Case Report
Thoracic Actinomycosis Masquerading as Malignancy: A Case Report
1Department of Thoracic Surgery, CHU Hassan II-Fès, Morocco.
2Faculty of Medicine and Pharmacy, Sidi Mohamed Ben Abdellah University, Fès, Morocco.
*Corresponding Author: F. Lamouime,Department of Thoracic Surgery, CHU Hassan II-Fès, Morocco.
Citation: F. Lamouime, M. Rhaouti, M. Lakranbi, Y. Ouadnouni, M Smahi. (2024). Thoracic Actinomycosis Masquerading as Malignancy: A Case Report. International Journal of Medical Case Reports and Reviews, BioRes Scientia Publishers. 3(4):1-6. DOI: 10.59657/2837-8172.brs.24.050
Copyright: © 2024 F. Lamouime, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: March 11, 2024 | Accepted: March 28, 2024 | Published: May 06, 2024
Abstract
Actinomycosis is a rare, specific, non-contagious bacterial infection characterized by purulent and granulomatous manifestations. It often presents challenges in diagnosis, with thoracic localization mimicking tuberculosis or cancer. We present the case of a 38-year-old chronic smoker admitted for the evaluation of a left anterior chest wall tumor. Clinical and radiological assessments revealed two left anterior parietal masses with pleuropulmonary invasion. Histological examination confirmed actinomycosis, prompting antibiotic therapy with intravenous Penicillin G followed by protected amoxicillin. The patient exhibited a positive clinical response. Thoracic actinomycosis, though benign, poses diagnostic challenges due to its deceptive radio-clinical presentation. Anatomopathological study becomes crucial to identify characteristic signs. The primary management involves tailored medical treatment. Actinomycosis should be considered a diagnosis of exclusion, especially when ruling out common causes of thoracic wall swellings.
Keywords: thoracic; infection; cervicofacial; non-contagious; radiological
Introduction
Actinomycosis is a specific, rare, and non-contagious bacterial infection, often chronic and predominantly affecting the cervicofacial region. It manifests as à purulent and granulomatous condition caused by Gram-positive anaerobic bacteria. Thoracic involvement accounts for 15% to 30% of reported cases. The prevalence has decreased with improved socioeconomic conditions and the advent of antibiotic therapy. Thoracic actinomycosis typically occurs in individuals with weakened immune systems. The clinical and radiological presentation is deceptive and can mimic bronchopulmonary cancer or pulmonary tuberculosis.
Observation
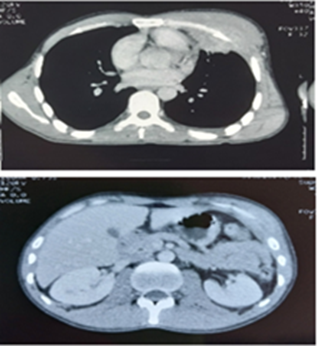
A 33-year-old chronic smoker presented with a two-month history of left anterior chest pain, non-radiating, accompanied by a cough producing mucous expectorations occasionally streaked with blood. The patient also reported two progressively enlarging masses located retro-mammary and at the left base of the thorax, along with unspecified weight loss. Clinical examination revealed poor oral hygiene and inflammatory signs associated with the two retro-mammary and left basithoracic swellings, without other associated symptoms. Biological assessment showed neutrophil-predominant leukocytosis with a count of 12,000. Sputum examination for Koch's bacillus was negative, and serologies for HIV, HBV, HCV, and syphilis were also negative. Frontal chest X-ray revealed no abnormalities. Radiological investigations, including thoracoabdominal CT scan, indicated a soft tissue lesion in the left thoracic wall causing rib destruction with ipsilateral pleuropulmonary and mediastinal involvement. Signs of carcinomatous lymphangitis and mediastinal lymphadenopathy were noted. Additionally, another soft tissue lesion was observed in the left hypochondrium Figure 1.
