procedure for the operation was followed as normal. In order to allow each patient to act as their own control, PRP was injected into the middle meatus on one randomly chosen n side following each treatment while the other side was treated normally [19]. A case series study in 2018 was carried out in the ENT department of Harsh hospital itself in Ghaziabad. The participants were the patients with reduced hearing loss and had complications of fullness of ear. They were evaluated with the essential investigation such as PTA, BERA. On the basis of audiogram, 200 patients were recognized having pure sensorineural and mixed hearing loss. Over a period of 1 year, study over 200 patients were covered. 0.5 ml injection of PRP were injected intratympanic ally in those 200 patients and it was repeated every 3 weeks along with comparative study of the audiogram with the previous preliminary audiograms. Among the 200 patients it was found that 172 had improvement in hearing after around five doses of the PRP injection. Although remaining 28 did not showed any improvement in hearing particularly. It should also be taken into account that all of them were above 70 years of age and 19 patients among them had diabetes as a predisposing factor [20]. In the year 2020, the year of COVID 19, another study was conducted in patients having olfactory loss of a duration more than 6 months with no evidence of sin nasal inflammatory disease and no history of improvement with olfactory training or topical agents. These patients were injected with intranasal PRP injection into the mucosa of olfactory cleft. The Sniff sticks olfactory test was conducted and observations were analysed up to 3 months. The results were quite impressive with improvement in symptoms [21]. On a study on osteonecrosis of the jaw which was mainly Related to Bisphosphonate commonly known as BRONJ. It was a case controlled randomized study in a group of 72 patients, all their treatment, surgical or non-surgical therapy was amplified by PRP gel for the observation of its effectiveness in osteonecrosis of Jaw. Due to its great wound healing capability, PRP showed amazing results. It’s provided definitive evidence in its wound healing properties [22]. According to research on the use of PRP in ENT Surgical procedures, it is particularly effective in myringoplasty. A retrospective study demonstrated that combining PRP with fat graft myringoplasty (FMG) improved the closure of tympanic membrane perforations compared to FMG alone. Additionally, topical autologous PRP treatment is safe, highly effective, and successful during myringoplasty, with no documented complications. PRP helps chronic TM perforations heal more quickly, but it also prevents infection and eliminates the need for an inner EAC pack [23]. The data extraction consists of a narrative overview of each article due to the wide variation of study methodology and result.
Results
After obtaining the full Articles, their relevance and abstracts were evaluated for the final result that could conclude the potential of PRP.
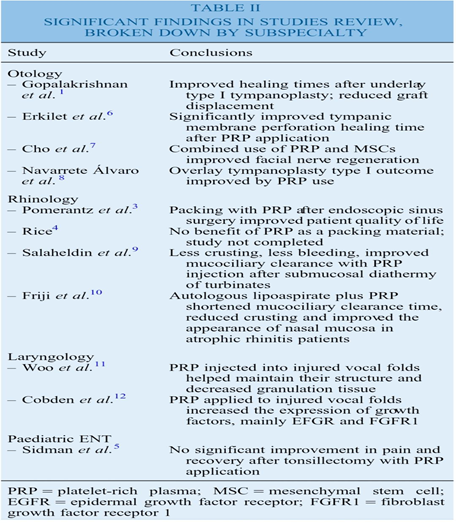
Use of platelet-rich plasma in otology surgery
Following bilateral tympanic membrane puncture in 44 rats, Arklie et al. reported in 2009 that platelet-rich plasma helped the membranes repair [24]. Navarrete lark et al. reported the preliminary outcomes of type I tympanoplasty supported by platelet-rich plasma for central perforations in 2001. After placing a platelet-rich plasma plug around three patients' dry perforations, they underwent overlay type I tympanoplasty [25]. In 2013, Gopalkrishnan et al. took into account the examination of 25 patients who went underlay tympanoplasty with the use of PRP and another control group of 25 patients who had tympanoplasty without PRP. The rates of closure of the perforation were 96% in the experimental group and 80% in the control group [26]. Cho et al. In the year 2010, inspected the effect of Platelet-rich_ plasma on the regeneration of ninth cranial nerve I.e., Facial nerve in 24 guinea Pigs. The group having Perineural microculture plus PRP and mesenchymal stem cells showed maximum myelinated axon Fibre group than the other ones [27].
