Research Article
Unsafe Abortion Presentation and Management Outcome Among Sudanese Women
1Specialist of Obstetrical & Gynecology, Sudan Medical Specialization Board, Sudan.
2Consultant Obstetrician &Gynecologist, Faculty of Medicine, Al Neelain University, Sudan.
*Corresponding Author: Awadalla Abdelwahid, Consultant Obstetrician &Gynecologist, Faculty of Medicine, Al Neelain University, Sudan.
Citation: B. Abdeen, A. Abdelwahid, H. Suliman. (2024). Unsafe Abortion Presentation and Management Outcome Among Sudanese Women, Journal of Women Health Care and Gynecology, BioRes Scientia Publishers. 3(1):1-10., DOI: 10.59657/2993-0871.brs.24.026
Copyright: © 2024 Awadalla Abdelwahid, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: December 20, 2023 | Accepted: January 10, 2024 | Published: January 15, 2024
Abstract
Background: Complications of unsafe abortion remain high in developing countries with a significant morbidity rate and the potential for maternal death. Developing countries need to legalize abortion and improve the care system to reduce abortion-related maternal deaths.
Purpose: The main purpose of the study was to determine the prevalence, methods, complications, and management outcomes of unsafe abortion at Bashair Teaching Hospital.
Methodology: It was a descriptive, cross-sectional hospital-based study conducted at Bashair Teaching Hospital from October 2021 to March 2022. Data was collected by trained doctors in the emergency clinic and postoperative gynaecology ward. One hundred and twenty-two (122) women with unsafe abortions were included after informed consent.
Results: The prevalence of unsafe abortion was 9.2%. The onset of bleeding was spontaneous in 106(89.9%) and induced in 16(13.1%). The method of induction of abortion was herbal 7(5.7%), drug 4(3.3%), trauma to abdomen 3(2.5%) and manipulation by foreign body 2(1.6%). The duration of bleeding was 1-2 days 63(51.6%), between 3-5 days 38(31.1%) and more than 5 days 21(17.3%). The complications were shock 19(15.6%), septicaemia 15(12.3%) and uterine perforation 6(4.9%). Discharge well 97(79.5%), discharged after admission to the intensive care unit were23(18.9%), and 2(1.6%) were died.
Conclusions: Unsafe abortion women presented with significant severe bleeding, shock, septicaemia, and fever. The foreign body causes uterine perforation and internal bleeding, so women need laparotomy and blood transfusion. admission to the intensive care unit is high. Maternal death is due to massive bleeding and septicaemia.
Keywords: unsafe; abortion; presentation; management; outcome; Sudanese; women
Introduction
An unsafe abortion is completely avoidable. It is still a pandemic and a significant global public health concern [1]. According to the World Health Organization (WHO), an unsafe abortion is performed by someone who lacks the essential skills, takes place in a setting that does not meet the bare minimum of medical standards, or both [2].
Unsafe abortion is a healthcare issue that underdeveloped nations frequently ignore. Unsafe abortion practices have virtually not improved despite advances in medical technology. One of the main factors contributing to maternal morbidity and mortality is unsafe abortion [3]. Abortion is more prevalent in Sub-Saharan Africa, where it is typically illegal, dangerous, and contributes significantly to maternal death [4]. Around the world, a significant proportion of women pass away from childbirth and pregnancy-related problems, with low- and middle-income nations accounting for nearly 99.0% of the total [5]. Abortion is one of the leading causes of maternal death. The study found that abortion was responsible for 7.9% of maternal deaths that occurred between 2003 and 2009 in 115 different nations. The number of abortion-related deaths is probably underreported; therefore, it might be higher [6]. Unsafe abortion is one of the main causes of maternal death in low- and middle-income countries, among other things. Abortion can happen naturally or purposely; the latter is also referred to as induced abortion and can be safe or harmful. Abortion (particularly unsafe abortion) can have negative effects on one's health and lead to issues like hemorrhage, infection, and uterine perforation [7].
From 2003 to 2008, the global abortion rate remained stable at 2829/1000 women aged 1544 years, but the percentage of unsafe abortions grew from 44.0% to 49.0% [8]. Due to stringent anti-abortion laws in many South Asian nations, the rate of unsafe abortions is quite high in South Asia (which makes up about one-third of the world's population). Due to the preference for a male kid, the rate of sex-selective abortion is also high in this area [9-10]. Most dangerous abortions take place in impoverished nations where it is forbidden, where access to inexpensive, skilled healthcare providers is limited, or where modern birth control is not widely available [11-14].