Figure 1: Two CT scan sections illustrating two invasive lesions, one affecting the left thoracic soft tissues, leading to costal lysis with ipsilateral pleuro-pulmonary and mediastinal involvement, and the other involving the soft tissues of the left hypochondrium.
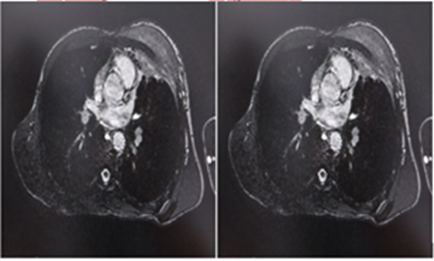
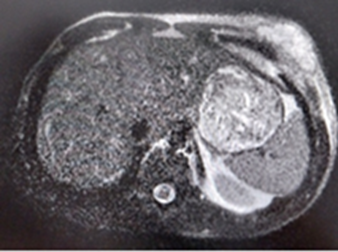
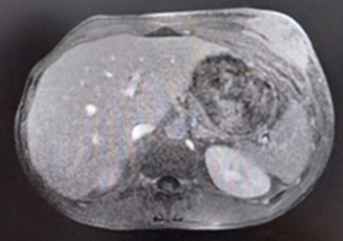
Thoracic MRI revealed two soft tissue processes involving the left anterior thoracic wall, hypointense on T1 and hyperintense on T2, enhancing post-contrast. These measured 61*26 and 32*19 mm, infiltrating the left pectoralis major muscle, extending into the pre- and retro-pectoral spaces, infiltrating the costal cartilages, intercostal and pleural spaces, with pleural effusion and adjacent pulmonary consolidation. (Figures 2,3 and 4).
Figure 2: Two axial sections in T1 FATSAT-weighted sequence revealing an invasive tissue process of the left thoracic wall with hypointensity.
Figure 3: Axial section in T2-weighted sequence illustrating a lesion with hypersignal in the soft tissues of the left hypochondrium.
Figure 4: Axial section in T2-weighted sequence demonstrating a lesion with hypersignal in the soft tissues of the left hypochondrium.
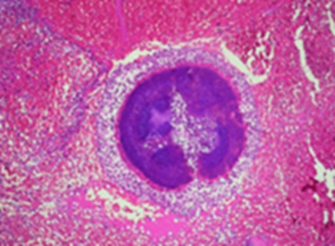
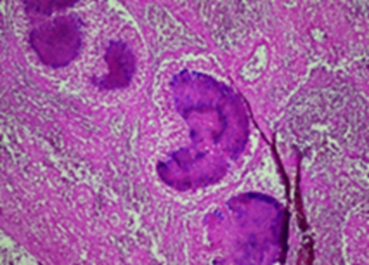
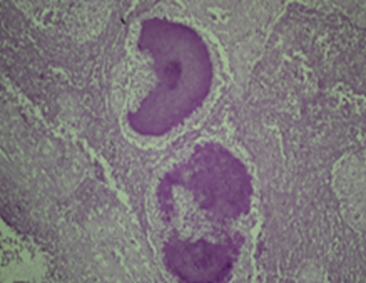
Histopathological examination, following an initial inconclusive trucut biopsy, revealed no signs of malignancy or tuberculosis. A second surgical biopsy confirmed actinomycosis, with positive special stains for "PAS" and "GRAM." (Figures 5,6 and 7).
Figure 5: Actinomycosis: Clusters of thick, basophilic, filamentous, short, and non-septated organisms (X40).
Figure 6: Actinomycosis: Zone of fibrosarcomatous transformation deep within, exhibiting a fishbone architecture (x10).
Figure 7: Actinomycosis: GRAM STAINING OF Clusters of microorganisms (X40).
Treatment involved intravenous Penicillin G at 10 million units per day for two weeks, followed by oral amoxicillin-clavulanate at 3 grammes per day for 6 months.
The patient demonstrated a favorable clinical evolution marked by weight gain, reduction in the size of the two masses, and alleviation of pain.
Patient Consent
The patient provided informed consent.
