Review
The Use of the Obstetric Vacuum Extractor for Rotational and Non-Rotational Vaginal Delivery
- Salvatore Felis *
- F. Cremonini
- E. Primizia, A. Tomasi
Obstetrics & Gynecology Department, IRCCS San Martino Hospital-Genova, Italy.
*Corresponding Author: Salvatore Felis,Obstetrics & Gynecology Department, IRCCS San Martino Hospital-Genova, Italy.
Citation: Felis S, Cremonini F, Primizia E, Tomasi A. (2023). The Use of the Obstetric Vacuum Extractor for Rotational and Non-Rotational Vaginal Delivery, Journal of Surgical Case Reports and Reviews, BRS Publishers. 2(1); DOI: 10.59657/2993-1126.brs.23.012
Copyright: © 2023 S. Felis, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: June 02, 2023 | Accepted: June 22, 2023 | Published: June 26, 2023
Abstract
Vacuum-assisted birth is a safe delivery method when performed by a skilled provider. Vacuum extraction can prevent prolonged second stage of labor, birth asphyxia in the presence of fetal distress, or when maternal pushing is contraindicated. However, vacuum-assisted births, especially those involving mid-pelvic rotational deliveries, have increasingly been replaced by cesarean sections, even though they generally carry a potentially higher risk for women and future children. This article provides detailed information on the indications and contraindications of vacuum-assisted birth, as well as the basic principles of the vacuum technique. It also includes a dedicated section on vacuum extraction for rotational births. When obstetric caregivers are knowledgeable, trained, and experienced in these techniques, vacuum extraction can greatly enhance the safety of childbirth.
Keywords: vacuum extractor; vaginal delivery; birth asphyxia; fetal distress; mid-pelvic
Introduction
While the cesarean section rate has been increasing at an alarming rate worldwide, the utilization of operative vaginal birth has declined over time and, in some countries, has even disappeared [1]. Temporal data indicate that the reduction in the rate of assisted vaginal birth has been inversely correlated with the increase in cesarean section numbers [2]. Particularly, births assisted with mid-pelvic rotation have become less common as there is a growing trend towards choosing cesarean section in the second stage [3]. This has led to a decrease in experience with the use of obstetric vacuum extraction for operative birth, for example, in North America [4]. These data should be a cause for concern, especially in contexts where maternal and perinatal mortality associated with cesarean section is high [5-7]. It has been shown that preventing a prolonged second stage of labor through assisted vaginal birth reduces rates of postpartum hemorrhage, sepsis, and when fetal monitoring is present, intrapartum asphyxia [8,9]. Furthermore, women who deliver vaginally and their future offspring are not exposed to the risks associated with pregnancies in a uterus that has undergone previous surgical intervention. Despite these clear advantages, the rate of assisted vaginal birth remains low in many countries (Table 1) [1,10]. Within the European Union, there are significant differences in the use of operative vaginal birth (vacuum or forceps) and cesarean section [11]. To reduce unnecessary cesarean sections and increase the rate of vaginal births, the use of obstetric vacuum extraction is likely a more widely utilized method compared to forceps, as it is relatively easy to perform and teach [8].
| Country | Vacuum-Assisted Birth | Forceps-Assisted Birth | Cesarean section |
| Congo-Brazzaville, 2012 | <0> | 0,2 | 6,9 |
| Cyprus, 2010 | 2,5* | 52,2 | |
| Ghana, 2010 | 0,5 | <0> | 12,3 |
| Italy, 2010 | 3,4* | 38,0 | |
| Laos, 2010/2011 | 3,4 | 0,1 | 7,3 |
| Poland, 2010 | 1,4* | 34,0 | |
| Romania, 2010 | 0,5* | 36,9 | |
| Zambia, 2015 | 0,5 | 0,1 | 5,0 |
| Global WHO Survey | 2,6* | 25,7 |
Table 1: Percentage distribution of vacuum-assisted birth, forceps-assisted birth, and cesarean section in various countries [1,10].
