Case Report
Type IV Branchial Cyst in Pediatric Patient: Radio-Surgical Challenge
1Consultant E.N.T. and Head-neck surgeon, Apollo ENT Hospital, Rajasthan, India.
2 SS wellness centre, Jodhpur, Rajasthan, India.
*Corresponding Author: Pankaj Goyal, Consultant E.N.T. and Head-neck surgeon, Apollo ENT Hospital, Rajasthan, India.
Citation: Goyal P. Pooja M. (2024). Type IV Branchial Cyst in Paediatric Patient: Radio-Surgical Challenge. Journal of Surgical Case Reports and Reviews. BioRes Scientia Publishers. 3(1):1-5. DOI: 10.59657/2993-1126.brs.24.0021
Copyright: © 2024 Pankaj Goyal, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: March 02, 2024 | Accepted: March 22, 2024 | Published: March 30, 2024
Abstract
Background: Fourth branchial pouch abnormalities are uncommon congenital diseases of the neck caused by aberrant development of the branchial apparatus during embryogenesis. Misdiagnosis, inadequate treatment, and ongoing recurrence are possible outcomes of improper recognition of these aberrations.
Case Report: This article presents a unique case of a 12-year-old pediatric patient who reported with a sudden emergence of a left sided lateral neck mass following sports practice. The patient underwent thorough diagnostic testing, including radiographic tests, which revealed a fourth branchial cleft cyst and treated with surgical excision. The patient underwent surgical excision with no postoperative complications and remained asymptomatic during follow-up.
Conclusion: This case highlights the importance of considering brachial arch anomalies in the differential diagnosis of neck masses in pediatric patients.
Keywords: branchial pouch abnormalities; congenital; branchial cleft cyst; neck mass; radiographic test; surgical excision
Introduction
Six paired mesodermal arches make up the human branchial apparatus, which develops during the early stages of gestation. These arches are divided by ectodermal and endodermal invaginations known as clefts and pouches, respectively [1]. The mesenchymal core of each arch is made up of neural crest cells. This core will eventually give rise to the skeletal and interstitial structures of the head and neck, as well as the blood vessels and nerves that are connected to them. The branchial apparatus is hypothesized to be the source of congenital lateral cervical cysts, fistulae, and sinuses. Of the congenital malformations of the branchial apparatus, the second branchial arch, pouch, or cleft accounts for around 95% of cases, with the first and third arches accounting for the majority of the remaining cases [5]. Less than 100 occurrences have ever been documented in the literature [2,3]. making remnants of the fourth branchial arch incredibly uncommon. They make up 1-4 percent of all branchial abnormalities. The most common presentations of these abnormalities are acute suppurative thyroiditis, recurring neck infections, and/or abscesses [4,5]. The laryngeal cartilages, the pharyngeal and laryngeal constrictor muscles, the superior laryngeal nerve, the left thoracic aorta, the right proximal subclavian artery, the ultimobranchial body, which gives rise to the thyroid's calcitonin-secreting intrafollicular cells, and the superior parathyroid glands are all derivatives of the fourth pouch [6-8]. Nearly all fourth branchial abnormalities are seen on the left side [9,10,11]. There is no concrete evidence to support this private location's purpose. This discovery has been linked to the asymmetry in vascular development between the left and right fourth arches, according to certain suggestions [9,10]. The fourth arch artery on the left side develops into the aortic arch during normal branchial apparatus development, whereas the fourth arch artery on the right side forms the proximal portion of the right subclavian artery [12,13]. Nevertheless, an additional explanation might be the preferential left-sided development of the ultimobranchial bodies in most mammalian species, for reasons that are now unclear [14,15,16]. These malformations frequently pose difficulties for diagnosis and treatment. In certain cases, the diagnosis of fourth branchial abnormalities is still challenging despite the results of endoscopic assessment using direct laryngoscopy, computed tomography (CT) scan, barium swallow tests, and ultrasound. However, these congenital anomalies may not always be identifiable in clinical practice due to their uncommon frequency. This clinical example emphasizes how crucial it is to identify uncommon illnesses like branchial cleft cysts as soon as possible and to treat them appropriately.
