Case Report
This Paper Provides a Description of a Rare Case of a Gestational Trophoblastic Tumor of The Choriocarcinoma Type That Has Metastasized to The Brain, Lung and Kidney
- Analida Yovana-Martínez 1*
- Dana Sulieth-Mena 2
- Lady Johanna-Díaz 3
- Ignacio Salgado Castañeda 4
- Andres Enrique-Becker 5
1Neurology Resident, University of SINU Cartagena, Colombia.
2Doctor, Antonio Nariño University Bogotá, Colombia.
3Gynecology and obstetrics Resident, FUCS Health Sciences University Foundation Bogotá, Colombia.
4Neurologist, FUCS Health Sciences University Foundation Bogotá, Colombia.
5Neurology Resident, SINU University Cartagena, Colombia.
*Corresponding Author: Analida Yovana-Martínez, Neurology Resident, University of SINU Cartagena, Colombia.
Citation: Yovana-Martínez A., Sulieth-Mena D., Johanna-Díaz L., Castañeda I. S., Enrique-Becker A. (2024). This Paper Provides a Description of a Rare Case of a Gestational Trophoblastic Tumor of The Choriocarcinoma Type That Has Metastasized to The Brain, Lung and Kidney, Journal of BioMed Research and Reports, BioRes Scientia Publishers. 5(2):1-9. DOI: 10.59657/2837-4681.brs.24.088
Copyright: © 2024 Analida Yovana-Martínez, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: May 28, 2024 | Accepted: July 15, 2024 | Published: July 27, 2024
Abstract
Introduction: Choriocarcinoma is a type of gestational trophoblastic tumor, with approximately 20% of patients requiring treatment for malignant sequelae after the evacuation of a hydatidiform mole. Therefore, rigorous follow-up with quantitative levels of human chorionic gonadotropin (hCG) is essential. This type of tumor occurs in around 1 in every 20,000 to 40,000 pregnancies, with a 2-3% risk following a complete mole.
Case Report: A clinical case is described of a patient with metastatic choriocarcinoma to the brain, lungs, and kidney, the latter being of low prevalence. The patient did not receive medical follow-up after a complete hydatidiform mole and was diagnosed due to neurological symptoms. Thus far, she has experienced a favorable evolution under hCG level monitoring, although with complications secondary to acute hemorrhages in disseminated organs, such as the brain.
Discussion: Gestational trophoblastic diseases are proliferative disorders of the placental trophoblast, including premalignant conditions or true neoplastic gestational trophoblastic tumors. Choriocarcinoma tends to spread widely via hematogenous route and is associated with distant metastasis. It has been reported to commonly metastasize to the lungs and vagina, and less frequently to the liver, brain, kidneys, and gastrointestinal tract. Symptoms of metastatic lesions are usually secondary to acute hemorrhages in the organ to which they spread, as in the case of the patient.
Conclusion: The optimal management of this disease depends on the type of specialized center, pathology review, and evidence-based treatment guidelines. Given the rarity of trophoblastic tumors, as well as the associated diagnostic challenges, it is crucial to follow up on hydatidiform moles to prevent metastasis, as in the case of this patient.