Use of platelet-rich plasma in rhinology surgery
In order to cure atrophic rhinitis, Fiji et al. published a technique in 2014. They used autologous fat and platelet-rich plasma transplantation [28]. Pomerantz and Dutton in the year 2005 created a questionnaire series and compared the results with the control group in order to assess the lifestyle of 16- patients of all age group who underwent packing or filling with Platelet-rich plasma after the Endoscopic Sinus Surgery. Undoubtedly The PRP group outperformed the control group in terms of scores [29]. In 2006, Rice reported the same findings as Pomerantz and Dutton, he reported with the preliminary findings which were so impressive that strengthen the use of PRP in Ear packs. Following submucosal diathermy, Hussein and Salaheddin treated a herd of 30 patients in 2012 by injecting platelet-rich plasma into the inferior turbinate of the ear [30].
Use of platelet-rich plasma in laryngology surgery
Woo et al. (2014) examined the palliative effects of Platelet-rich plasma in Rabbits. They found that platelet-rich plasma appeared to preserve the wounded vocal fold's structure while reducing the production of granulation tissue [31]. In 2015, Cowden et al. Used various components of PRP such as EGF receptor, FGF, Fibroblast GF Receptor 1 etc in repairing the Vocal cord and they were found very effective in healing of the Vocal Fold Scar [32].
Use of platelet-rich plasma in not surgery
The results of tonsillectomy following the application of platelet-rich plasma to the tonsillar fossae were reported by Sidman et al. in 2008. No discernible alterations were found [33]. The conclusion of each study is summarised in table 2 [34].
Conclusion
The numerous types of studies of the platelet rich plasma in Ear Nose Throat commonly known as otolaryngology surgery. When compared to the enormous uses of this significant material, the number of studies will always be ‘Not Enough’. Every single article mentioned in the above had different experimental and control groups, each sharing some similarities as well in the methods of techniques and evaluation. It cannot be precisely oncluded, with the broad-spectrum uses of platelet-rich plasma how much essential is the wield of Platelet-rich plasma in the surgery of Ear Nose Throat Surgeries as some of the drawbacks included limitations in the aggregation participants and remissness to nurture a close delving up or some errors in the study design. Undoubtedly, Platelet-rich plasma is a boon for modern medicine with enormous potential clinical applications. The mechanism by which it aids healing process, by the promotion of growth factors aggregation is included in this review. The various surgeries of Otology, rhinology and laryngology and its effectiveness in various processes during the entire surgery, is compiled in this review. "Sometimes you have to go far to find what is close." For platelet-rich plasma (PRP) as we currently understand it, Paulo Coelho's adage still holds true. Although much progress has been made in our knowledge of this "Youth" in blood, there still appears to be much to learn. Despite advancements, understanding on its preparation, biology, and end product's qualities continues to elude scientists.
References
- Edgar L, Pu T, Porter B, Aziz JM, La Pointe C, Asthana A, Orlando G. (2020). Regenerative medicine, organ bioengineering and transplantation. Br J Surg, 107(7):793-800.
Publisher | Google Scholor - Umezawa A. (2016). [REGENERATIVE MEDICINE]. Arerugi, 65(8):987-989.
Publisher | Google Scholor - Pensato R, La Padula S. (2022). The use of platelet-rich plasma in aesthetic and regenerative medicine: A comprehensive review. Aesthetic Plast Surg.
Publisher | Google Scholor - Stavrakas, Marios & Karkos, P & Markou, Konstantinos & Grigoriadis, Nikolaos. (2016). Platelet-rich plasma in otolaryngology. The Journal of Laryngology & Otology, 130.
Publisher | Google Scholor - Althaus K, Pelzl L, Hidiatov O, Amiral J, Marini I, Bakchoul T. (2019). Evaluation of a flow cytometer-based functional assay using platelet-rich plasma in the diagnosis of heparin-induced thrombocytopenia, 180:55-61.