According to the World Health Organization (WHO), nearly all abortions (92%) are safe in industrialized regions, whereas more than half (55%) are dangerous in developing nations. According to other sources, unsafe abortion causes at least 8% of maternal fatalities and has a risk rate of 1/270, according to WHO statistics. Induced abortions are dangerous in 48% of cases worldwide [15]. Unsafe abortion techniques include using a sharp tool or wire (such as an unbent clothes hanger or knitting needle) to try to break the amniotic sac inside the uterus. This technique has the potential to kill by infecting or damaging internal organs, such as the uterus or intestine. Using a huge feather was one of the classic methods since the uterus relaxes during pregnancy and is very simple to puncture [16-19].
Injecting the woman's body with harmful substances including chili pepper mixes and chemicals like alum, Lysol, permanganate, or plant poison. The woman can experience toxic shock and die as a result of this technique [20-21]. Unsafe abortion can result in death and damage to women all around the world [22-24]. Medical care is something that is legally mandated to be given to patients because it could save their lives. Doctors are required by law to report cases of patients who have had any kind of abortion. The risks to women's lives and health increase with every delay in care [25-26].
Material and Methods
It was a descriptive prospective cross-sectional hospital-based study conducted at Bashair Teaching Hospital from October 2021 to March 2022. The Study population that was included all women diagnosed with unsafe abortion who came during the study period to the gynecology clinic and emergency room, and they agreed to participate in the study. About 122 women who were diagnosed with unsafe abortions were included. Convenience non-random technique was applied to select the study participants by including all the cases throughout the data collection period (6 months) convenience non-random technique was applied to select the study participants by including all the cases throughout the data collection period (6 months).
Data was collected by direct interview by using a well-structured questionnaire. The participants were interviewed about age, education, gestational age, parity, symptoms of presentation, type of management, and complications.
Statistical analysis was performed via SPSS software (SPSS, Chicago, IL, USA). Continuous variables were compared using the student’s t-test (for paired data) or the Mann–Whitney U test for nonparametric data. For categorical data, a comparison was done using the Chi-square test (X2) or Fisher’s exact test when appropriate. A P-value of less than 0.05 was considered statistically significant.
Written ethical clearance and approval for conducting this research were obtained from the Educational Development Centre (EDC), the ethical committee, and from Sudan Medical Specialization Board Ethical Committee. Written permission was obtained from the administrative authority of Bashair Teaching Hospital, Khartoum state, Sudan. Written consent was obtained from the study participants after a full explanation of the study-related issues and implications. Study data/information was used for research purposes only. The privacy issues were intentionally considered. Confidentiality of participants' data was considered by coding the questionnaire.
Results
During the study period total number of women admitted to the gynecological department of the hospital was 1319, and 122 were diagnosed with unsafe abortion so the incidence of unsafe abortion is found (122/1319) in approximately 9.2% of all early pregnancy women. Sociodemographic distribution of unsafe abortion, Women aged most below ≤ 19 years were 56.6% while lest distribution between 31 – and 40 years was 10.6%. Most women were housewives 52.5%, and their educational level.
Most were Illiterate women 46.7%, The women from rural areas were 63.9% while from urban areas were 36.1%, 90.2% were married, 5.7% were unmarried, 2.5% were divorced, and 1.6% were widowed. Most women were multipara women 52.5%, primigravida 39.3% and grand multipara 8.2%. Table 1.
Table 1: Sociodemographic characteristics of Unsafe Abortion (n=122).
| Sociodemographic | Frequency | Percent |
| Age <19> | 69 | 56.6 |
| 20-30 | 16 | 13.1 |
| 31-40 | 13 | 10.6 |
| >40 | 24 | 19.7 |
| Occupation | ||
| Housewife | 64 | 52.2 |
| Laborer | 33 | 27 |
| Employee | 20 | 16.4 |
| Professional | 5 | 4.1 |
| Education | ||
| Illiterate | 57 | 46.7 |
| Primary school | 33 | 27 |
| Secondary school | 17 | 13.9 |
| University | 15 | 12.4 |
| Residence | ||
| Rural | 78 | 63.9 |
| Urban | 44 | 36.1 |
| Marital status | ||
| Married | 110 | 90.2 |
| Unmarried | 7 | 5.7 |
| Divorced | 3 | 2.5 |
| Wido | 2 | 1.6 |
| Gravity | ||
| Primigravida | 48 | 39.3 |
| Multiparous | 64 | 52.5 |
| Grand Multiparous | 10 | 8.2 |
| Total | 122 | 100 |
All women presented with vaginal bleeding, 45(36.9%) fever, 44(36.1%) offensive vaginal discharge, 37(30.3%) abdominal pain and 29(23.8%) expulsion of tissue Table 2.