Combined vacuum and forceps-assisted delivery
Indications, contraindications, and prerequisites for vacuum-assisted birth
Maternal indications for assisted vaginal delivery include the prolonged second stage of labor, maternal exhaustion, cardiac diseases or placental detachment, presumed non-reassuring fetal status resulting from a maternal or independent condition, as well as other fetal indications [9]. Non-cephalic and facial presentations are contraindications for vacuum-assisted birth. Fetal demineralization (e.g., osteogenesis imperfecta), connective tissue disorders, and a tendency to bleed due to hemophilia or thrombocytopenia are rare and relative contraindications. The risks of vacuum-assisted birth in these Cases must be balanced against the considerable risk of causing severe damage to the fetal head [9].
Since premature infants have a higher risk of developing cephalohematoma, neonatal jaundice, intracranial jaundice, and subgaleal hemorrhage, vacuum-assisted birth is not recommended before 34 weeks of gestation, and it is unclear whether forceps-assisted birth is safe before 36 weeks [9]. Good clinical practice dictates that vacuum-assisted birth should only be attempted when the woman consents to the procedure, the cervix is fully dilated, the membranes have ruptured, and the fetal head is engaged, which means that the largest circumference of the fetal head has passed the pelvic inlet, and in the occipital-anterior position, implying that the bony part of the skull is at or below the level of the ischial spines (station 0). It is important to note that significant caput or molding can misleadingly make the descent appear lower than it is. Therefore, abdominal palpation may be less deceptive and should always complement the internal examination [9, 12]. Other prerequisites include an empty bladder and the availability of competent personnel to perform neonatal resuscitation. Access to an operating room is preferable but not always feasible in low-income countries. Adequate uterine contractions reduce the possibility of vacuum-assisted birth failure. Increasing contractions with oxytocin can help establish effective contractions, and there should be a low threshold to initiate oxytocin when performing vacuum extraction [9, 12].
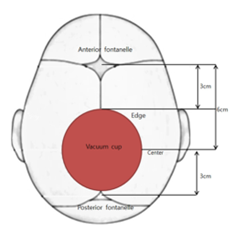
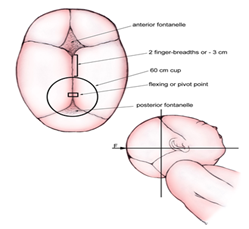
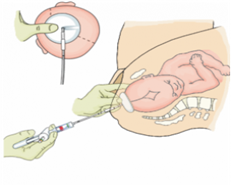
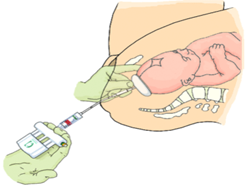
Materials and technique
Data on the optimal instrument for vacuum-assisted delivery is limited. The Cochrane review on this topic may be considered outdated as it largely predates the evidence applying the Kiwi Omnicup. In essence, the same principles apply to all types of vacuum extractors regarding technique, but the failure rates and complication rates may vary (Box 1). Cups that allow for high traction force (O'Neil, Bird) may also have a higher risk of fetal damage. The use of cups that allow for moderate traction force (Malmstrom, Kiwi Omnicup) may be more suitable, although some prefer the Bird OP cup in cases of difficult rotational delivery. Generally, 50 mm cups are used, and larger cups are rarely needed (the Kiwi Omnicup is only available in one size). Soft cups should generally be avoided [8,9,12]. Proper preparation of the procedure is essential before undertaking it (BOX 2). The cup should be positioned when there is no uterine contraction. There are different methods for inserting the cup into the vagina. A common technique is to widen the labia and take care not to damage the vaginal wall. One technique involves inserting the cup laterally and then tilting the outer rim of the cup toward the posterior vaginal wall. A soft cup can also be folded [12]. The most crucial part of the procedure is to position the cup on the flexion point (Fig. 1). The flexion point is located 3 cm from the center of the posterior fontanelle. If using a 5 cm cup, the cup's edge will be at the edge of the posterior fontanelle. Proper placement of the cup on the flexion point will promote flexion of the fetal head and thus result in a favorable position [14]. The Kiwi Omnicup has markings on the tube at 6 and 11 cm from the suction cup. In combination with finger length, these markings can be used to guide the cup's placement on the flexion point [15]. After placing the cup, palpation should be used to ensure that no maternal tissue is trapped between the cup and