Case Report
Thymic Cancer: A Not-So-Indolent Cause of Pericardial Effusion
- L. Afendi *
- F. Essadqi
- M. Belhakim
- A. El bouaazizi
- M. Haboub
- L. Azouzi
- R. Habbal
Cardiology, UHC Ibn Rochd, Casablanca, Morocco.
*Corresponding Author: L. Afendi, Cardiology, UHC Ibn Rochd, Casablanca, Morocco.
Citation: Afendi L, Essadqi F, Belhakim M, El bouaazizi A, Haboub M. et al. (2024). Thymic Cancer: A Not-So-Indolent Cause of Pericardial Effusion. Clinical Case Reports and Studies, BioRes Scientia Publishers. 6(2):1-4. DOI: 10.59657/2837-2565.brs.24.139
Copyright: © 2024 L. Afendi, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: June 05, 2024 | Accepted: June 19, 2024 | Published: June 27, 2024
Abstract
Tumors of the thymus are rare, and represent about 20% of all mediastinal tumors, the most frequent are thymomas, A pericardial effusion is an infrequent mode of discovery of these tumors present in about 20% of patients. In this report we describe the case of a 52-year-old patient who was admitted to the cardiology department for a very abundant pericardial effusion complicated by cardiac tamponade associated with an intra-OD mass revealing a locally advanced thymoma with invasion of the pericardium of OD and large vessels.
Keywords: mediastinal mass; thymoma; pericardial effusion; cardiac tamponade; mass intra-OD
Introduction
Thymomas are the most common neoplasia of the thymus, and the most common primary tumor. current of the anterior mediastinum in adults. They are usually benign or malignant in nature low-grade thymic epithelium [1]. The average age at diagnosis is around 50 years [2], earlier in those with myasthenia gravis, and they are extremely rare before age 15 and rare before age 20. The clinical presentation of a thymoma varies from asymptomatic incidental discovery to manifestations such as cough, paraneoplastic syndrome and symptoms caused by thoracic spread of the tumor such as phrenic nerve palsy. Pleural and pericardial effusions may occur in disseminated cases; however, spontaneous hemorrhagic pericardial effusion complicated by cardiac tamponade is a very rare finding. In this work we report the case of a patient in whom the etiological investigation of a very abundant pericardial effusion revealed the diagnosis of a thymoma with invasion of the pericardium and the right atrium as well as the great vessels.
Presentation of the case
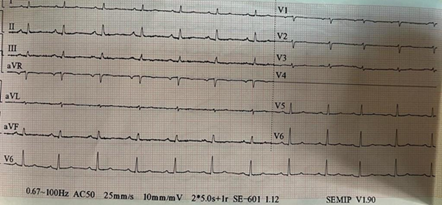
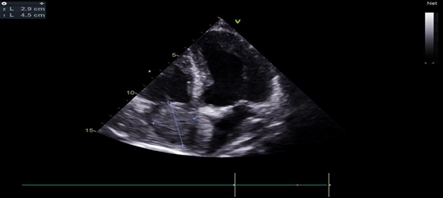
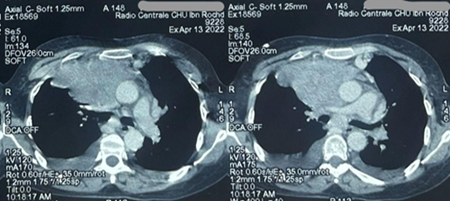
This is a 52-year-old patient without any particular pathological ATCDS, who presented to the emergency room for asthenia with chronic dyspnea that had recently worsened without any other associated signs. The clinical examination in her case had objectified a dyspneic patient with NYHA stage III with hypotension at 09/05, tachycardia at 110 bpm and turgidity of the jugular vein associated with collateral circulation in the abdomen. On the ECG, a diffuse micro voltage with electric alternation of the QRS was noted (figure 1), the biological assessment carried out in emergency was without particularities and the chest X-ray had shown cardiomegaly with blunting of the right CDS, a Trans thoracic echocardiography (ETT) was carried out evoking a very abundant effusion with collapse of the OD and variations in flow at the level of the tricuspid at 57% associated with a hyperechoic mobile rounded intra OD mass measuring 20*20mm (figure 2), in front of the hemodynamic instability of the patient the effusion was punctured urgently with removal of 900cc of sero-haematic fluid with good clinical evolution, a CTAP CT scan was subsequently performed showing a locally advanced mediastinum-pulmonary process of LSD having close links with the pericardium and the large vessels associated with a large bilateral and pericardial pleural effusion and an intra OD mass of tissue appearance in contact with the mediastinal mass related either to an invasion by contiguity or a 2nd mass (figure 3).
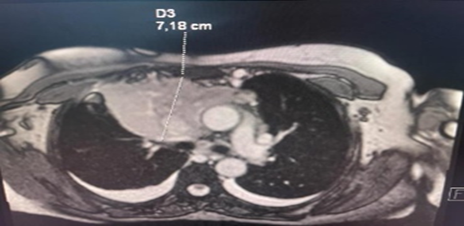
A biopsy of the mass under ultrasound guidance was performed with an anatomopathological study evoking a thymoma with a morphological and immunohistochemical aspect in favor of a type B1 thymoma. Cardiac MRI was performed confirming tumor invasion of the OD (Figure 4). In view of the locally advanced extension and the non-respectability of the tumour, it was decided to initiate neoadjuvant induction chemotherapy. A weekly ultrasound control of the pericardial effusion was done in the patient.