Case Report
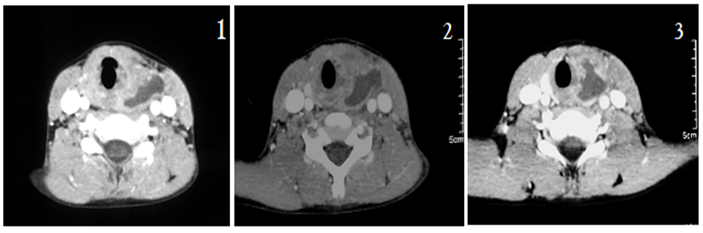
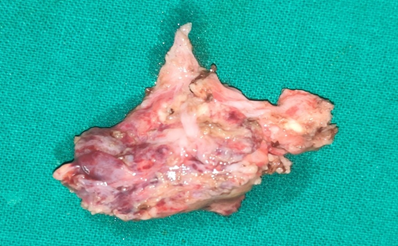
A twelve-year-old male youngster presented to Apollo E.N.T. Hospital in Jodhpur, Rajasthan, India, complaining of left-sided neck swelling on the anterior aspect during the previous three to four years. To begin, there was a history of anterior neck blunt traumatic injury while playing with a ball. He had an uncomfortable swelling on the left side of his neck at the time, as well as a fever. There had been no previous history of dysphagia, dyspnoea, hoarseness, vomiting, or aspiration. In response to the aforementioned concerns, the patient was prescribed medicine by a paediatrician. After 4-5 days of medicine, the swelling had shrunk and all of the symptoms had vanished. Within 3-5 months, he got swelling in the neck at the same spot, along with fever and discomfort. The computed tomography (CT) scan that was performed on this case demonstrated a hypodense mass lesion with rim enhancement between the left thyroid lobe and neck arteries, extending to the left pyriform sinus apex. These results are consistent with a thyroid abscess. Only leucocytosis was discovered in the blood tests. Intravenous antibiotics relieve the symptoms once more. After a year, the same problems have resurfaced. Parents were concerned about the symptoms this time. Parents sought advice from the paediatrician, but when the situation did not improve, the patient was transferred to us. Regarding the nature of the illness, parents have received counselling. A repeat CT scan was advised. Radiological diagnosis was challenging in this patient as the lesion was giving impression of thyroid abscess but looking at the previous radiology scan and history of recurrence, the possibility of recurrent infection in pre-existing congenital cyst was raised and laryngoscopy correlation was advised. The patient was scheduled for general anaesthesia surgery following the acquisition of appropriate consent for the surgical removal of the cyst. Direct laryngoscopy was used to rule out any communication with the pyriform fossa following intubation, and it was not present. An incision had been made in the lower neck skin crease following painting and draping at the surgical site. The subplatysmal flap was raised. Because of the cyst's fibrosis and inflammation, the strap muscles were attached to it. A good surgical plain was kept in place across the internal carotid artery and internal jugular vein. It was possible to identify the cyst's posterior wall and observe that a tiny pouch of the cyst was connected close to the side of the pyriform fossa. The cyst, with its whole posterior wall, was totally removed. Haemostasis was attained. The surgical site was sutured in layers, and the suction drain was left in place. After a successful extubation, the youngster was sent to recovery. The drain was removed on post-op day 2 and the patient was released without complaint. The patient is presently doing well.
Figure 1-3: Computed tomgraphy scan suggestive of hypodense mass lesion (arrow mark) with rim enhancement between the left thyroid lobe and neck arteries, extending to the left pyriform sinus apex (small vertical arrow).