the fetal scalp. The vacuum should then rise promptly to 0.8 kg/cm2 [16,17]. Traction should be performed during contractions while the woman pushes to increase the force outward. The fingers of the dominant hand perform the traction, while the fingers of the non-dominant hand are positioned on the fetal head and the cup, typically using three fingers, with the thumb placed on the cup and the index and middle fingers on the fetal head [12]. Traction should be smooth, and jerky movements should always be avoided. The direction of traction should always follow the axis of the birth canal. The initial traction should generally be directed toward the floor of the delivery room. A common mistake is to pull too horizontally, in which case the head is pulled against the pubic symphysis, increasing the chances of slippage. If sufficient force can be developed with proper traction, there should be progress in the descent of the fetal head, with the first traction dislodging the fetal head and correcting the position, and the second traction resulting in significant descent. After that, with the third traction, the fetal head should (almost) exit [9,12]. The need for episiotomy should be considered when the head is crowning to reduce the risk of anal sphincter laceration. At the emergence of the head, the vacuum is released (for example by pressing the release button on the Kiwi Omnicup). The birth of the shoulders and trunk occurs in the same manner as in physiological vaginal delivery. The risk of shoulder dystocia should be kept in mind. In multiparous women, vacuum-assisted delivery is indicated in case of fetal distress with a favorable position but should be carefully considered in cases of prolonged labor, particularly with a poorly descended fetal head [9,12]. Some doctors apply pressure to the fundus simultaneously during vacuum-assisted delivery, especially in areas where cesarean section carries greater risks (Figure n. 1-13). In some low-income settings where a cesarean section is inaccessible or highly dangerous, symphysiotomy could be performed if vacuum-assisted delivery fails and recourse to the operating room is impossible or undesirable [18]. It is essential to provide post-procedure assistance in every vacuum-assisted delivery (Box 3).
Box 1: Most used vacuum cups.
|
Box 2: Preparation for Vacuum-Assisted Delivery.
*Some practitioners propose performing a translabial or transperineal ultrasound to predict failure of vacuum-assisted vaginal delivery, using the angle of progression between the pubic symphysis and fetal head, but this technique still requires confirmation [13]. |
Box 3: After the procedure.
|
Technique of Application of Obstetric Vacuum Extractor
The technique of applying the Vacuum Extractor is based on the following principles:
The cup adheres firmly to the fetal scalp without compressing the cranial sphere or altering its internal pressure (more than what occurs in a spontaneous birth). It can be left in place without causing harm.
Creating a vacuum between the cup and the scalp forms an artificial birth tumor, which is essential for the cup to grip and allow traction to be exerted. During the traction maneuver, the scalp undergoes stretching up to the limit of its elasticity, but the force applied to it is usually lower than what is needed to cause detachment, as excessive force would result in the cup coming off. The main action performed by the vacuum extractor on the fetus is pulling, in addition to the force exerted by uterine contractions from behind.The external genitalia and the vulvovaginal orifice are separated, and the cup is inserted by making a cut and applying slight pressure on the fork and the posterior vaginal wall. The cup is placed on the "flexion point," which is located along the sagittal suture approximately 3 cm in front of the posterior fontanelle and about 6 cm from the anterior fontanelle. Since the cup diameters are approximately 5-6 cm, the cup's edge should be positioned 3 cm from the anterior fontanelle. The creation of vacuum should be gradual, and the suction pressure is increased by 0.2 kg/cm2 every 2 minutes until it reaches a value of 0.8 kg/cm2. Once the cup has firmly adhered, traction is applied in coordination with uterine contractions. Traction is temporarily halted during the pause between contractions and resumed consistently, without sudden movements, during active uterine contractions.
