Case Report
Tracheostomal Myiasis: A Case Report
1Department of Emergency Medicine Sisli Hamidiye Etfal Training and Research Hospital, University of Health Sciences Turkey, Istanbul, Turkey.
2Department of Otolaryngology, Sisli Hamidiye Etfal Training and Research Hospital, University of Health Sciences Turkey,İstanbul, Turkey.
3Department of Emergency Medicine Bağcılar Training and Research Hospital, University of Health Sciences Turkey, Istanbul, Turkey.
*Corresponding Author: Abuzer Coskun, Department of Emergency Medicine Bağcılar Training and Research Hospital, University of Health Sciences Turkey, Istanbul, Turkey.
Citation: Mehmet N. Sutasir, Memioglu M, Ece M, Altınbilek E, Coskun A. (2024). Tracheostomal Myiasis: A Case Report. Journal of BioMed Research and Reports, BioRes Scientia Publishers. 4(3):1-4. DOI: 10.59657/2837-4681.brs.24.064
Copyright: © 2024 Abuzer Coskun, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: December 28, 2023 | Accepted: January 20, 2024 | Published: January 26, 2024
Abstract
Myiasis is an infection caused by the larvae of Diptera flies in the human body. Larvae can infect skin, necrotic tissues and natural cavities of living humans. Myiasis may be primary if it infects intact skin, or secondary if it infects the site of a previous injury. Human myiasis is rare in Europe and North America. It is common in tropical and subtropical regions and in hot and humid climates. Compromise of tissues due to malignant disease, surgery, ischemia, or infection may predispose the patient to myiasis. In this case, we aimed to present a 90-year-old male patient who came to our emergency department with the diagnosis of Myiasis, along with the literature.
Keywords: tracheostomal myiasis; infection; larvae of diptera flies; human body
Introduction
The term myiasis was first used by Frederick William Hope in 1840. “Myia” means fly in Greek, and myiasis is the name given to the disease caused by some fly larvae feeding on the tissues of humans and animals [1]. Myiasis is common throughout the world. It is generally common in regions where sheep and goats are raised in the summer months. Myiasis is divided into two parts: internal and traumatic cutaneous myiasis. Generally, traumatic skin myiasis agents belong to the Calliphoridae and Sarcophagidae families, while Oestrus, Gasterophilus, and Hypoderma are internal myiasis agents. Myiasis larvae can be transmitted to humans while feeding on wounds in animals [2]. In addition to their harmful effects, today larvae of these flies are used in wound treatment and forensic medicine [3]. It is prevalent all over the world, especially in tropical and subtropical countries with low socioeconomic status. Myiasis in humans has been associated with low socioeconomic status, mental or neurological diseases, poor personal hygiene, diabetes mellitus, malnutrition, advanced-stage cancer, and immunosuppression. Myiasis is most commonly seen as skin invasion in the human body but can be observed in many areas such as the eye, ear, nose, throat, urogenital, intestinal, cerebral, and tracheopulmonary. Tracheopulmonary myiasis is a very rare condition [4].