Publisher | Google Scholor - Chiou C-S, Wu C-M, Dubey NK, Lo W-C, Tsai F-C, Tung TDX, et al. (2018). Mechanistic insight into hyaluronic acid and platelet-rich plasma-mediated anti-inflammatory and anti-apoptotic activities in osteoarthritic mice. Aging, 10(12):4152-4165.
Publisher | Google Scholor - Boivin J, Tolsma R, Awad P, Kenter K, Li Y. (2021). The biological use of platelet-rich plasma in skeletal muscle injury and repair. Am J Sports Med.
Publisher | Google Scholor - Stamatiou C, Daunert S, Jimenez J. 573 A review of the use of platelet rich plasma for the treatment of androgenic alopecia. J Invest Dermatol, 138(5):97.
Publisher | Google Scholor - Dohan Ehrenfest DM, Andia I, Zumstein MA, Zhang C-Q, Pinto NR, Bielecki T. (2014). Classification of platelet concentrates (Platelet-Rich Plasma-PRP, Platelet-Rich Fibrin-PRF) for topical and infiltrative use in orthopedic and sports medicine: current consensus, clinical implications and perspectives. Muscles Ligaments Tendons J, 4(1):3-9.
Publisher | Google Scholor - Bachelor LP, Bachelor YX, Li T, Li Y, Zhu J, Tang X. (2022). Platelet-rich plasma injection can be a viable alternative to corticosteroid injection for conservative treatment of rotator cuff disease: A meta-analysis of randomized controlled trials. Arthroscopy.
Publisher | Google Scholor - Everts P, Onishi K, Jayaram P, Lana JF, Mautner K. (2021). Platelet-Rich Plasma: New Performance Understandings and Therapeutic Considerations in 2020. Int J Mol Sci. 21(20):7794.
Publisher | Google Scholor - Sharara FI, Lelea LL, Rahman S, Klebanoff JS, Moawad GN. (2021). A narrative review of platelet-rich plasma (PRP) in reproductive medicine. J Assist Reprod Genet, 38(5):1003-1012.
Publisher | Google Scholor - Sclafani AP, Azzi J. (2015). Platelet preparations for use in facial rejuvenation and wound healing: a critical review of current literature. Aesthetic Plast Surg, 39:495-505.
Publisher | Google Scholor - Akgül A, Cirak M, Birinci T. (2016). Applications of Platelet-Rich Plasma in Lymphedema. Lymphat Res Biol, 14(4):206-209.
Publisher | Google Scholor - Madhi MI, Yausep OE, Khamdan K, Trigkilidas D. (2022). The use of PRP in treatment of Achilles Tendinopathy: A systematic review of literature. Study design: Systematic review of literature. Ann Med Surg, 55:320-326.
Publisher | Google Scholor - Attia S, Narberhaus C, Schaaf H, Streckbein P, Pons-Kühnemann J, Schmitt C, et al. Long-term influence of platelet-rich plasma (PRP) on dental implants after maxillary augmentation: Retrospective clinical and radiological outcomes of a randomized controlled clinical trial. J Clin Med [Internet]. 2020 [cited 2022 Jul 23];9(2):355.
Publisher | Google Scholor - Stavrakas, Marios & Karkos, P & Markou, Konstantinos & Grigoriadis, Nikolaos. (2016). Platelet-rich plasma in otolaryngology. The Journal of Laryngology & Otology, 130:1098-1102.
Publisher | Google Scholor - Bava ED, Barber FA. (2011). Platelet-rich plasma products in sports medicine. Phys Sportsmed. 39(3):94-99.
Publisher | Google Scholor - Gökçe Kütük S, Özdaş T. (2019). Impact of platelet-rich fibrin therapy in tympanoplasty type 1 surgery on graft survival and frequency-specific hearing outcomes: a retrospective analysis in patients with tympanic membrane perforation due to chronic otitis media. J Laryngol Otol, 133(12):1068-1073.