If the fetal head is already rotated and situated between the middle and lower part of the pelvis, tractions will initially be applied in a downward and backward direction. As the head descends further and reaches the lower pelvic strait, tractions will be directed forward and upward. The operator maintains continuous monitoring of the secure attachment of the vacuum cup to the fetal head and applies traction with a force that is never excessive. The obstetric vacuum can withstand a traction force equivalent to a weight of 12-13 kg (forceps can reach 30-35 kg).
Figure 1: Obstetric Vacuum Extractor Omni Cup
Figure 2a
Figure 2b
Figure 2a: Correct positioning of the vacuum application. The cup is placed on the flexion point to maximize adherence to the fetal scalp, the center of the cup is located 6 cm from the anterior fontanelle and 3 cm from the posterior fontanelle, on the sagittal suture.
Figure 3a
Figure 3b
Figure 3a-b: Correct application of the Obstetric Vacuum Extractor. Downward traction axis.
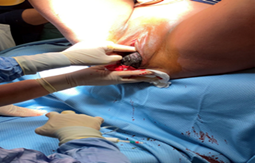
Figure 4: Application of Vacuum Extraction (personal photo)
Figure 5: Correct Application and Traction (personal photo)
Figure 6: Correct Application and Traction (personal photo)
Figure 7: Correct Application and Traction (personal photo)
Figure 8: Correct Application and Traction (personal photo)
Figure 9: Correct Application and Traction (personal photo)
Figure 10: Correct Application and Traction with Episiotomy Execution (personal photo)
Figure 11: Vacuum Extraction with PP on the perineal floor (personal photo)
Figure 12: PP on the perineal floor (personal photo)
Figure 13: PP on the perineal floor (personal photo)
Rotational delivery
The occiput posterior (OP) position often results from a deflexed fetal head. After placing the vacuum cup, the direction of traction is aimed at the flexion point, which promotes flexion. After flexion, the fetal head will often rotate on its own and emerge with the occiput anteriorly, although it can also emerge with the occiput posteriorly. In rotational delivery, it is extremely important, compared to non-rotational delivery, that the vacuum cup is positioned at the flexion point. The flexion point is often found further back than anticipated in the occiput transverse and OP positions [15,21,22].
Contrary to some claims, the need for rotation should be a significant factor in opting for vacuum-assisted delivery. When the correct traction line is applied, the fetal head will naturally rotate without the need for manual rotation of the cup. Manual rotation is unnecessary and can increase the risk of lacerations for both the mother and the baby. The Softcup should not be used for rotational delivery. However, the Kiwi Omnicup or any metal cup can be used for this purpose. Both the Kiwi Omnicup and the Bird OP-cup are specifically designed to be able to place the cup on the flexion point in cases of deflected OP position, where the flexion point is located deep in the posterior pelvis.
Failure and Complications
The decision to discontinue the procedure if there is no progress with subsequent tractions, or if delivery is not imminent after the third traction (one traction being equivalent to a contraction during which adequate traction force could be applied) or within 20 minutes, is based on common sense rather than concrete evidence [9]. The validity of these empirical rules can be questioned. For example, it is unclear whether five pulls with relatively low traction force pose a greater risk to the fetus compared to three strong pulls. Limited data is available to provide definitive answers to such questions, emphasizing the need for further research on assisted vaginal delivery during labor.
BOX 4: Reasons for vacuum extraction failure.
- Cup placement outside the flexion point: The cup should be placed at the flexion point of the fetal head to ensure a proper grip and successful extraction. If the cup is positioned incorrectly, it may result in failure.
- Incorrect traction direction: Inexperienced operators may tend to pull too early or horizontally. The traction direction should generally be directed dorsally/downward for most of the procedure.
- Large caput succedaneum: In rare cases, a large caput succedaneum (swelling of the fetal scalp) can make vacuum extraction challenging and may lead to failure.
- Insufficient uterine contractions: Adequate contractions are necessary for successful vacuum extraction. Sometimes, oxytocin may need to be administered to stimulate effective contractions.
- Cephalopelvic disproportion: If there is a significant size mismatch between the fetal head and the maternal pelvis, vacuum extraction may not be successful.
- Faulty or inadequate equipment
BOX 4: Reasons for vacuum extraction failure.
