Case Report
Transient Intussusception of Terminal Ileum Due to Intestinal Endometriosis: A Case Report
- Erika Ermida Freitas 1*
- Djulia Adriani Frainer 2
- Carolina Da Silveira Welter 1
- Dayana Talita Galdino 3
1General Surgery Residency, Sao Jose Municipal Hospital, Joinville, Santa Catarina, Brazil.
2Medicine Course, University of the Joinville Region, Joinville, Santa Catarina, Brazil.
3Trauma Surgery, Sao Jose Municipal Hospital, Joinville, Santa Catarina, Brazil.
*Corresponding Author: Erika Ermida Freitas, General Surgery Residency, Sao Jose Municipal Hospital, Joinville, Santa Catarina, Brazil.
Citation: Erika E. Freitas, Djulia A. Frainer, C.D.S. Welter, Dayana T. Galdino. (2024). Transient Intussusception of Terminal Ileum Due to Intestinal Endometriosis: A Case Report, International Journal of Biomedical and Clinical Research, BioRes Scientia Publishers. 1(2):1-4. DOI: 10.59657/2997-6103.brs.24.007
Copyright: © 2024 Erika Ermida Freitas, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: April 09, 2024 | Accepted: June 19, 2024 | Published: June 26, 2024
Abstract
Intestinal obstruction in adults is usually secondary to neoplasms, hernias and adhesions. Intestinal intussusception is a rare cause in this population, especially when associated with etiologies such as intestinal endometriosis. This report presents the case of a 32-year-old patient with an obstructive acute abdomen due to intussusception in the terminal ileum, secondary an intestinal endometriosis, requiring a surgical approach through enterectomy of the affected segment.
Keywords: intussusception; endometriosis; abdomen; acute; ileum; case reports
Introduction
Obstructive acute abdomen is one of the main causes of acute abdomen in the adult population. The causes are usually tumors, hernias and adhesions [1]. Intestinal intussusception is a rare condition in this age group, associated with less than 5% of cases. When present, it is usually secondary to tumors, with few cases described in the literature resulting from endometriosis intestinal [2]. In this report, the case of a 32-year-old patient who presented with an acute abdomen obstructive due to intestinal intussusception in terminal ileum, secondary to intestinal endometriosis, requiring enterectomy and enteroanastomosis of the affected segment, and with good evolution after operative. This article was registered under the CAAE 51683821.3.0000.5362 and approved by the committee of ethics of the proposing institution for the process 4,972,878. Free consent form obtained and clarified in the use of information from the medical record doctor and images by the patient.
Case Report
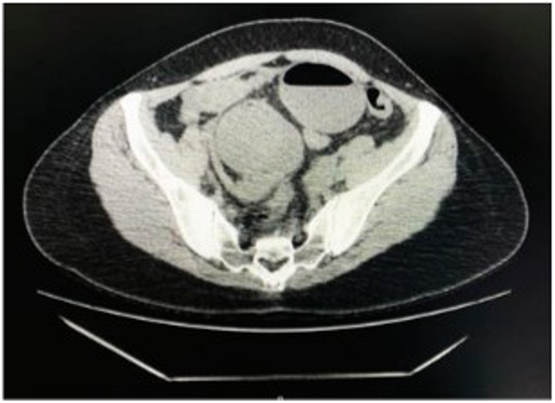
Female patient, 32 years old, nulliparous, no comorbidities, use of continuous medications or previous surgeries and no gynecological complaints. She presented with periumbilical abdominal pain of sudden onset, in colic, with three days of evolution, associated with nausea and diarrhea. On physical examination, diffuse abdominal pain on palpation, without signs of peritoneal irritation. Laboratory tests without changes. In the tomography performed on admission, there were signs suggestive of ileal intussusception distal in hypogastrium. (Figure 1) Choosing to maintain observation due to the absence of alarm signals and improvement of symptoms with simple analgesia.
Figure 1: Computed tomography showing the presence of intussusception in the distal ileum.
After 72 hours of hospitalization, her condition worsened. The abdominal pain became refractory to analgesia, with absence of evacuations during the period, maintaining vital signs stable and laboratory tests were unremarkable. Due the evolution of the condition, opting for a new tomography, which showed maintenance of the intussusception susceptibility associated with the presence of small amounts of free liquid in the cavity, indicating surgical treatment.
Figure 2: Small loop obstruction secondary to adhesion process firm in the serosa of the small intestine.
