Review Article
Thalassemia: Inherited Blood Disorder
1Sri Sharda Group of Institutions Lucknow, U.P., India
2DGPG College Kanpur U.P. India.
*Corresponding Author: D.K. Awasthi, Sri Sharda Group of Institutions Lucknow, U.P., India
Citation: Awasthi D. K, Dixit A. (2023). Thalassemia: Inherited Blood Disorder. Journal of BioMed Research and Reports, BioRes Scientia Publishers. 4(6):1-06. DOI: 10.59657/2837-4681.brs.24.086
Copyright: © 2024 D.K. Awasthi, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: May 01, 2024 | Accepted: May 16, 2024 | Published: May 23, 2024
Abstract
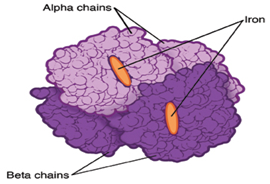
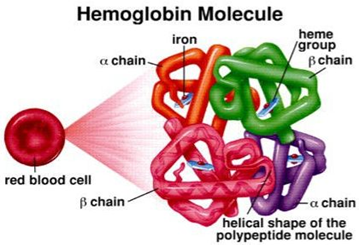
Thalassemia is the most common inherited blood condition in the world. This condition is caused by changes to the genes for hemoglobin. Hemoglobin is a protein in red blood cells that carries oxygen around the body. Changes affecting hemoglobin result in severe anemia. Thalassemia can affect people of any nationality and ethnicity. It is particularly common in people of Mediterranean ancestry and across a broad region extending through India, the Middle East, Asia and Latin America. Thalassemia is usually diagnosed within the first six months of life and can be fatal in early childhood without ongoing treatment. There are two different types of thalassemia: alpha (a) and beta (b). Alpha-thalassemia involves genetic changes in two genes (HBA1 and HBA2). Beta-thalassemia involves changes in one gene (HBB). Alpha-thalassemia is more common in countries in Africa, Asia and the Middle East. Beta-thalassemia is more common in Mediterranean countries.
Keywords: thalassemia; red blood cells; genes; anemia; beta; alpha
Introduction
Thalassemia is an inherited blood disorder in which the body makes an abnormal form of hemoglobin. Hemoglobin is the protein molecule in red blood cells that carries oxygen. The disorder results in excessive destruction of red blood cells, which leads to anemia. Anemia is a condition in which your body doesn’t have enough normal, healthy red blood cells. Thalassemia is inherited, meaning that at least one of your parents must be a carrier of the disorder. It’s caused by either a genetic mutation or a deletion of certain key gene fragments. Thalassemia minor is a less serious form of the disorder. There are two main forms of thalassemia that are more serious. In alpha thalassemia, at least one of the alpha globin genes has a mutation or abnormality. In beta thalassemia, the beta globin genes are affected. Each of these forms of thalassemia has different subtypes. The exact form you have will affect the severity of your symptoms and your outlook. The symptoms of thalassemia can vary. Some of the most common ones include:1. Bone deformities especially in the face2. Dark urine 3. Delayed growth and development4.excessive tiredness and fatigue 5. yellow or pale skin Thalassemia occurs when there’s an abnormality or mutation in one of the genes involved in hemoglobin production. You inherit this genetic abnormality from your parents. If only one of your parents is a carrier for thalassemia, you may develop a form of the disease known as thalassemia minor. If this occurs, you probably won’t have symptoms, but you’ll be a carrier. Some people with thalassemia minor do develop minor symptoms. If both of your parents are carriers of thalassemia, you have a greater chance of inheriting a more serious form of the disease.
There are three main types of thalassemia (and four subtypes)
1.beta thalassemia, which includes the subtypes major and intermedia,Beta thalassemia occurs when your body can’t produce beta globin. Two genes, one from each parent, are inherited to make beta globin. This type of thalassemia comes in two serious subtypes: thalassemia major (Cooley’s anemia) and thalassemia intermedia.