- Cup placement outside the flexion point: The cup should be placed at the flexion point of the fetal head to ensure a proper grip and successful extraction. If the cup is positioned incorrectly, it may result in failure.
- Incorrect traction direction: Inexperienced operators may tend to pull too early or horizontally. The traction direction should generally be directed dorsally/downward for most of the procedure.
- Large caput succedaneum: In rare cases, a large caput succedaneum (swelling of the fetal scalp) can make vacuum extraction challenging and may lead to failure.
- Insufficient uterine contractions: Adequate contractions are necessary for successful vacuum extraction. Sometimes, oxytocin may need to be administered to stimulate effective contractions.
- Cephalopelvic disproportion: If there is a significant size mismatch between the fetal head and the maternal pelvis, vacuum extraction may not be successful.
- Faulty or inadequate equipment
Higher failure rates occur in obese women, macrosomic infants, cases of OP position, and when the vacuum is applied to the mid or upper part of the pelvis [9]. In several older studies, the Kiwi Omnicup was found to have a failure rate as high as 30% [23,24]. However, more recent studies have not confirmed such high failure rates, and it seems that the rates are lower when the procedure is performed by experienced practi-tioners [25]. It is important to emphasize that the failure rates of vacuum extraction can also be influenced by the safety of the technique itself. If excessive traction force is applied or if the technique is not performed correctly, particularly with deviations from the pelvic axis, it could potentially cause harm to both the woman and her fetus if the cup does not release appropriately. Maternal complications include postpartum hemorrhage and perineal lacerations, including anal sphincter tears. However, these are less frequent compared to forceps-assisted deliveries. Postpartum infections appear to be lower after operative vaginal delivery compared to cesarean section [26]. The most common neonatal complications are generally self-limiting or without long-term consequ-ences (cephalohematoma, jaundice, and retinal hemorrhage), but rarer complications can be severe and even life-threatening, such as intracranial injuries (epidural, subdural, intraparenchymal, and subarachnoid) and subgaleal hemorrhage. In the case of subgaleal hemorrhage, a newborn can experience significant blood loss into the potential space between the cranial periosteum and the aponeurosis. Additionally, shoulder dystocia, a condition where the baby's shoulders get stuck during delivery, may be more common after vacuum-assisted delivery compared to other methods. In 1998, the FDA issued a public health advisory emphasizing the importance of using proper indications and techniques in vacuum-assisted deli-veries, as well as the need to educate healthcare personnel about potential complications. It is crucial to ensure that neonatal staff is adequately informed by the obstetric team, especially in high-risk situations such as sequential instrument use or failed vacuum extraction with the fetal head stuck in the pelvis and requiring difficult extraction during a cesarean section. In such situations, the risk of adverse neonatal outcomes increases. Although, if performed correctly, vacuum-assisted delivery is associated with few harms to the mother and the newborn, it should not be performed if it can be safely avoided. In this regard, it is important to note the crucial role of continuous support during labor, which is increasingly challenging in many high-income countries, and has been shown to reduce the need for assisted vaginal delivery [27]. The use of delayed pushing in women with neuraxial analgesia has been recently discovered to not reduce the need for operative vaginal delivery. Similarly, contrary to previous beliefs, upright positions do not increase the likelihood of spontaneous vaginal delivery [28,29]. Vacuum extraction is a technique used in the second stage of labor to facilitate vaginal delivery in cases of prolonged second stage or fetal distress. When common sense and a set of safety precautions are followed, the procedure carries low additional risks for a physiological birth. Vacuum-assisted delivery is relatively straightforward to teach and learn.