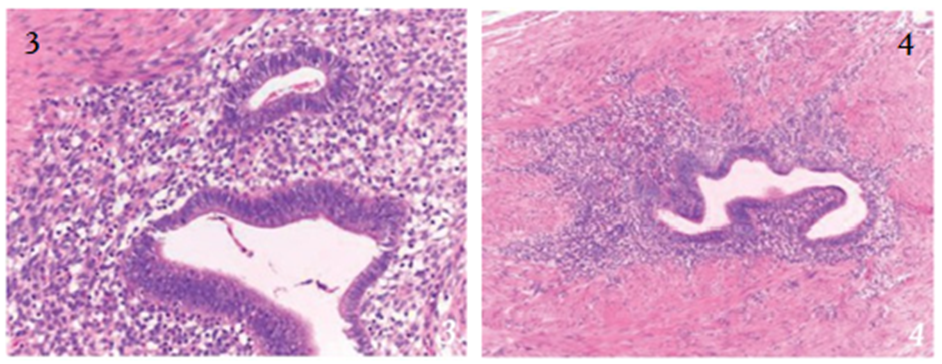
At laparotomy, evidence of significant distension of proximal loops of the secondary small area of obstruction in the region of the distal ileum (between 15 and 20cm from the ileocecal valve), due to an adequate process firm structure located in the serosa of the intestinal loop. No signs of intussusception or lung ischemia intraoperatively. (Figure 2) Associated, there was moderate amount of serohematic fluid in pelvic region. Opted for segmental enterectomy affected and laterolateral enteroanastomosis at 15 cm of the ileocecal valve with a stapler due to important difference in diameter between the proximal and distal loop. Lymph node biopsies were performed due to associated with mesenteric lymph node enlargement. Patient developed an episode of paralytic ileus post-surgery, with improvement after clinical measures, being discharged on the 5th post-operative day and with good evolution during outpatient follow-up. Pathology (Figure 3 and 4) of the surgical specimen showed endometriosis of the terminal ileum, with no presence of neoplasia in the sample. Later patient referred for gynecological follow-up.
Figures 3, 4: Histological sections of small intestine samples, stained using the hematoxylin and eosin technique, reveal stromal islands with an endometrium surrounding glands lined by simple cylindrical epithelium.
Discussion
Intussusception occurs due to the invagination of a proximal segment through the distal in a portion of the intestine. Normally this telescoping occurs due to the presence of a lesion in the intestinal lumen that interferes with peristalsis. About 95% of intussusception occurs in children, being a common cause of intestinal obstruction in this population, usually secondary to viral infections or idiopathic². In adults, its incidence is very minor, and has etiologies different from pediatric ones, being related to pathological conditions in 90%, 65% of which are malignant tumors. Transient intussusception, the main diagnostic suspicion in this patient, is even rarer and related to celiac disease, Crohn's disease or bridles, none of which were present in the case described [3,4]. Endometriosis is a gynecological condition, of unknown etiology and poorly established pathophysiology, with a chronic and benign evolution, which can be defined as the presence of endometrial tissue outside the uterine cavity, affecting approximately 5-10% of women of childbearing age [2]. The gastrointestinal tract is the most common extra pelvic location, occurring in approximately 3 to 37% of women with endometriosis, being the rectum and sigmoid colon, the most common sites. Involvement of the small intestine is infrequent, corresponding to only 0.5% of cases [3]. The main symptoms of endometriosis are infertility, dysmenorrhea and dyspareunia, however, vary depending on your location. When it affects the small intestine, it is most often asymptomatic due to the fact that the implants remain in the serous layer, which may or may not be associated with a local inflammatory process and generate non-specific symptoms such as cramps and postprandial distension [2,5]. In the case in question, the patient did not report symptoms of endometriosis or previous gastrointestinal changes, however, their age range is compatible with your diagnosis, since extra pelvic endometriosis generally manifests between 30 and 40 years of age [5].
According to the pathophysiology of intestinal endometriosis, the endometrial implant in the ileal wall generates a localized fibrosis, whose inflammatory process may develop and present as a stenosing, polypoid mass, or both. In this case, the fibrotic lesion observed intraoperatively, later attributed to endometriosis, possibly acted as a lesion that caused the transient intestinal intussusception present in this case. The initial approach to intestinal intussusception, in the absence of alarm signals, it is conservative through hydrostatic or pneumatic reduction, with high success rate. The patient must undergo clinical observation due to the possibility recurrence in the first 24 hours. Contraindications for conservative treatment are peritonitis, hemodynamic instability and persistence of intussusception which is associated with the greatest risk necrosis of the affected intestinal segment. At presence of any contraindication, a surgical approach through laparotomy is indicated exploratory or video laparoscopy [6]. In the aforementioned case, conservative treatment was chosen through hospitalization and clinical observation due to improvement of abdominal pain with simple analgesia and for not presenting changes on physical examination and laboratory. However, on the 3rd day of hospitalization hospital, evolved with a significant worsening of abdominal pain, with absent intestinal elimination, in addition repeat imaging examination confirming persistence of intestinal intussusception and free fluid in the abdominal cavity, surgical treatment through laparotomy being indicated [7-15]. Furthermore, despite the exploratory laparotomy is not considered standard gold for diagnosing endometriosis, were not evidenced endometrial implants in review of cavity, making it difficult to formulate this hypothesis intraoperative diagnosis, mainly related to the fact that there is no suspicion of this condition beforehand.