Discussion
Actinomycosis is an infectious disease caused by filamentous anaerobic bacteria of the order Actinomycetales, belonging to the class Actinomycetes, the family Actinomycetaceae, and the genus Actinomyces [1]. Contrary to what the term "actinomycosis" might suggest, it is not a mycotic infection but rather a bacterial infection caused by saprophytic bacilli present in the natural cavities of the human body. There are 14 species, of which six can be responsible for diseases in humans. The flagship species is A. israelii, most commonly recognized in thoracic actinomycosis [1]. The typical mode of contamination is endogenous, with mucosal rupture serving as the primary step in the progression towards pathogenicity. Examples include instances where actinomycosis occurs following dental procedures, trauma, surgery, or aspiration [2]. Actinomycosis predominantly impacts adults aged 20 to 60, with a peak incidence around 40 years old. Its occurrence is less frequent in children, accounting for fewer than 10% of reported cases, and typically presenting between the ages of 3 and 6. The scarcity of this condition in children is attributed to prompt dental caries treatment, the natural loss of teeth, and the absence of periodontal diseases [3]. Facial localization is the most common, accounting for 55% of cases, while abdominal-pelvic forms represent 20% of cases. Thoracic forms represent 15–20%, and can involve the pleura, mediastinum, or thoracic wall [4]. The occurrence of actinomycosis seems to have decreased over the last four decades, accompanied by less severe clinical manifestations, a trend likely influenced by improved hygiene practices. Thoracic involvement ranges from 15% to 50
Conclusion
Diagnosing thoracic actinomycosis poses à challenge due to its misleading clinical and radiological presentation, often resembling tuberculosis or cancer. Therefore, the importance of histopathological examination in identifying specific signs of actinomycosis cannot be overstated. The preferred therapeutic strategy mainly involves medical management, and invasive procedures are generally not required when initiated promptly.
References
- sebald M. (1996). Actinomycoses à bactéries anaérobies. Ecycl Med Chir. 8:6.
Publisher | Google Scholor - Wilson.R, Sande.M, Drew A, STAT W.L. (2001). «Currentdiagnosis&treatment in infectiousdiseases» New york: Lange Medical Books/McGraw-Hill.
Publisher | Google Scholor - Msougar Y, Fenane H, Maidi M, Benosman A. (2013). L’actinomycose thoracique multiple chez l’immunocompétent. Pan Afr Med J, 16 :1-5.
Publisher | Google Scholor - Souadka A, Ouadfel J, Jalil A, Benjelloun S. (1992). L’Acctinomycose Abdominale Pseudotumorale à propos de deux cas. Médecine du Maghreb, 39.
Publisher | Google Scholor - Hall.V. (2007). « Actinomyces-Gatheringevidence of humancolonization and infection » Anaerobe Reference Unit.
Publisher | Google Scholor - Molina E, Delhom E, Gallix B, Bruel J.M. (2005). Colites infectieuses, iatrogènes et autres colites rares. Ecycl Med Chir (Elsevier, Paris). Radiodiagnostic Appareil Digestif, 33-430-A-70.
Publisher | Google Scholor - Webb WR, Sagel SS. (1982). Actinomycosis involving the chest wall: CT findings. AJR, 139:1007-1009.
Publisher | Google Scholor - Hoekstra CJ, Hoekstra OS, Teengs JP, Postmus PE, Smit EF. (1999). Thoracicactino mycosisimagingwith fluorine-18 fluorodeoxyglucose positron emission tomography. ClinNucl Med, 24:529-530.
Publisher | Google Scholor - Garner J.P, Macdonald M, Kumar P.K. (2006). Abdominal Actinomycosis. International Journal of Surgery, 20 :1-8.
Publisher | Google Scholor - Park JY, Lee T, Lee H, Lim HJ, Lee J, Park JS, et al. (2014). Multivariate analysis of prognostic factors in patients with pulmonary actinomycosis. BMC infect Dis, 14 :1-7.
Publisher | Google Scholor