Table 2: Unsafe abortion symptoms of presentation (n=122).
| Presentations | Had symptoms | Not had symptoms | Total | |||
| N | % | N | % | N | % | |
| Vaginal bleeding | 122 | 100.0 | 0 | 0.0 | 122 | 100 |
| Fever | 45 | 36.9 | 77 | 63.1 | 122 | 100 |
| Vaginal discharge (offensive) | 44 | 36.1 | 78 | 63.9 | 122 | 100 |
| Abdominal pain | 37 | 30.3 | 85 | 69.7 | 122 | 100 |
| Expulsion of tissue | 29 | 23.8 | 93 | 76.2 | 122 | 100 |
The duration of bleeding was 1-2 days 63(51.6%) had shock 4(6.3%), septicemia 1(1.6%), uterine perforation 2(3.2%) and no complication 56(88.9%), between 3-5 days 38(31.1%) had shock 5(13.2%), septicemia 10(26.3%), uterine perforation 2(5.3%) and no complication 21(55.3%) and more than 5 days 21(17.3%) had shock 10(47.6%), septicemia 4(19%), uterine perforation 2(9.2%) and no complication 5(23.8%). The estimated amount of bleeding was severe 43(35.2%), had shock17(39.5%), septicemia 13(30.2%), uterine perforation 6(14%) and no complication 7(16.3%), moderate 40(32.8%) had shock 2(5%), septicemia 2(5%), no uterine perforation and no complication 36(90%) and minimal 39(32%) no complication 39(100%) Table 3.
Table 3: Unsafe abortion complications about the duration and degree of bleeding (n=122).
| Complications | Duration of Vaginal Bleeding | P-value | ||||||
| 1 - 2 days | 3 -5 days | > 5 days | ||||||
| N | % | N | % | N | % | |||
| Shock (hemorrhage) | 4 | 6.3 | 5 | 13.2 | 10 | 47.6 | ||
| Septicemia | 1 | 1.6 | 10 | 26.3 | 4 | 19.0 | 0.019 | |
| Uterine perforation | 2 | 3.2 | 2 | 5.3 | 2 | 9.5 | ||
| No complications | 56 | 88.9 | 21 | 55.3 | 5 | 23.8 | ||
| Complications | Degree of Vaginal Bleeding | |||||||
| Minimal | Moderate | Severe | ||||||
| N | % | N | % | N | % | |||
| Shock (hemorrhage) | 0 | 0.0 | 2 | 5.0 | 17 | 39.5 | ||
| Septicemia | 0 | 0.0 | 2 | 5.0 | 13 | 30.2 | 0.014 | |
| Uterine perforation | 0 | 0.0 | 0 | 0.0 | 6 | 14.0 | ||
| No complications | 39 | 100.0 | 36 | 90.0 | 7 | 16.3 | ||
| Total | 39 | 100.0 | 40 | 100.0 | 43 | 100.0 | ||
Poor outcome of unsafe abortion (admission to intensive care unit and death) was significantly associated with duration of bleeding 3 days or more, severe amount of bleeding, and complications such as shock and septicemia (P value < 0> 6 days (12(12.4%), had minimal bleeding (39(40.2%), moderate bleeding 38(39.2%), severe bleeding 20(20.6%), 23(18.9%) discharged after admission to the intensive care unit had a duration of vaginal bleeding1-2days5(21.7%),3-5days 10(43.7%%),>6days 8(34.8%), no woman had minimal bleeding, moderate bleeding 2(8.7%), severe bleeding 21(91.3%), and 2(1.6%) died 1(50%) had bleeding >6days and1(50%) bleeding 3-5days both had severe vaginal bleeding. Table 4.