Case Presentation
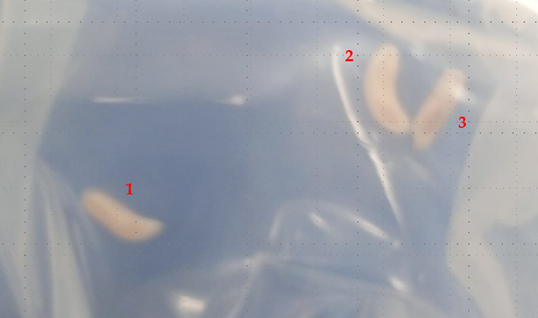
A 90-year-old male patient attended our emergency department for swelling and erythema around the tracheostomy cannula. He had an acute stroke two years ago. After this incident, he underwent percutaneous tracheostomy by anaesthesiologists at different healthcare centers. He had undergone a cardiac stent two years previously. He applied to our hospital emergency department with confusion and complaints of fatigue. He had a history of ischemic stroke two years ago. Additionally, he had hypertension and a cardiac stent. He was immobile, debilitated, and bedridden for two years. After this incident, he underwent percutaneous tracheostomy by anaesthesiologists at different healthcare centers. He had bad hygienic conditions with poor personal care. His tracheostomy cannula was changed only one time in the past two years. On physical examination maggots were seen around the tracheostomy cannula Three live larvae were carefully removed from the tracheostomy wound in the emergency department (Figure 1). Larvae were 10 mm long and 3 mm wide. However, we cannot remove the other larvae around the tracheostomy cannula. During the examination of the patient, we observed many larvae between the tube and the tracheal wall. After Otolaryngology consultation the patient was hospitalized for tracheostomy care. The peritracheostomal area was inflamed and had a bad odor and larvae were seen. A flexible bronchoscopy was performed to rule out the presence of larvae in the lower respiratory tract, and no larvae or debris were found. Wound debridement and tracheostomy cannula replacement were performed in an operation room. Special care was taken to avoid larvae falling to the lungs. With regular dressing of the tracheostomy stoma, the wound healed in one week. The patient was discharged postoperative second day.
Figure 1: Three larvae removed in Emergency Department
Discussion
Myiasis is a Diptera larval infection that is not commonly seen, especially in Western societies, and it affects human tissues and vertebrate animals. Myiasis is a disease caused by the invasion of organs and tissue by dipterous larvae, which last for some time and feed on the living or dead tissues. The larvae become mature and invasive and leave the necrotic tissue for viable tissue, causing extension of the lesion by local tissue destruction. Myiasis is also found among elderly and abandoned individuals, as well as in interns of geriatric hospitals and mental institutions presenting poor hygiene habits [5]. Risk factors for this infection include low socioeconomic status, immunosuppression, advanced age, alcoholism, neurological disease, and vegetative state. Our patient, being of advanced age, having a neurological disease, and having a low socioeconomic status, provided a suitable environment for myiasis to develop. Since this infection is not common, especially in Western societies, it is important for emergency physicians and otolaryngologists, who are likely to encounter this infection at the primary care level, to be aware of this disease. Myiasis occurs by dipterous larvae developing in decaying tissues and the developmental transition via the larval stage requires an intermediate host and the number of developing larvae depends on the number of viable eggs deposited. The Three live larvae that were difficult to remove in the emergency department and some maggots in this report determined extensive tissue damage, have been necessary operative. The myiasis is diagnosed clinically based on the presence of the maggots but the classification of the larvae rarely has been made. In the present case was not possible to identify the larvae. Myiasis can be primary if it infects intact skin or secondary if it infects a previous injury. Depending on the degree of parasitism, myiasis may be obligatory, facultative, or accidental [6]. People living in underdeveloped countries where malnutrition and unsanitary conditions are more prone are vulnerable to diseases such as myiasis [7].
Progressive necrosis of the tissue continues, along with the deep invasion of the larvae until a cavernous lesion is formed, while the larvae aggregate and remain active. The lesion is characterized by tense and oedematous surrounding tissue with a pungent odor. Extension of the lesion into the body cavity would be seen in some of the cases. The larvae can damage the vital tissues which sometimes be fatal if they cause life-threatening hemorrhage [8]. The severity of the lesion depends on the time interval from the onset of infection and the diagnosis of the lesion. If the lesion is diagnosed early, a smaller number of larvae will be present with minimal tissue damage. However, if the lesion is presented at a later stage or delayed, it will result in a greater number of larvae with extensive tissue necrosis. Therefore, early diagnosis is crucial to limit tissue damage. Depending on the number of viable eggs that are deposited by the female fly, the same number of larvae hatches and grow in any lesion. Myiasis can be prevented by practicing good personal hygiene, primary care of wounds, controlling fly population, and maintenance of sanitation of the surroundings. Apart from these, the patient’s relatives should be educated about post-operative care, by teaching them the dressing and wound care and the importance of it, so that such manifestation of larvae could be prevented. Any symptoms relating to infestation should be reported to the hospital as soon the earliest so that the lesion can be treated with minimal tissue damage rather than extensive necrosis when presenting at a later stage [9].