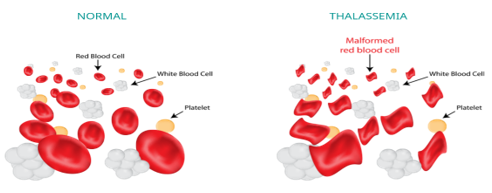
Figure 1
2.alpha thalassemia, which include the subtypes hemoglobin H and hydrops fetalis Alpha thalassemia occurs when the body can’t make alpha globin. In order to make alpha globin, you need to have four genes, two from each parent. This type of thalassemia also has two serious types: hemoglobin H disease and hydrops fetalis.
3.thalassemia minor Even if thalassemia minor doesn’t cause any noticeable symptoms, you can still be a carrier for the disease. This means that, if you have children, they could develop some form of the gene mutation.
Figure 2
Figure 3
Figure 4
Abnormally shaped red blood cells are a sign of thalassemia. For example, a severely enlarged spleen might suggest to your doctor that you have hemoglobin H disease.
Blood transfusion
- Bone Marrow transplant
- medications and supplements
possible surgery to remove the spleen or gallbladder
Your doctor may instruct you not to take vitamins or supplements containing iron. This is especially true if you need blood transfusions because people who receive them accumulate extra iron that the body can’t easily get rid of. Iron can build up in tissues, which can be potentially fatal. If you’re receiving a blood transfusion, you may also need chelation therapy. This generally involves receiving an injection of a chemical that binds with iron and other heavy metals. This helps remove extra iron from your body. Beta thalassemia occurs when your body can’t produce beta globin. Two genes, one from each parent, are inherited to make beta globin. This type of thalassemia comes in two serious subtypes: thalassemia major (Cooley’s anemia) and thalassemia intermedia.
Thalassemia major
Thalassemia major is the most severe form of beta thalassemia. It develops when beta globin genes are missing.
The symptoms of thalassemia major generally appear before a child’s second birthday. The severe anemia related to this condition can be life-threatening. Other signs and symptoms include:
- fussiness
- paleness
- frequent infections
- a poor appetite
- failure to thrive
- jaundice, which is a yellowing of the skin or the whites of the eyes
- enlarged organs
This form of thalassemia is usually so severe that it requires regular blood transfusions.
Thalassemia intermedia is a less severe form. It develops because of alterations in both beta globin genes. People with thalassemia intermedia don’t need blood transfusions.
Hemoglobin H develops as when a person is missing three alpha globin genes or experiences changes in these genes. This disease can lead to bone issues. The cheeks, forehead, and jaw may all overgrow.
Additionally, hemoglobin H disease can cause:
- jaundice
- an extremely enlarged spleen
- malnourishment
Hydrops fetalis is an extremely severe form of thalassemia that occurs before birth. Most babies with this condition are either stillborn or die shortly after being born. This condition develops when all four alpha globin genes are altered or missing. Thalassemia can quickly lead to anemia. This condition is marked by a lack of oxygen being transported to tissues and organs. Since red blood cells are responsible for delivering oxygen, a reduced number of these cells means you don’t have enough oxygen in the body either. Thalassemia is genetic in nature. To develop full thalassemia, both of your parents must be carriers of the disease. As a result, you will have two mutated genes. It’s also possible to become a carrier of thalassemia, where you only have one mutated gene and not two from both parents. Either one or both of your parents must have the condition or be a carrier of it. This means that you inherit one mutated gene from either one of your parents. It’s important to get tested if one of your parents or a relative has some form of the disease.
Children can start exhibiting symptoms of thalassemia during their first two years of life. Some of the most noticeable signs include:
- fatigue
- jaundice
- pale skin
- poor appetite
- slow growth
It’s important to diagnose thalassemia quickly in children. If you or your child’s other parent are carriers, you should have testing done early.
A low-fat, plant-based diet is the best choice for most people, including those with thalassemia. However, you may need to limit iron -rich foods if you already have high iron levels in your blood. Fish and meats are rich in iron, so you may need to limit these in your diet.
You may also consider avoiding fortified cereals, breads, and juices. They contain high iron levels, too.
Thalassemia can cause folic acid (folate) deficiencies. Naturally found in foods such as dark leafy greens and legumes, this B vitamin is essential for warding off the effects of high iron levels and protecting red blood cells.