Table 4: Unsafe abortion outcome about the duration and degree of bleeding (n=122).
| Duration of vaginal bleeding | Outcome | P-value | |||||
| Discharged well | Admitted to ICU | Death | |||||
| N | % | N | % | N | % | ||
| 1 - 2 days | 58 | 59.8 | 5 | 21.7 | 0 | 0.0 | |
| 3 -5 days | 27 | 27.8 | 10 | 43.5 | 1 | 50.0 | 0.011 |
| > 6 days | 12 | 12.4 | 8 | 34.8 | 1 | 50.0 | |
| Total | 97 | 100.0 | 23 | 100.0 | 2 | 100.0 | |
| Degree of vaginal bleeding | Outcome | ||||||
| Discharged well | Admitted to ICU | Death | |||||
| N | % | N | % | N | % | ||
| Minimal | 39 | 40.2 | 0 | 0.0 | 0 | 0.0 | |
| Moderate | 38 | 39.2 | 2 | 8.7 | 0 | 0.0 | 0.001 |
| Severe | 20 | 20.6 | 21 | 91.3 | 2 | 100.0 | |
| Total | 97 | 100.0 | 23 | 100.0 | 2 | 100.0 | |
Outcome of unsafe abortion after management discharge well 97(79.5%) shock 4(4.1%), septicemia 5(5.2%), uterine perforation 6(6.2%) and no complications 82(84.5%), admitted to ICU 23(18.8%) shock 14(60.9%), septicemia 9(39.1%), no uterine perforation and no complications, death 2(1.6%) shock 1(50%) and septicemia 1(50%). The complications of unsafe abortion among the women in this study were significantly common in women with a duration of bleeding 3 days or more and a severe amount of bleeding (P value less than 0.01). Table 5.
Table 5: Unsafe abortion outcome about complications (n=122).
| Complications | Outcome | P-value | |||||
| Discharged well | Admitted to ICU | Death | |||||
| N | % | N | % | N | % | ||
| Shock (hemorrhage) | 4 | 4.1 | 14 | 60.9 | 1 | 50.0 | |
| Septicemia | 5 | 5.2 | 9 | 39.1 | 1 | 50.0 | 0.014 |
| Uterine perforation | 6 | 6.2 | 0 | 0.0 | 0 | 0.0 | |
| No complications | 82 | 84.5 | 0 | 0.0 | 0 | 0.0 | |
| Total | 97 | 100.0 | 23 | 100.0 | 2 | 100.0 | |
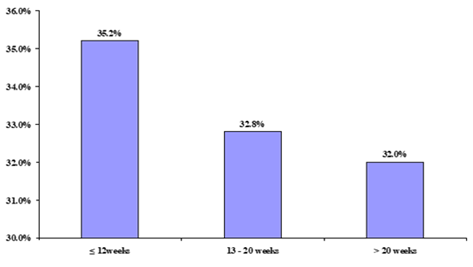
The gestational age at presentation was less than or equal to 12 weeks 43(35.2%), between 13 – 20 weeks 40(32.8%) and more than 20 weeks 39(32%) Figure 1.
Figure 1: Unsafe abortion gestational age at presentation distribution (n=122).
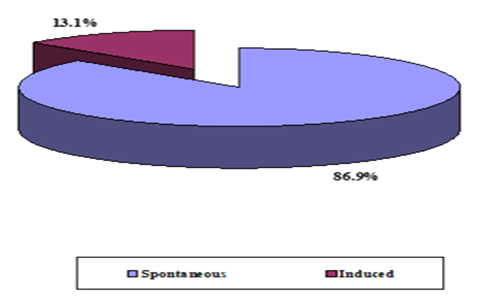
The onset of bleeding was spontaneous in 106(89.9%) and induced in 16(13.1%) Figure 2.
Figure 2: Unsafe abortion onset of bleeding distribution(n=122).
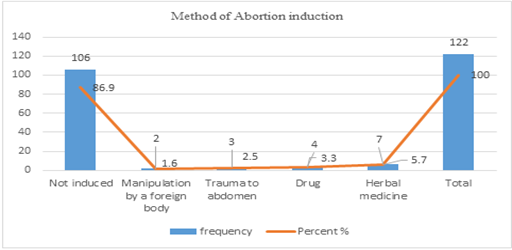
The method of induction of abortion was herbal 7(5.7%), drug 4(3.3%), trauma to abdomen 3(2.5%) and manipulation by foreign body 2(1.6%) Figure 3.