Keywords: gestational trophoblastic tumor; choriocarcinoma; brain metastasis; human chorionic gonadotropin hormone; lung metastasis; high risk choriocarcinoma
Introduction
Choriocarcinoma, categorized as a gestational trophoblastic tumor, poses a notable risk, as evidenced by the fact that 20% of patients experience malignant complications post-evacuation of a hydatidiform mole. Therefore, diligent follow-up through quantitative hCG level monitoring becomes imperative. This particular tumor manifests in approximately 1 in 20,000 to 40,000 pregnancies, with a 2-3% risk post-complete mole (0.1-0.5% in incomplete mole) [1]. It stands out as the most common trophoblastic tumor, exhibiting a diverse range of presentations, typically emerging around the age of 30. Choriocarcinoma can originate from various gestational, with statistics indicating 50% occurrence after a full-term pregnancy, 25% following a molar pregnancy, and another 25
Case Presentation
A 38-year-old female patient was admitted to the emergency room with an altered state of consciousness, seizure from focal motor to bilateral tonic-clonic onset lasting 3 minutes with recovery of consciousness and a new similar episode during the assessment. The postictal period was 15 minutes. Treatment was started with levetiracetam (500 mg every 12 hours) with an adequate response. During the evaluation, the patient presented with vaginal bleeding, with a report of positive qualitative beta subunit chorionic gonadotropin. Family members reported that she had metrorrhagia for one month. The last pregnancy was 10 months prior, with evidence of a molar pregnancy, and was carried out for curettage, with pathology revealing gestational trophoblastic disease type complete hydatidiform mole. The patient was lost to follow-up and did not receive control treatment. In the 2 weeks prior to admission, she presented intense headache, changes in behavior due to aggressive and irritable behavior, and seizures.
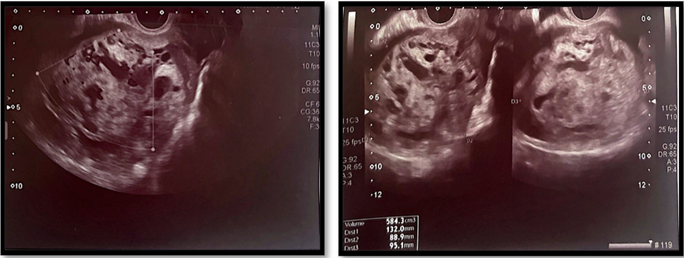
During the current evaluation, on ultrasonography, an enlarged uterus was found, and multiple endometrial cystic foci configured a mass with a snowstorm pattern, measuring 108x66x70 mm and having a volume of 264 cc; these findings are suggestive of molar pregnancy (Figure 1). On physical examination, she was febrile and drowsy and required invasive mechanical ventilation and vasopressor support. Respiratory sounds with bilateral rhonchi and abundant mobilization of secretions were observed. Her chorionic gonadotropin concentration was 219181 mIU/ml in her blood (Table 1). Her obstetric curettage revealed an enlarged uterus (11 cm), a curettage product with scant ovular remnants, and difficult bleeding control.
Figure 1: Ultrasonography. Patient ultrasonography revealed multiple endometrial cystic foci configuring a mass with a snowstorm pattern measuring 108x66x70 mm and with a volume of 264 cc, suggesting molar pregnancy.
Table 1: Paraclinical.
| Gravindex | Positive | |
| Calcium | 8.06 | mg/dl |
| Chlorine | 105 | mEq/L |
| Potassium | 3.12 | mEq/L |
| Sodium | 137 | mEq/L |
| Bun | 6.8 | mg/dl |
| Creatinine | 0.60 | mg/dl |
| H.B. | 11.7 | |
| HTO | 31.1 | |
| Neutrophils | 5420 | uL |
| Lymphocytes | 4.1 | % |
| Neutrophils | 80.4 | % |
| BHCG | 219181 | mUl/ml |
| Total, Bilirubin | 0.59 | mg/dl |
| Direct Bilirubin | 0.42 | mg/dl |
| Indirect Bilirubin | 0.17 | mg/dl |
| TGO-AST | 27 | U/L |
| TGP-ALT | 15 | U/L |
| PTT | 30.4 | sec |
| PTT | 10.8 | sec |
| INR | 1.07 | |
| Lactate | 0.68 | mmol/L |
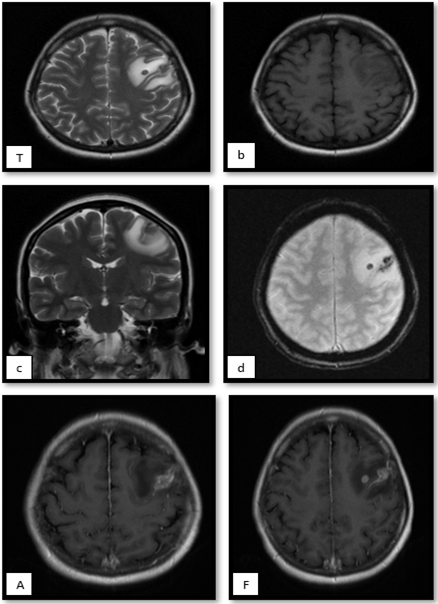
Magnetic resonance imaging of the brain was performed (Figure 2) and revealed an intra-axial lesion in the deep white matter of the left frontal lobe measuring 5 mm and was oval, with peripheral contrast enhancement, which is associated with extensive vasogenic edema (thickness up to 12 mm). Moreover, in ferromagnetic sequences, bleeding within the lesion is evident. Without ruling out neuro infection, paraclinical tests are performed, with a complete blood analysis revealing anemia and mild hypokalemia, as well as metabolic acidosis partially compensated for by mild oxygenation disorder. Lumbar puncture showed no signs of an infectious process; however, there was a report of elevated hCG in the CSF. (Table 2).