In tracheostomy myiasis, because of the risk of lower airway obstruction and aspiration pneumonia, migration of maggots to the tracheobronchial tree should be prevented during treatment [9]. Regular tracheostomy dressing and good hygienic conditions are crucial for preventing tracheostomy myiasis [10]. There are no standard treatment guidelines for myiasis. Treatment includes larval removal, antisepsis, regular dressing, and general care interventions. Antibiotics and larval removal are effective for treating secondary infection [11].
Conclusion
For bedridden patients, patients with superficial wounds who live in myiasis-endemic areas, or patients who undergo a tracheostomy or have open wounds, health workers and caregivers should consider preventive care of wounds, which are risk factors for myiasis infection. This care consists of suitable wound dressing and proper personal and environmental hygiene. Myiasis can be prevented, so “prevention is better than cure”.
Declarations
Author Contributions
Conception/Design of study- M.N.C, M.M, M,E; Data acquisition- E.A, A.C.; Data analysis/Interpretation- M.N.C, M.M.; Drafting manuscript- E.A, A.C.; Critical revision of manuscript- A.C.; Final approval and accountability- E.A; Technical or material support – M.N.C, M,E; Supervision – M.N.C, M.M, M,E, A.C.
Informed Consent
Written informed consent was obtained from the patient. Ethics Committee Approval: Ethics committee approval was not required for the case report.
Conflict of Interest
Authors declared no conflict of interest
Financial Disclosure
Authors declared no financial support.
Funding
None declared.
Availability of Data and Materials
All data is available on request without restriction.
Conflict of Interest
None declared.
Human Rights
The study was made in following the Declaration of Helsinki for Human Research.
References
- Sayin Ipek DN, Saki EC, Ozer E. (2011). External Myiasis Factors and Seasonal Distribution in Diyarbakır and Its Surroundings. Kafkas University Faculty of Veterinary Medicine Journal, 17(3):469-475.
Publisher | Google Scholor - Yaman M, Zerek A. (2017). Use of Myiasis Flies Larvae in the Wound Treatment. Mustafa Kemal Univ Medical Journal. 8(32):20-28.
Publisher | Google Scholor - Sherman RA, Hall MJ, Thomas S. (2000). Medicinal maggots: an ancient remedy for some contemporary afflictions. Annu Rev Entomol, 45:55-81.
Publisher | Google Scholor - R. Balasubramanya, N. Pushker, M. S. Bajaj, and A. Rani. (2003). Massive orbital and ocular invasion in ophthalmomyiasis. Canadian Journal of Ophthalmology, 28:297-298.
Publisher | Google Scholor - Francesconi F, Lupi O. (2012). Myiasis. Clin Microbiol Rev. 25:79-105.
Publisher | Google Scholor - Abdo EN, Sette-Dias AC, Comunian CR, Dutra CEA, Aguiar EG. (2006). Oral myiasis: A case report. Med Oral Patol Oral Cir Bucal. 11:E130-E131.
Publisher | Google Scholor - Auluck A. (2005). Oralhealth of poor people in rural areas of developing countries. J Can Dent Assoc Nov, 71:753-755
Publisher | Google Scholor - RibeiroFAQ, Pereira CSB, Alves A, Marcon MA. (2001). Treatment of human myiasis with ivermectin oral cavity. Rev Bras Otorrinolaringol, 67:755-761
Publisher | Google Scholor - Shinohara EH, Marini MZ, Oliveira Neto HG, Takahashi A. (2004). Oral myiasis treated with ivermectin: case report. Braz Dent J, 15:79-81
Publisher | Google Scholor - Blejter J. (2012). Tracheostomy wound myiasis in a child: case report and review of the literature. Case Rep Pediatr, 317862.
Publisher | Google Scholor - Prasanna Kumar S, Ravikumar A, Somu L, Vijaya Prabhu P. (2011). Mundakannan Subbaiya Periyasamy Subbaraj R. Tracheostomal myiasis: a case report and review of the literature. Case Rep Otolaryngol., 2011:303510.
Publisher | Google Scholor