Discussion
Branchial arches are the source of several particular structures seen in the neck. Acute suppurative thyroiditis, abscesses, or lateral neck masses are the typical symptoms of fourth branchial pouch abnormalities, which are unusual [4]. Just a few isolated occurrences have been documented since these anomalies were initially discovered in 1972; they represent 1-4 percent of all branchial apparatus abnormalities [17]. A fistula of branchial origin is made up of remains of both the pouch and the cleft, with rupture of the intervening branchial plate; a sinus is a tract that is accessible to either the gut or the skin, but not both, and a cyst is open to neither [18]. These three classifications can be used to describe anomalies. By means of the pharyngobranchial duct, the third and fourth pouches are joined to the throat. There is ongoing connection with the pyriform fossa if this duct does not disintegrate by the seventh week of pregnancy. It can be challenging to distinguish between abnormalities of the main arches based only on clinical criteria because to their comparable courses. Starting from the pyriform sinus, the fistulous tract of a fourth branchial pouch descends and exits the throat posterior to the thyroid cartilage, cricothyroid muscle, and superior laryngeal nerve. The trachea and recurrent laryngeal nerve are reached by the tract as it continues to descend lateral. The tract turns forward beneath the aortic arch on the left side before moving upward and posterior to the internal carotid artery. Rarely, the tract on the right side circumnavigates the subclavian artery before rising. The tract travels superiorly, passing across the hypoglossal nerve, and may eventually open externally in the neck at the sternocleidomastoid muscle's lower anterior part [6,7,19,20]. Age-related differences exist in the clinical appearance of anomalies of the fourth branchial arch. Dyspnoea episodes are the most common presentation in newborns [21], cervical cutaneous fistulas appear in childhood, and these cysts later present classically with a recurring history of infections and neck abscesses, the left side being affected in 93.6 percent of cases, the right side in 6%, and the bilateral location in 0.5% of cases. Acute suppurative thyroiditis can be caused by infectious episodes that manifest clinically as chronic neck edema and may even affect the ipsilateral thyroid lobe where the cyst is located. Subacute de Quervain's thyroiditis, Hashimoto's thyroiditis, or bleeding from a thyroid nodule should be considered as differential diagnoses when these signs are observed in the neck [22]. It is necessary to undertake a diagnosis in order to show the presence of a sinus or fistula originating in the pyriform sinus. These results can be shown with a barium esophagogram, which should only be performed once the acute infection has cleared up. The preferred methods for exhibiting thyroid involvement, as well as the location and extent of pyriform sinus abnormalities, are magnetic resonance imaging (MRI) and computed tomography (CT) [23, 24].
The timely detection of fourth branchial pouch abnormalities is a crucial problem that our case raises. The patient had received a great deal of medical care. Because of the risk of infection and potentially fatal abscesses, thorough surgical excision is the cornerstone of therapy for fourth branchial abnormalities [2, 5]. Recently, branchial cleft cysts have been treated with sclerotherapy using OK-432 [25]. Early excision is advised due to the increased likelihood of subsequent infection of congenital malformations. In order to start the surgical procedure in a region devoid of post inflammatory fibrosis, the thyroid ala and carotid sheath should be exposed [2].
Figure 4: Main surgical specimen
Conclusion
Unusual and intriguing prenatal development abnormalities, fourth branchial arch anomalies can manifest in a variety of ways. By appropriately evaluating the patient before to surgery and carefully organizing the surgical procedure, these lesions may be effectively removed, providing the patient with respite from this cause of recurring infection. Surgical removal of the abnormality is the final step towards definitive therapy.
Declarations
Compliance with Ethical Standards
The procedure performed in this case report was in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Funding
This study is not funded by any resources.
Conflict of Interest
The author (s) declares no potential conflicts of interest with respect to the research, authorship, and/or publication of this paper.
Ethical Approval
For the purpose of publishing this case report, the patient's written informed consent was obtained.
References
- M. Shrime, A. Kacker, J. Bent, et al. (2003). “Fourth branchial complex anomalies: a case series,”. International Journal of Pediatric Otorhinolaryngology, 67(11):12271233.
Publisher | Google Scholor - Jeyakumar and A. S. Hengerer. (2004). “Various presentations of fourth branchial pouch anomalies,” Ear, Nose and Throat Journal, 83(9): 640-644,
Publisher | Google Scholor - R. Nicollas, B. Guelfucci, S. Roman, et al. (2000). Congenital cysts, and fistulas of the neck,”. International Journal of Pediatric Otorhinolaryngology, 55(2):117-124,2000.
Publisher | Google Scholor - H. M. Tucker and M. L. Skolnick. (1973). “Fourth branchial cleft (pharyngeal pouch) remnant,”. Transactions of the American Academy of Ophthalmology and Otolaryngology, 77(5)3680-371.
Publisher | Google Scholor - S. Takai, A. Miyauchi, and F. Matsuzuka. (1979). “Internal fistula as a route of infection in acute suppurative thyroiditis,” The Lancet, 1(8119):751-752.
Publisher | Google Scholor - M. M. Cohen Jr. (2002). “Malformations of the craniofacial region: evolutionary, embryonic, genetic, and clinical perspectives,”. American Journal of Medical Genetics—Seminars in Medical Genetics, 115(4):245-268.
Publisher | Google Scholor - K. Nicoucar, R. Giger, T. Jaecklin, et al. (2010). “Management of congenital third branchial arch anomalies: a systematic review,” Otolaryngology—Head and Neck Surgery, 142(1):21-28.