Figure 2: Magnetic resonance imaging of the brain. Patient magnetic resonance imaging of the brain showing intra-axial lesion in the deep white matter of the left frontal lobe that measures 5mm, oval, isointense on T1 (B), hypointense on T2 (AC), which is associated with extensive vasogenic edema (thickness up to 12mm). and in ferromagnetic sequences, bleeding within the lesion is evident, characteristic of these. With peripheral contrast enhancement (F).
Table 2: CSF.
| CSF | ||
| Glucose | 67 | |
| Total Proteins | 14 | |
| VDRL Serology | NR | mg/dl |
| White | 0 | |
| Red | 2 | |
| Neutrophils | 0 | |
| Lymphocytes | 0 | % |
| Fresh Erythrocytes | 100 | % |
| Created Erythrocytes | Either | |
| Crop | Negative | |
| Chinese Ink | Negative | |
| hCG | 747 | |
| Gram | Negative | mUl/ml |
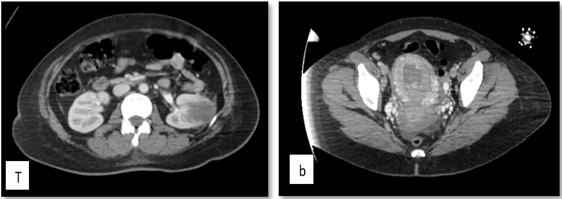
Chest tomography (Figure 3) showed evidence of bilateral pleural effusion predominantly on the right. Numerous nodules with soft tissue density were identified in the right hemithorax. The largest projected in the posterior segment of the basal lobe had a long axis diameter of 68 mm. In the left hemithorax, nodules with the same characteristics were identified, the largest of which were projected in the anterior segment of the apical lobe with a long axis diameter of 12 mm.
Figure 3: Patient chest tomography revealed numerous nodules with a soft tissue density in the right hemithorax. The largest projected in the posterior segment of the basal lobe had a long axis diameter of 68 mm. In the left hemithorax, nodules with the same characteristics were identified, the largest of which were projected in the anterior segment of the apical lobe with a long axis diameter of 12 mm.
Given these findings, an extension of the search for lesions was carried out via neck tomography, revealing numerous lymph nodes in different spaces of the neck, the largest of which were projected to left station III with a diameter of 12 mm in the short axis. In addition, in the bone system, a small lytic lesion projected on the vertebral body of C5. On tomography of the abdomen and pelvis (Figure 4), in the middle third of the left kidney, an ill-defined hypodense image of 34 × 33 mm with soft tissue density and a central uterus with a thick endometrium of 31 mm of heterogeneous content were observed. The other tumor markers were reported (Table 3).
Figure 4: Abdominopelvic Tomography. Patient abdominopelvic tomography revealed, in the middle third of the left kidney, an ill-defined hypodense image of 34 × 33 mm with soft tissue density and a central uterus with a thick endometrium of 31 mm of heterogeneous content.