Publisher | Google Scholor - Sari H, Karaketir S, Kumral TL, Akgun MF, Gurpinar B, Hanci D, Berkiten G, Uyar Y. (2021). The effect of platelet-rich fibrin (PRF) on wound healing, adhesion, and hemostasis after endoscopic sinus surgery in patients with nasal polyposis. Am J Otolaryngol., 42(5):103010.
Publisher | Google Scholor - Bajpai S. (2019). Study on use of platelet-rich plasma in myringoplasty. In: 27th Annual National Conference of the Indian Society of Otology. Thieme Medical and Scientific Publishers Private Ltd.
Publisher | Google Scholor - Hassan O, Ibrahim M, ElFarouka A, El Garem A. Platelet-rich plasma nasal packing in endoscopic sinus surgery. Pan Arab Journal of Rhinology. 2020;10(2):94.
Publisher | Google Scholor - Cardoso CL, Curra C, Curi MM, Matsumoto MA, Argentino CD, Franzolin SOB, Constantino D, Barbosa DN, Ferreira Júnior O. (2019). Treatment of bisphosphonate-related osteonecrosis using platelet-rich plasma: microtomographic, microscopic, and immunohistochemical analyses. Braz Oral Res, 33:50.
Publisher | Google Scholor - Huang J, Shi Y, Wu L, Lv C, Hu Y, Shen Y. (2022). Comparative efficacy of platelet-rich plasma applied in myringoplasty: A systematic review and meta-analysis. PLoS One, 16(1):0245968.
Publisher | Google Scholor - Erkilet E, Koyuncu M, Atmaca S, Yarim M. (2009). Platelet-rich plasma improves healing of tympanic membrane perforations:experimental study. J Laryngol Otol, 123:482.
Publisher | Google Scholor - Gopalakrishnan S, Venkatasamy P, Vivekanandamurthy K. (2013). A study on efficacy of autologous platelet rich plasma in myringoplasty. Online J Otolaryngol, 3:36-51.
Publisher | Google Scholor - Cho HH, Jang S, Lee SC, Jeong HS, Park JS, Han JY et al. (2010). Effect of neural‐induced mesenchymal stem cells and platelet‐rich plasma on facial nerve regeneration in an acute nerve injury model. Laryngoscope, 120:907-913.
Publisher | Google Scholor - Friji M, Gopalakrishnan S, Verma S, Parida P, Mohapatra D.New regenerative approach to atrophic rhinitis using autologous lipoaspirate transfer and platelet‐rich plasma in five patients: our experience. Clinical Otolaryngol, 39:289-292.
Publisher | Google Scholor - Pomerantz J, Dutton JM. (2005). Platelet gel for endoscopic sinus surgery. Ann Otol Rhinol Laryngol, 114:699-704.
Publisher | Google Scholor - Rice DH. (2006). Platelet-rich plasma in endoscopic sinus surgery. Ear Nose Throat J, 85:516.
Publisher | Google Scholor - Salaheldin AH, Hussein A. Effect of platelet-rich plasma on nasal mucociliary clearance after submucous diathermy of inferior turbinate. EJENTAS, 13:71-75.
Publisher | Google Scholor - Woo SH, Jeong H-S, Kim JP, Koh E-H, Lee SU, Jin SM et al. (2014). Favorable vocal fold wound healing induced by platelet-rich plasma injection. Clin Exp Otorhinolaryngol, 7:4752.
Publisher | Google Scholor - Cobden SB, Oztürk K, Duman S, Esen H, Aktan TM, Avunduk MC et al. (2015). Treatment of acute vocal fold injury with platelet-rich plasma. J Voice.
Publisher | Google Scholor - Sidman JD, Lander TA, Finkelstein M. (2008). Platelet‐rich plasma for pediatric tonsillectomy patients. Laryngoscope, 118:1765-1767.
Publisher | Google Scholor - Stavrakas, Marios & Karkos, P & Markou, Konstantinos & Grigoriadis, Nikolaos. (2016). Platelet-rich plasma in otolaryngology. The Journal of Laryngology & Otology, 130. 1098-1102.
Publisher | Google Scholor