Research Article
Surgical Treatment in Squamous Cell Lip Carcinoma
1Faculty of Medicine and Pharmacy “Dunărea de jos” Galati, Romania.
2University of Medicine and Pharmacy “Gr. T. Popa” Iasi, Romania.
3Emergency County Hospital of Braila, Romania.
*Corresponding Author: Cristina Stanescu, Faculty of Medicine and Pharmacy “Dunărea de jos” Galati, Romania.
Citation: Stanescu C., Tamas C., Georgiana D. Stanescu. (2023). Surgical Treatment in Squamous Cell Lip Carcinoma. Journal of BioMed Research and Reports, BRS Publishers. 2(3); DOI: 10.59657/2837-4681.brs.23.024
Copyright: © 2023 Cristina Stanescu, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: April 24, 2023 | Accepted: May 10, 2023 | Published: May 16, 2023
Abstract
Introduction: Lip cancer is the most frequent malignant tumours of the oral cavity. Lip carcinoma could appear on pre-cancerous lesions (such as radio-dermitis, chronic cheilitis, xeroderma pigmentosum etc.) and is related with other risk factors like smoking, chronic alcohol consumption, immunosuppression, HPV infection etc.
Materials and Methods: This study was conducted on a representative sample made of 164 patients diagnosed with squamous cell carcinoma and 62 patients with squamous cell lip carcinoma from 2010 to 2018 at the Plastic Surgery Compartment at the Emergency County Hospital of Braila. The incidence of squamous cell lip carcinoma increases in the last years from 20% in 2010 to 26% in 2018. This study analyses clinical characteristics and histopathological types of lip carcinoma, frequency of the squamous cell lip carcinoma, the relation between the resection margins and tumour size, types of local flaps used in the reconstruction of consecutive defects, local evolution and possible metastatic spread to the lymph node of the neck. Squamous cell lip carcinoma was located to the lower lip at 40 patients, to the commissure at 14 patients and to the upper lip at 8 patients. The youngest patient with squamous cell lip carcinoma was 22 years old.
Results and Discussion: Lesions smaller than 1 cm were more frequent (62%) compare to the lesions which involved more than half of the lip (8%). For small tumours, under 1 cm, the resection margins were made at 4 mm, for tumours with sizes between 1-2 cm the tumour resection was performed 6 mm from the tumour margins and for large tumours, more than 2 cm, the resection margins increase to 1 cm. Early-stage tumours were treated by direct suture with a very good prognosis. For advanced lesions we used a variety of flaps for lip reconstruction: Gillies’s flap, Abbé flap, Karapandzic flap, McGregor flap, Estlander flap, nasolabial flaps (Fujimori and Ombredane) etc. Two patients return for commissuroplasty. We used a Converse flap and a Zisser flap.
Conclusions: The successful reconstruction depends on preoperative planning according to the tumour site and size. Lymph node metastases significantly reduce long term survival. For a plastic surgeon the aesthetic appearance has the same importance like the functional results.
Keywords: squamous cell lip carcinoma; incidence; risk factors; resection margins; surgical reconstruction; survival rate
Introduction
Lip cancer is the most frequent malignant tumors of the oral cavity [1]. The squamous cell carcinoma is the most frequent tumor in the lower lip, on the red part, whereas the basal cell carcinoma usually involves the white upper lip. The lesion caused by squamous cell lip carcinoma is often asimptomatic and the clinical appearance is highly variable from a reddish skin plaque to an ulcerated lesion with hard raised edges. Squamous cell lip carcinoma is slow-growing, but occasionaly, these cancers can have a behaviour more aggressively, spreading to regional lymph nodes at a relatively early stage [2]. The incidence in rural patients is higher compare to urban patients because of their outdoors activities. Long term exposure to sun radiation is directly involved in the pathogeny of facial cutaneous carcinoma [3]. Lip carcinoma could appear on pre-cancerous lesions, such as radiodermitis, chronic cheilitis, xeroderma pigmentosum etc. Most skin cancers are not caused by an inherited faulty gene that can be passed on to the next generation, but members of families have the same skin type, wich may increase their risk of developing a skin cancer. Lip carcinoma is related with other risk factors like smoching, chronic alcohol consumption, immunosuppression, HPV infection etc [4]. Another possible risk factors are represented by over exposure to some chemicals such as coal tar, soot, pitch, asphalt, petroleum derivatives, paraffin waxes, arsenic etc [5]. Excision is undertaken with 4 mm margins for low risk and more than 6 mm for high-risk lesions [6]. There is no randomised controlled study to show that Mohs technique is superior to conventional surgery [7]. Regarding the choice for lip reconstruction after wide excision, several issues should be considered including contour, texture, colour, aesthetic units, donor site and the wishes of the patients. Early stage tumors treated by direct suture have a very good prognosis. For advanced lesions a variety of flaps could be used, according to the preoperative plan [8]. The percentage of patients with lymph node metastases increases considerably in advanced stage tumor. Lymph node metastases significantly reduce long term survival [9].