Figure 3: Unsafe abortion method of induction (n=122).
Discussion
This study found the prevalence of unsafe abortion in this setting during the study period was 9.2%, which is lower than Ngowa, et al [27] in Cameron who reported that the prevalence of unsafe abortion was 26.3%. According to Fusco et al's estimation of the incidence of hazardous abortion in Brazil, the five-year prevalence of abortion was 21.1% among women of reproductive age who had ever terminated a pregnancy, and 16.0% of all abortions were unsafe [28]. This study found a prevalence rate of 24.8% of abortions, which is high [29]. In Brooke et al study, abortion incidence complications methodology was used to estimate levels of induced abortion in Malawi. e. It was estimated that 70,194 induced abortions (range 50,696-89,692) occurred in Malawi in 2009, yielding an abortion rate of 24.0 abortions per 1000 women aged 15-44 (range 17.4-30.7) [30]. All women presented with vaginal bleeding, 36.9% of women presented with fever, 36.1% with offensive vaginal discharge,30.3% presented with abdominal pain, and 23.8% presented with the expulsion of tissue. Similar to Melese et al in Ethiopia [31-32]. Based on varying socioeconomic levels, this study found significant disparities in unsafe abortion procedures. For instance, there is a strong correlation between unsafe abortion and women who work as housewives and have only received an elementary education. These results were consistent with research from Brazil [33] and Mexico [34], where it was discovered that low-income and uneducated women were more likely to undergo unsafe abortions. The legality of abortion differed from state to state in Mexico; Mexico City allows abortions up to 13 weeks gestation, but Brazil allows abortions if the pregnancy was brought on by rape or incest or if the mother's or the fetus' lives were in danger [35].
The method of inducing abortion was herbal 5.7%, drug 3.3%, trauma to the abdomen 2.5%, and manipulation by a foreign body 1.6%. The commencement of bleeding was spontaneous in 89.9% of cases and induced in 13.1% of cases. Contrary to Melese et al.'s findings, which indicated that 3.9% of abortions were patient-induced, the majority of abortions (95.5%) were found to be spontaneous. Eighty-two women, or 67.2%, reported no complications. Shock (15.6%), septicemia (12.3%), and uterine perforation (6(4.9%)) were the consequences. With mild to severe vaginal bleeding, unsafe abortion patients with prolonged vaginal bleeding have a likelihood ratio of 17.812 and a 95% confidence interval of.093(.053-.164) to present with septicemia. 90.954 percent chance of septicemia in women with a Likelihood Ratio of 22.643 95% Confidence interval (CI) of 11.700(6.468-21.164) for septicemia discharge. Unsafe abortion for intensive care unit (ICU) admission, women with septicemia had a likelihood ratio of 44.051 95% CI 18.833(8.645-41.028). The likelihood ratio between septicemia and maternal death is 4.252,95 % The Congo study's [36] Confidence Interval of 8.643(5.281-14.144) is comparable. Another study revealed that induced abortion-related complications among women who were hospitalized included retained fetal products (50%) as well as bleeding (34%), fever (34%), and other symptoms similar to [37]. The majority of the women had successful outcomes, with 79.5
Strength and Limitations
One of the study's limitations was the fact that only one hospital's data was collected. However, the hospital is unable to offer thorough postabortion treatment since it receives complex cases from other medical facilities. Another drawback was the small number of cases that were found. In our study, the death rate from unsafe abortions was 1.6%, which is less than in other studies. The fact that accessing hospitals in Sudan that perform unsafe abortions is stigmatized to a high degree and that hospitalization leads to a police report because abortion is illegal may be the cause of this. As a result, women may not seek medical attention or may hide the fact that they had an abortion.
Conclusion
According to the study, the three worst consequences include substantial morbidity from unsafe abortion, septicaemia, and uterine perforation. Both the likelihood of maternal mortality and ICU admission are very high. The provision of safe abortion services is not supplied owing to religion; hence contraception should be accessible to help reduce unsafe abortion practices in Sudan. It took a hospital setting and qualified medical staff to manage unsafe abortion consequences like shock, extensive vaginal bleeding, septicaemia, and uterine perforation. Among unsafe abortions, the practice of blood transfusion is lifesaving. When healthcare providers give their patients the best possible care, positive results are attained.