Figure 1: Electrocardiogram (ECG) showing diffuse microvoltage with electrical alternation.
Figure 2: Transthoracic echocardiography (TTE) showing intra OD mass
Figure 3: Computed tomography of the thorax showing a locally advanced mediastinum-pulmonary mass.
Figure 4: Cardiac MRI: performed confirming tumor invasion of the OD.
Discussion
Thymomas are rare epithelial tumors in adults (overall incidence of 0.15 per 100,000 person- years of malignant tumors [3]). The rarity and diversity of the clinical presentation makes the positive diagnosis of thymomas difficult.
One-third to one-half of patients with thymoma are asymptomatic, and 33% of patients have local symptoms related to involvement of surrounding structures such as chest pain, chest discomfort, dyspnea, and superior vena cava syndrome [4]. The effusion is an infrequent clinical manifestation, present in 20% of patients [5], what we report in our patient is a hemorrhagic pericardial effusion of great abundance revealing a locally advanced thymoma with invasion of the pericardium and the atrium right and large vessels. According to the literature it has never been described.
Malignant tumors of the thymus can be staged according to the Masaoka staging system [6] which is based on the integrity of the thymic capsule, the occurrence of macroscopic or microscopic invasion into neighboring structures and metastatic spread; there are 4 stages (according to the Masaoka system) with a poor prognosis for advanced stages and a higher recurrence rate [7]. The Thymoma in our case was classified as stage III with macroscopic involvement of the pericardium and OD and large vessels while the mode of discovery was pericardial effusion complicated by tamponade and associated with an intra OD mass. As far as thymic tumors are concerned, surgery remains the treatment of choice for operable thymic tumors [8]. Platinum-based chemotherapy such as cisplatin remains the standard of care for thymic malignancies that are locally advanced as well as metastatic disease. Histone deacetylase inhibitors have shown some response in thymoma; Sunitinib, an inhibitor of the tyrosine kinase receptor, can be active in thymic carcinoma [9], as was the case in our patient before the locally advanced extension chemotherapy was initiated based on cyclophosphamide, doxorubicin and cisplatin.
On the other hand, the best approach in the diagnosis and treatment of neoplastic pericardial disease has not yet been defined. The authors report the most recent literature on the new techniques useful for the diagnostic process but the literature on the therapeutic options is critically reviewed, in order to give suggestions for use in clinical practice. Pericardial effusion may require urgent drainage; however, the solid component becomes predominant in some cases [10].
Conclusion
Thymomas can present atypically, such as with a hemorrhagic pericardial effusion, complicating their diagnosis and treatment. The described case demonstrates the importance of a multidisciplinary approach for locally advanced thymomas. Platinum-based chemotherapy remains essential for unresectable tumors. This report enriches the literature by documenting a rare presentation and the associated challenges.
Declarations
Ethics approval and consent to participate
This case report was conducted in accordance with the declaration of Helsinki. The collection and evaluation of all protected patient health information was performed in a health insurance portability and accountability Act. we know of no conflicts of interest associated with this publication.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Competing interests
Not applicable
Funding
None
References
- MALKAOUI, wadiaa .Thymomas Retrospective study about 35 cases.
Publisher | Google Scholor - Khan, Abdul, Jain, Akriti G., Faisaluddin, Mohammed, et al. (2019). Cardiac Tamponade in the Setting of a Thymoma. Cureus, 11(6).
Publisher | Google Scholor - Engels EA, Pfeiffer RM. (2003). Malignant thymoma in the United States: demographic patterns of incidence and associations with subsequent malignancies. Int J Cancer., 105:546-551.
Publisher | Google Scholor - Woldow A, Kotler M, Goldstein S, Milcu M. (1995). Thymoma with pericardial tamponade. Clin Cardiol.
Publisher | Google Scholor - Engels EA. (2010). Epidemiology of thymoma and associated malignancies. J Thorac Oncol., 5:S260-S265
Publisher | Google Scholor - Wright CD, Kessler KA. (2005). Surgical treatment of thymic tumors. Cardiovascular surgery Semin Thorac., 17:20-26
Publisher | Google Scholor - Takanami I, Takeuchi K, Naruke M. (1999). Large non-invasive thymoma with a natural history of twenty-one years. J Thorac Cardiovascular Surg., 118:1134-1135.
Publisher | Google Scholor - Masaoka A. (2010). Thymoma staging system. J Thorac Oncol. 5:304-312.
Publisher | Google Scholor - Ströbel P, Bauer A, Puppe B, et al. (2004). Tumor recurrence and survival in patients treated for thymomas and thymic squamous cell carcinomas: a retrospective analysis. J Clin Oncol., 22:1501-1509.
Publisher | Google Scholor - Whiting, Adrian, Reyes, Jonathan Vincent M., Ahmad, Saad, Et Al. (2021). Thymic cancer: A not-soindolent cause of pericardial effusion. Annals of Medicine and Surgery, 71:102866.
Publisher | Google Scholor