Materials and Methods
This study was conducted on a representative sample made of 164 patients diagnosed with squamous cell carcinoma and 62 patients with squamous cell lip carcinoma from 2010 to 2018 in the Plastic Surgery Compartment at the Emergency County Hospital of Braila. This study analises clinical characteristics and histopathological types of lip carcinoma, frequency, the relation between the resection margins and tumor size, types of local flaps used in the reconstruction of consecutive defects, functional results, local evolution and possible metastatic spread to the lymph node of the neck. We quantified the characteristic parameters represented by age, sex, residence, types of carcinomas, anatomical areas. The incidence in rural patients is high compare to the urban patients. The incidence in male patients is higher (58%) than female (42%). Squamous cell lip carcinoma was located to the lower lip at 40 patients (64,5%), to the commissure at 14 patients (22,5%) andto the upper lip at 8 patients (13%). The youngest patient with squamous cell lip carcinoma was 22 years old. Eight patients developed two types of cutaneous carcinoma at the same time in different areas.
Lesions smaller than 1 cm were more frequent (62%), compare to the lesions which involved more than half of the lip (8%). 96% of squamous cell lip carcinoma involve the vermillion. The successful of reconstruction depends on preoperative planning according to the tumor site and size. For small tumors, under 1 cm, the resection margins were made at 4 mm, for tumors with diameter between 1-2 cm the tumor resection is performed 6 mm from the tumor margins and for large tumors, more than 2 cm, the resection margins increase to 1 cm. Numerous techniques have been developed for lip reconstruction. The choice depends on the position of tumor and its extension level. Early stage tumors was treated by direct suture after V-shaped excision, with a very good prognosis. For advanced lesions we used a variety of flaps for lip reconstruction: Gillies’s flap, Mc Gregor flap, Karapandzic flap, Abbé flap, Estlander flap, nasolabial flap (Fujimori and Ombredane) etc. Two patients return for comissuroplasty. We used a Converse flap and a Zisser flap. Suture must consider all anatomical planes, using separate absorbable threads for mucosa and muscular plane and nonabsorbable threads for skin. Lymph node metastases significantly reduce long term survival.
Results and Discussion
The distribution of patients with squamous cell carcinoma has revealed that the highest incidence of this type of cancer is recorded in person aged over 50 years. The incidence of squamous cell lip carcinoma increases in the last years from 20% in 2010 to 26% in 2018. Local flaps were the first option for the most patients with large tumors which requiring postoperative reconstructions. The reconstruction of postoperative defects depends on the position of the lesion and its extension level. The patients with early stage tumors recovered within 3 weeks after surgery with good long-term aesthetic and functional results.
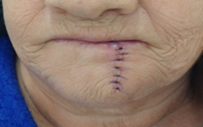
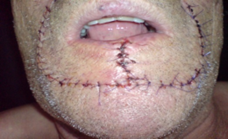
Figure 1: Postoperative appearance after three weeks.
Smaller lesions with diameter under 1 cm were most frequent (62%). In a few cases (8%) the lesions involved more than two-thirds of the lip. In 78% of cases a direct suture was performed, after V-shaped excision (Figure 1,2). In 14% of cases the lip reconstruction required the use of a single flap (figure 3,4). For near total lip defects (8% of cases) it was necessary to combine several flaps.
Figure 2: 74-year-old woman with lower lip carcinoma.
Figure 3: Direct suture after V-shaped excision.
Figure 4: 74-year-old woman with lower lip carcinoma.
Figure 5: Mc Gregor unilateral flap. Postoperative appearance after four years.
The nasolabial flap is widely used to cover facial defects, including the reconstruction of post excisional defects on the entire lower lips (figure 5,6). These flaps contained innervated muscle, has a good blood supply and motor function. The main disadvantage is the loss of saliva. The cross-lip operation (Abbé flap) has an important role in improving the appearance of the lips by reducing tension and restoring lip balance, having the advantage of early sectioning of the pedicle and great flexibility, this flap can be used in combination with other flaps (figure 7,8,9).
Figure 6: Extensive lower lip carcinoma in a 76-year-old man.
Figure 7: Bilateral nasolabial flap combined with submental advanced flap.
Figure 8: Extensive lower lip carcinoma in a 52-year-old man.
Figure 9: Gillies fan flap technique combined with the Abbé flap.
Figure 10: Postoperative appearance after five years.
For tumors located in the central lower lip the Karapandzic flap, consisting in perioral advancement, remains a good option (figure 10,11). The reconstruction of the commisure could be performed using a Brusari flap (figure 12, 13, 14). Numerous techniques have been developed for lip reconstruction, the choice depend on the position of tumor and its extension level. Early stage tumors treated by direct suture have a good prognostic, compare with advanced lesions who need for reconstruction complexe technique under general anesthesia altering the appearence and the oral functionality.
Figure 11: Central lower lip carcinoma in a 55-year-old man.