Recommendation
There is a need for health education for women of reproductive age about the urgency of seeking instant care after notice of any signs of unsafe abortion. There is a need for clinical audits on post-abortion care to ensure the implementation of the standard protocol and reduce complications. For managing women who present with unsafe abortion doctors should have and maintain a high index of suspicion that unsafe abortion may have occurred and be alert to the possibility of delayed presentation and rapid decompensation patient may be near missed, early use of intravenous broad-spectrum antibiotic and antipyretics will reduce septicaemia and hyperpyrexia complications, availability of ICU for unsafe abortion and trained staff for early intervention, health worker training and community education. Also, postabortion care services should be available in hospitals, and auditing of the practice of outcomes of unsafe abortion.
Declarations
This article is our original work. The Submitted manuscripts contain original and authentic results, data, and ideas, that were not published elsewhere. No material from other publications is reproduced in our article. All my co-authors should not submit the same manuscript, in the same language simultaneously to more than one journal. The author of this paper has read and approved the final version submitted.
Ethical clearance
Ethics approval was obtained from the Research and Ethics Committee of the hospital (Bashair Teaching Hospital). Ethical principles of autonomy, beneficence, non-maleficence, and justice, as stipulated in the ethical guidelines of the Sudan Medical Specialization Board (SMSB), and Medical Research Council, were upheld throughout the study. Informed written consent was obtained from every respondent who agreed to participate in the study.
Availability of data and materials
All data and materials are available when requested.
Competing interest
The authors declare that they have no financial or personal relationships which may have inappropriately influenced them in writing this paper. No direct or indirect financial interests or conflicts exist and all authors agreed with the content of the manuscript and there are no conflicts of interests between or among them.
Funding
My research project was self-sponsored by me and with the help of my colleagues and co-authors. There was no funding from any institute or organization for this paper.
Authors contribution
All my authors play major roles and real contributions to achieve this project. Bashir Abdeen, Awadalla Abdelwahid, and Hajar participated in data collection and analysis and participated in the manuscript plan, editing, and writing of the article.
Acknowledgments
The authors would like to acknowledge and thank Yousif Suliman Ibrahim for his effort in design, data analysis, and the interviewers for their invaluable contribution to this work, as well as the respondents for their participation in this study.
Abbreviations
CI: Confidence Interval
ICU: Intensive Care Unit
WHO: World Health Organization
Copyrights
Authors agreed to transfer the copyrights to the publisher as soon as the article is accepted for publication under the relevant license which permits to distribution, reprocessing, and or reprint of the published work. Under the license, the transfer of rights includes material such as tables, figures, supplementary data, and any part of the article that can be reused. Authors retain patent, trademark, and IP rights including the original findings of their work.
In case of a replica of any published work or a part of it such as figures/tables/text, etc. corresponding author is a reliable person to obtain the copyrights from the previous publisher. It is obligatory to state the copyright transference evidence wherever necessary and make sure that cited properly.
References
- Rehnström Loi, U., Gemzell-Danielsson, K., Faxelid, E., & Klingberg-Allvin, M. (2015). Health care providers’ perceptions of and attitudes towards induced abortions in sub-Saharan Africa and Southeast Asia: a systematic literature review of qualitative and quantitative data. BMC Public Health, 15(1).
Publisher | Google Scholor - World Health Organization. (2017). HRP annual report 2016 (No. WHO/RHR/HRP/17.06). World Health Organization.
Publisher | Google Scholor - World Health Organization. (2016). Interagency list of medical devices for essential interventions for reproductive, maternal, newborn, and child health.
Publisher | Google Scholor - Kulczycki, A. (2016). The imperative to expand provision, access, and use of misoprostol for post-abortion care in sub-Saharan Africa. African journal of reproductive health, 20(3):22-25.
Publisher | Google Scholor - World Health Organization. (2015). Trends in maternal mortality: 1990-2015: estimates from WHO, UNICEF, UNFPA, World Bank group and the United Nations population division. World Health Organization.
Publisher | Google Scholor - Say, L., Chou, D., Gemmill, A., Tunçalp, Ö., Moller, A. B., Daniels, J., ... & Alkema, L. (2014). Global causes of maternal death: a WHO systematic analysis. The Lancet Global Health, 2(6):323-333.