There’s no one diet that can cure thalassemia, but making sure you eat the right foods can help. Be sure to discuss any dietary changes with your doctor ahead of time.
Since thalassemia is a genetic disorder, there’s no way to prevent it. However, there are ways you can manage the disease to help prevent complications.
In addition to ongoing medical care, this disorder protects themselves from infections by keeping up with the following vaccines:
- haemophilus influnza type b
- hepatitis
- meningococcal
- pneumococcal
In addition to a healthy diet, regular exercise can help manage your symptoms and lead to a more positive prognosis. Moderate-intensity workouts are usually recommended, since heavy exercise can make your symptoms worse.
Walking and bike riding are examples of moderate-intensity workouts. Swimming and yoga are other options, and they’re also good for your joints. The key is to find something you enjoy and keep moving.
Thalassemia is a serious illness that can lead to life-threatening complications when left untreated or undertreated. While it’s difficult to pinpoint an exact life expectancy, the general rule is that the more severe the condition, the quicker thalassemia can become fatal.
people with beta thalassemia — the most severe form — typically die by age 30. The shortened life span has to do with iron overload, which can eventually affect your organs.
Researchers are continuing to explore genetic testing as well as the possibility of gene therapy. The earlier thalassemia is detected, the sooner you can receive treatment. In the future,gene therapy could possibly reactivate hemoglobin and deactivate abnormal gene mutations in the body.
Thalassemia also brings up different concerns related to pregnancy. The disorder affects reproductive organ development. Because of this, women with thalassemia may encounter fertility difficulties.To ensure the health of both you and your baby, it’s important to plan ahead of time as much as possible. If you want to have a baby, discuss this with your doctor to make sure that you’re in the best health possible. Your iron levels will need to be carefully monitored. Preexisting issues with major organs are also considered.
Prenatal testing for thalassemia may be done at 11- and 16-weeks trusted source. This is done by taking fluid samples from either the placenta or the fetus, respectively. Pregnancy carries the following risk factors in women with thalassemia:
- a higher risk for infections
- gestational diabetes
- heart problems
- hypothyroidism, or low thyroid
- increased number of blood transfusions
- low bone density
limit to the number of blood transfusions you can receive. However, they may become less effective over time as your body develops antibodies against transfused blood.
Immunosuppressant drugs: These medications suppress the damage that immune cells are doing to your bone marrow. This allows the bone marrow to recover and create more blood cells. Stem cell transplants: These can help rebuild the bone marrow to the point where it creates enough blood cells.
Thalassemia fever
Salmonella typhi, a hazardous pathogen, causes Thalassemia fever. The bacteria that cause salmonellosis, another deadly intestinal infection, are related to Salmonella typhi, but they are not the same. The majority of persons in wealthy countries contract Thalassemia bacteria while travelling. Once infected, they can transfer the disease to others via the fecal-oral route. This means that infected persons pass Salmonella typhi in their stools and occasionally in their pee. You can get Thalassemia fever if you eat food that has been touched by someone who has the disease and hasn't cleaned their hands thoroughly after using the restroom. The majority of persons infected with Thalassemia fever in developing nations get it through drinking polluted water. The bacterium can also be transferred by contaminated food or direct contact with an affected person.
Conclusion
The severity of thalassemia depends on how many genes are mutated One mutated gene: The person has no symptoms. A healthy person who has a child with symptoms of thalassemia is a carrier. This type is known as alpha thalassemia minima. Two mutated genes: The person has mild anemia. It is known as alpha thalassemia minor. Three mutated genes: The person has hemoglobin H disease, a type of chronic anemia. They will need regular blood transfusions throughout their life. Four mutated genes: Alpha thalassemia major is the most severe form of alpha thalassemia. It is known to cause hydrops fetalis, a serious condition in which fluid accumulates in parts of a fetus’s body. A fetus with four mutated genes cannot produce normal hemoglobin and is unlikely to survive, even with blood transfusions. People with thalassemia may have to avoid some foods, such as spinach or iron -enriched cereals, to prevent excessive iron buildup. The centers for Disease control and prevention urge people with thalassemia to keep their vaccinations up to date to prevent illness.