Table 3: Tumor Markers.
| Tumor Markers | ||
| ANTIGEN 19-9 | 10.22 | U/mL |
| LDH | 434 | U/L |
| AC 125 | 21.30 | U/ml |
| Carcinoembryonic GA | 3.54 | ng/ml |
| Serum Alpha-Fetoprotein | 2.66 | ng/ml |
| Alpha-Fetoprotein in CSF | <0> | Ul/mL |
| BHCG IN CSF | 747.90 | mUl/ml |
Progressive weaning of vasopressor support and ventilation was initiated due to clinical and hemodynamic stability. If metastatic lesions are suspected, a biopsy of the lung lesion is performed. Pathology revealed a lower left segmental lobectomy: a violet‒brown lobectomy product measuring 3.5x1x1 cm and a violet-colored nodular lesion measuring 0.6x0.6x0.6 cm in apparent contact with the pleura. With respect to the evidence of involvement by choriocarcinoma, immunohistochemistry studies have shown reactivity in the population affected by HCG, CKAE1/AE3, P63, PLAP, MUC4, INHIBINA and SALL4. P53: 50%. KI67: 70%. Pathology of the obstetric curettage material revealed atypical cells that suggested gestational tumors, with reactivity in the population with GATA-3, PLAP, CKAE1/AE3 or HCG. There was patchy reactivity with SALL4, INHIBIN and MUC4. No reactivity with P63. P53: NEGATIVE. KI67: 30%. A report of choriocarcinoma was available. Patient ventilatory and hemodynamic stability were successfully achieved. With symptomatic improvement.
Finally, given the diagnosis of FIGO IV gestational trophoblastic neoplasia of the choriocarcinoma type, treatment with chemotherapy was chosen to manage the high-risk trophoblastic neoplasia that the patient presented (cyclophosphamide, etoposide, methotrexate, vincristine, and dactinomycin in combination with folic acid, dexamethasone, and pegfilgrastim for complete the diagram). During the course of chemotherapy, in the second cycle, secondary intracranial hemorrhage was documented as a lesion already described in the brain MRI, clinically with evidence of right hemiplegia and focal motor crises in the right upper limb; thus, the dose was increased. of levetiracetam with seizure resolution. In addition, supplemental oxygen must be provided at low flow to maintain perfusion oxygenation. The values of the patients who underwent follow-up with hCG are shown in Figure 4.
Discussion
Gestational trophoblastic diseases are described as proliferative disorders of the placental trophoblast. These may be non-neoplastic proliferations, known as partial and complete hydatidiform moles; which are premalignant conditions; or true neoplastic conditions, such as gestational trophoblastic tumors. Within this group, different pathologies are known, such as gestational choriocarcinoma, placental site trophoblastic tumor, epithelioid trophoblastic tumor, and placental site nodule recently added to the guidelines. Collectively referred to as gestational trophoblastic neoplasms, each of these conditions arises from various subtypes of placental trophoblasts with different pathobiology’s [1].
It has been noted that tumors may develop following various gestational event, with 50% arising post-pregnancy, 25
Conclusion
Identifying gestational trophoblastic tumors poses challenges due to their relative rarity and overlap with common gynecologic tumors. Early and accurate diagnosis is essential for determining the appropriate treatment, particularly for patients with gestational choriocarcinoma, known for its favorable response to chemotherapy. Monitoring both complete and partial moles with serum hCG, a key marker in surveillance, is crucial. Choriocarcinoma typically spreads hematogenous, and our patient exhibited metastases to the brain, lung, and kidney, classifying them as ultrahigh risk according to FIGO. Complications, such as acute hemorrhages or intracranial hemorrhage, underscore the importance of adequately controlling molar pregnancies to minimize acute complications and promptly identify malignant sequelae.
Declarations
Authors Contribution
Analida Martínez: Conceptualization, Research, Methodology, Supervision, writing (original draft), Writing (review and editing of the manuscript).