Figure 12: Karapandzic flap for central lip reconstruction.
Figure 13: Invasive carcinoma at the level of the commissure in a 67-year-old patient.
Figure 13: Intraoperative aspect.
Figure 14: Bursary flap for commissure reconstruction.
At the time of diagnoses, 6 cases presented locoregional metastases. Recurrences after one year were recorded in 0,6 %. After 2 years the percentage increases to 1.8%. The survival rate at 3 years was 99%. Lymph node metastases reduce survival rate at 48%. Lymph node metastases appear to be more frequent in undifferentiated carcinoma than well different elated tumours [10]. Recurring tumours and lymph node metastases is associated with a poor prognosis [11]. The prognosis is worse for tumours located at the commissure than the tumours from the middle part of the lip [12].
Conclusion
The interventions using local flaps with similar colour and texture provide the possibility of restoring aesthetic appearance with good functional results. The reconstruction after tumor excision with local flaps is a real challenge from the perspective of multiple surgical techniques using to restore all the structures in one session. The defect reconstruction for most extensive tumors, using local flaps, provides the possibility of restoring motor and sensory oral function. Postoperative wounds heal in maximun 3 weeks, and complication like necrosis, infection and hematoma are very rare. The patients with advanced tumors after wide excision and local plasty presented complication related to postoperative incontinence and incompetence, including vocalization, drooling and chewing disorder. These patients need kinetotherapy to improve lips mobility and flexibility and just a few patients return for comissuroplasty [13].
The incomplete excision, young patients, presence of other comorbidities and local reccurences are associated with poor prognosis. Increasing the resection margins according to the tumor size, decreases the risk of reccurence. Radiotherapy is indicated after the tumor resection. Lymph node neck metastases significantly reduces long term survival [14]. The diagnosis of these tumors is facilitated by a direct view of lesions and the local invasion should be avoided. For a plastic surgeon the aesthetic appearance has the same importance like the functional results.
Conflicts of interest statement
The authors declare no conflicts of interests.
References
- Leiter U, Eigentler T, Garbe C. (2014). Epidemiology of skin cancer. Adv Exp Med Biol., 810:120-40.
Publisher | Google Scholor - Vartanian JG, Carvalho AL, Araujo Filho, et al. (2004). Predictive factors and distribution of lymph node metastasis in lip cancer patients and their implications on the treatment of the neck. Oral Oncology., 40:223-227.
Publisher | Google Scholor - Lim JL, Satem RS. (2005). High levels of ultraviolet B exposure increase the risk of non-melanoma skin cancer in psoralen and ultraviolet A-treated patients. J Invest Dermatol., 124(3):505-513.
Publisher | Google Scholor - Moore SR, Johnson NW, Pierce AM, et al. (1999). The epidemiology of lip cancer: a review of global incidence and etiology. Oral Dis., 5:185-195.
Publisher | Google Scholor - Fabbrocini G, Triass M, Mauriello MC, Annunziata MC, De Vita V. et al (2010). Epidemiology of skin cancer: role of some environmental factors. Cancers, 2(4):1980-1989.
Publisher | Google Scholor - Papadopoulos O, Konofaos P, Tsantoulas Z, et al. (2007). Lip defects due to tumor excision: Apropos of 899 cases. Oral Oncology, 43:204-212.
Publisher | Google Scholor - Baker SR. (1990). Current management of cancer of the lip. Oncology, 4:107-120.
Publisher | Google Scholor - Karapandzic M. (1974). Reconstruction of lip defects by local arterial flaps. Br J Plast Surg. 27:93-97.
Publisher | Google Scholor - Gooris PJJ, Vermey A, Visscher JGAM, et al. (2002). Supraomohyoid neck dissection in the management of cervical lymph node metastases of squamous cell carcinoma of the lower lip. Head Neck, 24:678-676
Publisher | Google Scholor - Vukadinovic M, Jezdic Z, Petrovic M, et al. (2007). Surgical management of squamous cell carcinoma of the lip: analysis of a 10-year experience in 223 patients. J Oral Maxillofac Surg, 65:675-679.
Publisher | Google Scholor - Bucur A, Stefanescu L. (2004). Management of patients with squamous cell carcinoma of the lower lip and N0-neck. J Craniomaxillofac Surg, 32:16-21.
Publisher | Google Scholor - Visscher JGAM, Elsaker K, Grond AJK, et al. (1998). Surgical treatment of squamous cell carcinoma of the lower lip: evaluation of long-term results and prognostic factors – A retrospective analysis of 184 patients. J Oral Maxillofac Surg, 56:814-820.
Publisher | Google Scholor - Zitsch RP. (1993). Carcinoma of the lip. Otolaryngol Clin North Am., 26:265-277.
Publisher | Google Scholor - Zitsch RP, Lee BW, Smith RB. (1999). Cervical lymph node metastases and squamous cell carcinoma of the lip. Head Neck, 21:447-453.
Publisher | Google Scholor