References
- He LN, Chen W, Yang Y, Xie YJ, Xiong ZY, et al. (2019). Elevated Prevalence of Abnormal Glucose Metabolism and Other Endocrine Disorders in Patients with β-Thalassemia Major: A Meta-Analysis. Biomed Res Int., 6573497.
Publisher | Google Scholor - Roddy E, Doherty M. (2010). Epidemiology of gout. Arthritis Res Ther; 12:223.
Publisher | Google Scholor - Zhu Y, Pandya BJ, Choi HK. (2011). Prevalence of gout and hyperuricemia in the US general population: the National Health and Nutrition Examination Survey 2007-2008. Arthritis Rheum, 63:3136-3141.
Publisher | Google Scholor - Mikuls TR, Farrar JT, Bilker WB, et al. (2005). Gout epidemiology: results from the UK general practice research database, 1990–1999. Ann Rheum Dis, 64:267-272.
Publisher | Google Scholor - Wallace KL, Riedel AA, Joseph-Ridge N, Wortmann R. (2004). Increasing prevalence of gout and hyperuricemia over 10 years among older adults in a managed care population. J Rheumatol, 31:1582-1587.
Publisher | Google Scholor - Choi HK, Curhan G. (2005). Gout: epidemiology and lifestyle choices. Curr Opin Rheumatol, 17:341-345.
Publisher | Google Scholor - Emmerson BT. (1996). The management of gout. N Engl J Med, 334:445-451.
Publisher | Google Scholor - Choi HK, Mount DB, Reginato AM; (2005). American College of Physicians; American Physiological Society. Pathogenesis of gout. Ann Intern Med, 143:499-516.
Publisher | Google Scholor - Martinon F, Glimcher LH. (2006). Gout: new insights into an old disease. J Clin Invest, 116:2073-2075.
Publisher | Google Scholor - Pascual E, Jovani V. (2005). Synovial fluid analysis. Best Pract Res Clin Rheumatol, 19:371-386.
Publisher | Google Scholor - Choi MH, MacKenzie JD, Dalinka MK. Imaging features of crystal-induced arthropathy. Rheum Dis Clin North Am, 32:427-446.
Publisher | Google Scholor - Bongartz T, Glazebrook KN, Kavros SJ, et al. Dual-energy CT for the diagnosis of gout: an accuracy and diagnostic yield study. Ann Rheum Dis, 74:1072-1077.
Publisher | Google Scholor - Frediani B, Filippou G, Falsetti P, et al. (2005). Diagnosis of calcium pyrophosphate dihydrate crystal deposition disease: ultrasonographic criteria proposed. Ann Rheum Dis, 64:638-640.
Publisher | Google Scholor - Thiele R, Schlesinger N. (2007). Diagnosis of gout by ultrasound. Rheumatology, 46:1116-1121.
Publisher | Google Scholor - Khanna D, Fitzgerald JD, Khanna PP, et al. (2005). 2012 American College of Rheumatology guidelines for management of gout. Part 1: systematic nonpharmacologic and pharmacologic therapeutic approaches to hyperuricemia. Arthritis Care Res (Hoboken) 64:1431-1446.
Publisher | Google Scholor - Khanna D, Khanna PP, Fitzgerald JD, et al. (2005). American College of Rheumatology guidelines for management of gout. Part 2: therapy and antiinflammatory prophylaxis of acute gouty arthritis. Arthritis Care Res (Hoboken), 64:1447.
Publisher | Google Scholor - Becker MA, Schumacher HR Jr, Wortmann RL, et al. (2005). Febuxostat compared with allopurinol in patients with hyperuricemia and gout. N Engl J Med, 353:2450-2461.
Publisher | Google Scholor - Borstad GC, Bryant LR, Abel MP, et al. (2004). Colchicine for prophylaxis of acute flares when initiating allopurinol for chronic gouty arthritis. J Rheumatol, 31:2429-2432.
Publisher | Google Scholor - Faruque LI, Ehteshami-Afshar A, Wiebe N, Tjosvold L, Homik J, Tonelli M. (2013). A systematic review and meta-analysis on the safety and efficacy of febuxostat versus allopurinol in chronic gout. Semin Arthritis Rheum, 43:367-375.