Publisher | Google Scholor - Meaidi, A., Friedrich, S., Gerds, T. A., & Lidegaard, O. (2019). Risk factors for surgical intervention of early medical abortion. American journal of obstetrics and gynecology, 220(5):478.
Publisher | Google Scholor - Sedgh, G., Singh, S., Shah, I. H., Åhman, E., Henshaw, S. K., & Bankole, A. (2012). Induced abortion: incidence and trends worldwide from 1995 to 2008. The Lancet, 379(9816):625-632.
Publisher | Google Scholor - Valente, C. (2014). Access to abortion, investments in neonatal health, and sex-selection: Evidence from Nepal. Journal of Development Economics, 107:225-243.
Publisher | Google Scholor - World Health Organization. (2003). Safe abortion: technical and policy guidance for health systems. World Health Organization.
Publisher | Google Scholor - Naoom, S. F., Van Dyke, M., Fixsen, D. L., Blasé, K. A., & Villagomez, A. N. (2012). Developing implementation capacity of organizations and systems to support effective uses of family literacy programs. Handbook of family literacy, 447-464.
Publisher | Google Scholor - Haddad, L. B., & Nour, N. M. (2009). Unsafe abortion: unnecessary maternal mortality. Reviews in obstetrics and gynecology, 2(2):122.
Publisher | Google Scholor - Ganatra, B., Gerdts, C., Rossier, C., Johnson, B. R., Tunçalp, Ö., Assifi, A., ... & Alkema, L. (2017). Global, regional, and subregional classification of abortions by safety, 2010–14: estimates from a Bayesian hierarchical model. The Lancet, 390(10110):2372-2381
Publisher | Google Scholor - World Health Organization. (2011). Unsafe abortion: global and regional estimates of the incidence of unsafe abortion and associated mortality in 2008. World Health Organization.
Publisher | Google Scholor - Nour, N. M. (2008). An introduction to maternal mortality. Reviews in obstetrics and gynecology, 1(2):77.
Publisher | Google Scholor - Rahaman, M., Roy, A., Chouhan, P., Das, K. C., & Rana, M. J. (2023). Revisiting the predisposing, enabling, and need factors of unsafe abortion in India using the Heckman Probit model. Journal of Biosocial Science, 1-21.
Publisher | Google Scholor - Giorgio, M. M., Utomo, B., Soeharno, N., Aryanty, R. I., Besral, Stillman, M., ... & Sedgh, G. (2020). Estimating the incidence of induced abortion in Java, Indonesia, 2018. International Perspectives on Sexual and Reproductive Health, 46:211-222.
Publisher | Google Scholor - Farrar, R. (2020). Women's Rights are Human Rights: Finding the Right to Access an Abortion in International Law. NY Int'l L. Rev, 33:19.
Publisher | Google Scholor - Grimes, D. A., Benson, J., Singh, S., Romero, M., Ganatra, B., Okonofua, F. E., & Shah, I. H. (2006). Unsafe abortion: the preventable pandemic. The Lancet, 368(9550):1908-1919.
Publisher | Google Scholor - Soomar, S. M., & Ramzan, R. (2023). Pakistan's Safe Abortion Law: An Analytical Perspective based on Public Health Ethics. Pakistan Perspectives, 28(1).
Publisher | Google Scholor - Barot, S. (2018). The roadmap to safe abortion worldwide: lessons from new global trends on incidence, legality, and safety. NY Guttmacher Inst, 21:6.
Publisher | Google Scholor - Ganatra, B., Gerdts, C., Rossier, C., Johnson, B. R., Tunçalp, Ö., Assifi, A., ... & Alkema, L. (2017). Global, regional, and subregional classification of abortions by safety, 2010–14: estimates from a Bayesian hierarchical model. The Lancet, 390(10110):2372-2381.
Publisher | Google Scholor - Jewkes, R., Rees, H., Dickson, K., Brown, H., & Levin, J. (2005). The impact of age on the epidemiology of incomplete abortions in South Africa after legislative change. BJOG: An International Journal of Obstetrics & Gynaecology, 112(3):355-359.
Publisher | Google Scholor - Bateman, C. (2007). Maternal mortalities are 90% down as legal ToPs more than triple. South African Medical Journal, 97(12):1238.