Clinical Report of An Operative Vaginal Delivery (35). Operator ……………………………… Date …………………. Supervisor …………………………… | |
Indication ……………………………………………. CLASSIFICATION: perineal / low excavation / medium excavation FETAL WELL-BEING CTG: normal/ questionable/ pathological ROTATION > 45°: yes / no AMNIOTIC FLUID: clear/ meconium ………… | |
Prerequisites Place: delivery room / operating room / other …… Analgesia: local/ regional/ epidural/ other…… Consent: verbal / written Catheterization: yes/no Obstetric Visit Dilatation ……………………. Presentation …………………. Station ………………………. Location ……………………… Childbirth tumor ………………. Amniorexi ……… spontaneous rupture …… | |
Procedure Tool used: … Vacuum extractor: Silastic/ Kiwi/ Metallic Forceps: rotational/ non-rotational Number of tractions …………………… Traction force ……………………… Strength of maternal drives: ………………. Spontaneous/instrumental secondment Episiotomy: yes/no Perineal injury: I / II / III / IV degree or other | Use of a later tool: yes/no Visit before the second application Dilatation ……………………. Presentation …………………. Station ………………………. Location ……………………… Childbirth tumor ………………. Reason for application: … Cesarean section yes/no CT indication: ………………… |
Newborn: M/F Weight: Apgar 1’……5’……10’…. Ph Cord Arteriosus…. Venous…… Base Deficit Arterial…Venous Cord… | |
POSTPARTUM Level of care: routine/ intensive Syntocinon infusion: yes/no Catheter: yes/ no removed………………. Vaginal tamponade: yes/no removed………………. Painkillers: yes/no which ones……………. doses…………. Thromboembolic risk: low/medium/high Thromboembolic prophylaxis: yes/no Date………………………. Signature | |
References
- Abdullaev M.Zh., Smurygina L.V. (2015). Organization of physical culture and health and sports events in a comprehensive school. Bukhara State University. Tutorial. Designed for teachers of faculties of physical education, sports colleges, sports schools and secondary schools. Bukhara: publishing house
Publisher | Google Scholor - Ivanova-Tyurina V, V. Smurygina L.V. (2022). Theory and methodology of track and field athletics (Training in the types of track and field athletics), Educational and methodological guide. Chirchik, 88.
Publisher | Google Scholor - Smurygina L. V., Vasilyeva E. B. The content of the training methodology for girls in the 400-meter running // Young scientist, 3:1035-1037.
Publisher | Google Scholor - Smurygina L.V., Ganibaev I.D. Organization and methods of training middle-distance runners. Toolkit. Tashkent, UzGosIFK, 80.
Publisher | Google Scholor - Smurygina L.V. (2013). Conducting scientific research in track and field athletics. Teaching aid. Tashkent, UzGIFC, 7-24.
Publisher | Google Scholor - Soliev Iqrorjon Roziqovich, Smurygina Larisa Vladimirovna. (2021). TECHNOLOGIES FOR PREPARING RUNNERS AVERAGE DISTANCES TO COMPETITION //Emergent: JOURNAL OF EDUCATIONAL DISCOVERIES AND LIFELONG LEARNING (EJEDL). 2776-0995. Indonesian Journal Publisher, 2(10).
Publisher | Google Scholor - Soliev I.R., Smurygina L.V. Olimov, M. S., Rasulova, T. R., Ivanova-Tyurina, V. V., Karimov. (2021). Ф. М. ЎРТА МАСОФАГА ЮГУРУВЧИЛАРНИ МУСОБАҚАЛАРГА ТАЙЁРЛАШ ТЕХНОЛОГИЯСИ. Central Asian Research Journal for Interdisciplinary Studies (CARJIS), 1(2):100-109.
Publisher | Google Scholor - Smurygina L.V. (2022). Theory and methodology of track and field athletics (part 1 - theoretical foundations). Study guide, Tashkent “O” ZKITOBSAVDONASHRIYOTI” NMIU, 414.
Publisher | Google Scholor - Smurygina L.V. (2022). Theory and methodology of track and field athletics (part 2 - Running types). Study guide, Tashkent, “O” ZKITOBSAVDONASHRIYOTI” NMIU, 256.
Publisher | Google Scholor - Smurygina L.V., Sivodedov I.L. Ivanova-Tyurina V.V., Homidova O.K. (2022). Theory and methodology of track and field athletics (Training in the types of athletics). Study Guide Tashkent, “O” ZKITOBSAVDONASHRIYOTI” NMIU, 128.
Publisher | Google Scholor