Publisher | Google Scholor - Schlesinger N. (2004). Management of acute and chronic gouty arthritis: present state-of-the-art. Drugs, 64:2399-2416.
Publisher | Google Scholor - Becker MA, Schumacher HR Jr, Wortmann RL, et al. (2005). Febuxostat, a novel nonpurine selective inhibitor of xanthine oxidase: a twenty-eight–day, multicenter, phase II, randomized, double-blind, placebo-controlled, dose-response clinical trial examining safety and efficacy in patients with gout. Arthritis Rheum, 52:916-923.
Publisher | Google Scholor - Tayar JH, Lopez-Olivo MA, Suarez-Almazor ME. (2005). Febuxostat for treating chronic gout. Cochrane Database Syst Rev, 11:CD008653.
Publisher | Google Scholor - Schumacher HR Jr, Becker MA, Lloyd E, MacDonald PA, et al. (2009). Febuxostat in the treatment of gout: 5-yr findings for the FOCUS efficacy and safety study. Rheumatology, 48:188-194.
Publisher | Google Scholor - Choi HK, Atkinson K, Karlson EW, et al. (2004). Alcohol intake and risk of incident gout in men: a prospective study. Lancet, 363:1277-1281.
Publisher | Google Scholor - Choi HK, Atkinson K, Karlson EW, et al. (2004). Purine-rich foods, dairy and protein intake, and the risk of gout in men. N Engl J Med, 350:1093-1103.
Publisher | Google Scholor - Lee SJ, Terkeltaub RA, Kavanaugh A. (2006). Recent developments in diet and gout. Curr Opin Rheumatol, 18:193-198.
Publisher | Google Scholor - De Souza AW, Fernandes V, Ferrari AJ. (2005). Female gout: clinical and laboratory features. J Rheumatol, 32:2186-2188.
Publisher | Google Scholor - Stamp L, Searle M, O'Donnell J, Chapman P. (2005). Gout in solid organ transplantation: a challenging clinical problem. Drugs, 65:2593-2611.
Publisher | Google Scholor - Wilkins E, Dieppe P, Maddison P, Evison G. (1983). Osteoarthritis and articular chondrocalcinosis in the elderly. Ann Rheum Dis, 42:280-284.
Publisher | Google Scholor - Neame RL, Carr AJ, Muir K, Doherty M. (2003). UK community prevalence of knee chondrocalcinosis: evidence that correlation with osteoarthritis is through a shared association with osteophyte. Ann Rheum Dis, 62:513-518.
Publisher | Google Scholor - Tenenbaum J, Muniz O, Schumacher HR, et al. (1981). Comparison of phosphohydrolase activities from articular cartilage in calcium pyrophosphate deposition disease and primary osteoarthritis. Arthritis Rheum, 24:492-500.
Publisher | Google Scholor - Johnson K, Pritzker K, Goding J, Terkeltaub R. (2001). The nucleoside triphosphate pyrophosphohydrolase isozyme PC-1 directly promotes cartilage calcification through chondrocyte apoptosis and increased calcium precipitation by mineralizing vesicles. J Rheumatol, 28:2681-2691.
Publisher | Google Scholor - Dieppe PA, Alexander GJ, Jones HE, et al. (1982). Pyrophosphate arthropathy: a clinical and radiological study of 105 cases. Ann Rheum Dis, 41:371-376.
Publisher | Google Scholor - Adamson TC 3rd, Resnik CS, Guerra J Jr, et al. (1983). Hand and wrist arthropathies of hemochromatosis and calcium pyrophosphate deposition disease: distinct radiographic features. Radiology, 147:377-381.
Publisher | Google Scholor - Alvarellos A, Spilberg I. (1986). Colchicine prophylaxis in pseudogout. J Rheumatol, 13:804-805.
Publisher | Google Scholor - Doherty M, Dieppe P, Watt I. (1993). Pyrophosphate arthropathy: a prospective study. Br J Rheumatol, 32:189-196.
Publisher | Google Scholor