Publisher | Google Scholor - K. Nicoucar, R. Giger, H. G. Pope, et al. (2009). “Management of congenital fourth branchial arch anomalies: a review and analysis of published cases,”. Journal of Pediatric Surgery, 44(7):1432-1439.
Publisher | Google Scholor - Meng F, Zhu Z, Ord RD, et al. A unique location of branchial cleft cyst: case report and review of the literature. Int. J. Oral Maxillofac. Surg, (2019). 48:712-715.
Publisher | Google Scholor - Andrieu-Guitrancourt J, Amstutz I, Buffet X. Bui P, Dehesdin D. (1988). Recurrent lateral cervical suppuration Role of fistulae and cysts of fourth branchial pouch. Ann Oto-Laryngol (Paris), 105:189-92.
Publisher | Google Scholor - Rosenfeld RM, Biller HF. Fourth branchial pouch sinus: diagnosis and treatment. Otolaryngol Head Neck Surg. (1991) 105:44-50.
Publisher | Google Scholor - Rea, Hartley. (2004). Bailey: third and fourth branchial pouch anomalies. J Laryngol Otol. 118:19-24.
Publisher | Google Scholor - Wang HK, Tiu CM, Chou YH, Chang CY. (2003). Imaging studies of pyriform sinus fistula. Pediatr Radiol, 33:328-333.
Publisher | Google Scholor - Chaudhary N, Gupta A, Motwani G, Kumar S. (2003). Fistula of the fourth branchial pouch. Am J Otolaryngol. (2003). 24:250-252.
Publisher | Google Scholor - Saxén L, Toivonen S. (1955). The development of the ultimobranchial body in Xenopus laevis Daudin and its relation to the thyroid gland and epithelial bodies. Development. 3:3760-3784.
Publisher | Google Scholor - Manac’h Y. Morisseau MP, Penin A, Aboucaya JP. (1988). Le fond du sinus piriform dans le traitement chirurgical des fistules de la quatrième poche endobranchiale. Otolaryngol (Paris). 105:391-396.
Publisher | Google Scholor - M. Shrime, A. Kacker, J. Bent, and R. F. Ward. (2003). “Fourth branchial complex anomalies: a case series,” International Journal of Pediatric Otorhinolaryngology, (67):111227-1233.
Publisher | Google Scholor - M. S. Godin, D. B. Kearns, S. M. Pransky, et al. (1990). “Fourth branchial pouch sinus: principles of diagnosis and management,” Laryngoscope, (2):174–178, 1990.
Publisher | Google Scholor - B. A. Mantle, T. D. Otteson, and D. H. Chi. (2008). “Fourth branchial cleft sinus: relationship to superior and recurrent laryngeal nerves,” American Journal of Otolaryngology, 29(3)198-200,
Publisher | Google Scholor - K.D. Pereira, G. G. Losh,D.Oliver, et al. (2004). “Management of anomalies of the third and fourth branchial pouches,” International Journal of Pediatric Otorhinolaryngology, 68(1):43-50,
Publisher | Google Scholor - Kruijff S, Sywak MS, Sidhu SB et al. (2015). Thyroidal abscesses in third and fourth branchial anomalies: not only a paediatric diagnosis. ANZ J Surg, 85:578-5781.
Publisher | Google Scholor - Hallak B, Bouayed S, Leishman C et al. (2014). Residual fistula of fourth branchial arch anomalies and recurrent left-side cervical abscess: clinical case and review of the literature. Case Rep Otolaryngol.
Publisher | Google Scholor - N. Chaudhary, A. Gupta, G. Motwani, and S. Kumar. (2003). “Fistula of the fourth branchial pouch,” American Journal of Otolaryngology, 24(4):250-252,
Publisher | Google Scholor - T. Z. Hwang, Y. J. Lin, and S. T. Tsai. (2000). “Fourth branchial cyst presenting with neonatal respiratory distress,” Annals of Otology, Rhinology and Laryngology, 109(4):431-434.
Publisher | Google Scholor - Kim, Myung-Gu et al. (2009). “Sclerotherapy of branchial cleft cysts using OK 432.” Otolaryngology--head and neck surgery: official journal of American Academy of Otolaryngology-Head and Neck Surgery vol. 141(3):329-334.
Publisher | Google Scholor