Publisher | Google Scholor - Yokoe, R., Rowe, R., Choudhury, S. S., Rani, A., Zahir, F., & Nair, M. (2019). Unsafe abortion and abortion-related death among 1.8 million women in India. BMJ global health, 4(3):00149
Publisher | Google Scholor - Bell, S. O., Omoluabi, E., OlaOlorun, F., Shankar, M., & Moreau, C. (2020). Inequities in the incidence and safety of abortion in Nigeria. BMJ Global Health, 5(1):001814.
Publisher | Google Scholor - Ngowa, J. D. K., Neng, H. T., Domgue, J. F., Nsahlai, C. J., & Kasia, J. M. (2015). Voluntary induced abortion in Cameroon: prevalence, reasons, and complications. Open Journal of Obstetrics and Gynecology, 5(9):475.
Publisher | Google Scholor - Yogi, A., KC, P., & Neupane, S. (2018). Prevalence and factors associated with abortion and unsafe abortion in Nepal: a nationwide cross-sectional study. BMC pregnancy and childbirth, 18:1-10.
Publisher | Google Scholor - Fusco, C. L., Silva, R. D. S. E., & Andreoni, S. (2012). Unsafe abortion: social determinants and health inequities in a vulnerable population in São Paulo, Brazil. Cadernos de saude publica, 28(4):709-719.
Publisher | Google Scholor - Levandowski, B. A., Mhango, C., Kuchingale, E., Lunguzi, J., Katengeza, H., Gebreselassie, H., & Singh, S. (2013). The incidence of induced abortion in Malawi. International Perspectives on Sexual and Reproductive Health, 88-96.
Publisher | Google Scholor - Melese, T., Habte, D., Tsima, B. M., Mogobe, K. D., Chabaesele, K., Rankgoane, G., ... & Moreri-Ntshabele, B. (2017). High levels of post-abortion complication in a setting where abortion service is not legalized. PloS one, 12(1):0166287.
Publisher | Google Scholor - Akinlusi, F. M., Rabiu, K. A., Adewunmi, A. A., Imosemi, O. D., Ottun, T. A., & Badmus, S. A. (2018). Complicated unsafe abortion in a Nigerian teaching hospital: pattern of morbidity and mortality. Journal of Obstetrics and Gynaecology, 38(7):961-966.
Publisher | Google Scholor - Sousa, A., Lozano, R., & Gakidou, E. (2010). Exploring the determinants of unsafe abortion: improving the evidence base in Mexico. Health Policy and Planning, 25(4):300-310.
Publisher | Google Scholor - Fusco, C. L. B. (2013). Unsafe abortion: a serious public health issue in a poverty-stricken population. Reprodução & Climatério, 28(1):2-9.
Publisher | Google Scholor - Kulczycki, A. (2011). Abortion in Latin America: changes in practice, growing conflict, and recent policy developments. Studies in family planning, 42(3):199-220.
Publisher | Google Scholor - Akilimali, P., Moreau, C., Byrne, M., Kayembe, D., Larson, E., & Bell, S. O. (2023). Estimating induced abortion incidence and the use of non-recommended abortion methods and sources in two provinces of the Democratic Republic of the Congo (Kinshasa and Kongo Central) in 2021: results from population-based, cross-sectional surveys of reproductive-aged women. Sexual and Reproductive Health Matters, 31(1):2207279.
Publisher | Google Scholor - Bankole, A., Adewole, I. F., Hussain, R., Awolude, O., Singh, S., & Akinyemi, J. O. (2015). The incidence of abortion in Nigeria. International perspectives on sexual and reproductive health, 41(4):170.
Publisher | Google Scholor - Kalilani-Phiri, L., Gebreselassie, H., Levandowski, B. A., Kuchingale, E., Kachale, F., & Kangaude, G. (2015). The severity of abortion complications in Malawi. International Journal of Gynecology & Obstetrics, 128(2):160-164.
Publisher | Google Scholor - Emechebe, C. I., Njoku, C. O., Udofia, U. M., & Ukaga, J. T. (2016). Complications of induced abortion: Contribution to maternal mortality in a tertiary center of a low resource setting. Saudi Journal for Health Sciences, 5(1):34-38.
Publisher | Google Scholor - Kinaro, J., Mohamed Ali, T. E., Schlangen, R., & Mack, J. (2009). Unsafe abortion and abortion care in Khartoum, Sudan. Reproductive health matters, 17(34):71-77.
Publisher | Google Scholor