Conclusion
Like intussusception, intestinal endometriosis is a rare cause of intestinal obstruction. However, despite being uncommon, this diagnosis should be considered in young patients, especially those of childbearing age. Therefore, the case referred to contributes to assisting in the diagnostic spectrum differences in cases of obstructive acute abdomen.
References
- Kumar KJ, Chandrashekar A, Basavaraja CK, Kumar HCK. (2016). Acute Pancreatitis Complicating Dengue Hemorrhagic Fever. Rev Soc Bras Med Trop. 49(5):656-659.
Publisher | Google Scholor - Jain V, Gupta OP, Rao T, Rao S. (2014). Acute Pancreatitis Complicating Severe Dengue. J Glob Infect Dis. 6(2):76-78.
Publisher | Google Scholor - Simadibrata M. (2012). Acute Pancreatitis in Dengue Hemorrhagic Fever. Acta Med Indones. 44(1):57-61.
Publisher | Google Scholor - Correa R, Ortega-Loubon C, Zapata L, Armién B, Culquichicón C. (2019). Dengue With Hemorrhagic Manifestations and Acute Pancreatitis: Case Report and Review. Cureus. 11(6):1-5.
Publisher | Google Scholor - Krithika AP, Ramya R. (2018). Acute Pancreatitis: A Late Complication of Dengue Fever. Int J Contemp Pediatr. 5(2):676.
Publisher | Google Scholor - Mishra A, Saini R, Kallani M. (2019). Acute Pancreatitis Associated with Dengue Fever: An Interesting and Rare Complication of Dengue Virus. Indian J Case Reports. 5(1):29-32.
Publisher | Google Scholor - Seetharam P, Rodrigues G. (2010). Dengue Fever Presenting as Acute Pancreatitis. Eurasian J Med. 42(3):151-152.
Publisher | Google Scholor - Wijekoon CN, Wijekoon PWMCSB. (2010). Dengue Hemorrhagic Fever Presenting with Acute Pancreatitis. Southeast Asian J Trop Med Public Health. 41(4):864-866.
Publisher | Google Scholor - Sudulagunta SR, Sodalagunta MB, Sepehrar M, Raja SKB, Nataraju AS, et al. (2016). Dengue Shock Syndrome. Oxford Med Case Reports. 2016(11):269-272.
Publisher | Google Scholor - Banday IA, Gattoo I, Khan AM, Javeed J, Gupta G, et al. (2015). Modified Computed Tomography Severity Index for Evaluation of Acute Pancreatitis and Its Correlation with Clinical Outcome: A Tertiary Care Hospital Based Observational Study. J Clin Diagn Res. 9(8):TC01-TC5.
Publisher | Google Scholor - Rasslan R, Novo FCF, Bitran A, Utiyama EM, Rasslan S. (2017). Management of Infected Pancreatic Necrosis: State of The Art. Rev Col Bras Cir. 44(5).
Publisher | Google Scholor - Portelli M, Jones CD. (2017). Severe Acute Pancreatitis: Pathogenesis, Diagnosis and Surgical Management. Hepatobiliary Pancreat Dis Int. 16(2):155-159.
Publisher | Google Scholor - Trujillo KAR, Altamirano FDE, Cristellot CJD, Ortega BES. (2021). Necrosectomia Pancreática. Recimundo. 5(2):149-158.
Publisher | Google Scholor - El Boukili I, Boschetti G, Belckhodja H, Kepenekian V, Rousset P, et al. (2017). Role Of Surgery in Acute Necrotizing Pancreatitis. J Visc Surg. 154(6):413-420.
Publisher | Google Scholor - Ye J, Wang L, Lu S, Yang D, Hu W, et al. (2021). Clinical Study on Cystogastrostomy and Roux-En-Y-Type Cystojejunostomy in The Treatment of Pancreatic Pseudocyst. Medicine. 100(10):e25029.
Publisher | Google Scholor