Ignacio Salgado: Research, Methodology, Visualization, writing (review and editing of the manuscript).
Dana Mena: Writing (original draft), Writing (review and editing of the manuscript).
Andres Becker: Visualization, writing (review and editing), Investigation.
Lady Diaz: Writing (original draft), Writing (review and editing of the manuscript), Visualization.
Ethical Considerations
There are no ethical considerations to report in the completion of this manuscript.
Conflicts of Interest
Through this we can assert that none of those present have any conflicts of interest.
Funding
The study received no funding from any institution or company.
References
- Strickland, A.L., Gwin, K. (2022). Gestational Trophoblastic Disease-Rare, Sometimes Dramatic, And What We Know So Far. In Seminars in Diagnostic Pathology. 39(3):228-237.
Publisher | Google Scholor - Seckl MJ, Fisher RA, Salerno G, et al. (2000). Choriocarcinoma And Partial Hydatidiform Moles. Lancet. 356(9223):36-93.
Publisher | Google Scholor - Picone, O., Castaigne, V., Ede, C. Fernandez, H. (2003). Cerebral Metastases of a Choriocarcinoma During Pregnancy. Obstetrics & Gynecology, 102(6):1380-1383.
Publisher | Google Scholor - Soper, J. T. (2006). Gestational Trophoblastic Disease. Obstetrics & Gynecology, 108(1):176-187.
Publisher | Google Scholor - Tuncer ZS, Bernstein MR, Goldstein DP, Berkowitz RS. (1999). Outcome of Pregnancies Occurring Before Completion of Human Chorionic Gonadotropin Follow-Up in Patients with Persistent Gestational Trophoblastic Tumor. Gynecol Oncol. 73:345-347.
Publisher | Google Scholor - Pei Hui. (2019). Gestational Trophoblastic Tumors: A Timely Review of Diagnostic Pathology. Arch Pathol Lab Med. 143(1):65-74.
Publisher | Google Scholor - Mao, T.L., Kurman, RJ, Huang, C.C., Lin, M.C., Shih, I.M. (2007). Immunohistochemistry Of Choriocarcinoma: An Aid in Differential Diagnosis and In Elucidating Pathogenesis. The American journal of surgical pathology, 31(11):1726-1732.
Publisher | Google Scholor - Bogani G, Ray-Coquard I, Mutch D, Vergote I, Ramirez PT, et al. (2023). Gestational Choriocarcinoma. Int J Gynecol Cancer. 33(10):1504-1514.
Publisher | Google Scholor - Horowitz Michael Bruce, Walter A. Hall. (1991). Central Nervous System Germinomas: A Review. Arch Neurol. 48(6):652-657.
Publisher | Google Scholor - Dadlani R., Furtado S., Ghosal N., Prasanna K., Hegde A. (2010). Unusual Clinical and Radiological Presentation of Metastatic Choriocarcinoma to The Brain and Long-Term Remission Following Emergency Craniotomy and Adjuvant EMA-CO Chemotherapy. J. Cancer Res. Ther. 6(4):552.
Publisher | Google Scholor - Hayashi S, Abe Y, Tomita S, et al. (2015). Primary Non-Gestational Pure Choriocarcinoma Arising in The Ovary: A Case Report and Literature Review. Oncol Lett. 9(5):2109-2111.
Publisher | Google Scholor - FIGO Committee on Gynecologic Oncology. (2009). Current FIGO Staging for Cancer of The Vagina, Fallopian Tube, Ovary, And Gestational Trophoblastic Neoplasia. Int J Gynaecol Obstet. 105(1):3-4.
Publisher | Google Scholor - Eiriksson L, Dean E, Sebastianelli A, Salvador S, Comeau R, et al. (2021). Guideline No. 408: Management of Gestational Trophoblastic Diseases. J Obstet Gynaecol Can. 43(1):91-105.
Publisher | Google Scholor