Review Article
Surgical Site Infections in Abdominal Surgeries and Role of Microorganisms-A Review Article
- Anilreddy Cherukula *
- S.N. Jajo0
- Bhushan Jajoo
- Garima Saxena
Department of General Surgery, Datta Meghe Institute of Medical Sciences, Wardha, India.
*Corresponding Author: Anilreddy Cherukula, Department of General Surgery, Datta Meghe Institute of Medical Sciences, Wardha, India.
Citation: Cherukula A. Jajoo S.N., Jajoo B, Saxena G. (2023). Surgical Site Infections in Abdominal Surgeries and Role of Microorganisms -A Review Article. Clinical Case Reports and Studies, BioRes Scientia Publishers. 5(3):1-6. DOI: 10.59657/2837-2565.brs.24.112
Copyright: © 2024 Anilreddy Cherukula, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: January 17, 2024 | Accepted: February 23, 2024 | Published: March 04, 2024
Abstract
Background: World Health Organization published a document regarding the increasing instances of the surgical site infections and it highlights the growing and expanding number of instances which are occurring throughout the world.
Summary: The surgical site infections are the infections are which are destined to cause after the surgical procedure which involves an incisional cut. However, the percentage of the occurrence of the SSI stands around 1 to 4 percentage of the cases, in case of abdominal surgeries up to 25 percentage of all the SSI cases occurrence in the abdominal surgery patient.
Conclusion: The infections are preventable in nature in the majority of the patients. The high-risk category patients indent8fied using various preexisting comorbidity and duration of the surgery can have impact on the patient’s clinical outcome.
Keywords: ssi; abdominal surgery; prophylactic; antibiotics; preopertive shower; diabetes mellitus
Introduction
Surgical station contamination (SSI) is outlined by the Centers for Disease Control and Prevention as a wound contamination that happens inside 30 days of an active process or within a old age if an insert is abandoned working and the contamination is thought expected subordinate to medical procedure. It is individual of ultimate common fitness care associated contaminations, happening following 1%–3% of all surgical processes. The rates of SSI are much greater with intestinal medical procedure than accompanying added types of medical procedure, accompanying various potential studies displaying an occurrence to every divide into four equal parts contingent upon the level of adulteration [1–3]. Such contaminations lengthen bed stay for a median of seven days. Potential beginnings of infection are the patient (particularly adulteration by digestive lot of microorganisms), hospital surroundings, cooking, different inmates, stick, infected surgical means, dressings, and even drugs and injections. Surgical location contamination is able to be averted and is guide high depression and death. In addition to the trenchant affect the patient’s course of situation, it is associated with extended time of nursing home stay and larger costs. Numerous risk determinants may enhance the happening of SSI, accompanying ultimate acknowledged factors being these organized in the SSI risk index, containing wound categorization, American Society of Anesthesiologists (ASA) score and event of the operation. The basic goals concerning this study search out name the occurrence and risk determinants guide SSI in victims meeting with intestinal surgery [4–6]. The subordinate aims search out study the microbiological pattern of SSI in our community and their medicine sensitivity, and to study the result of SSI on examination distance of stay.
Methodology
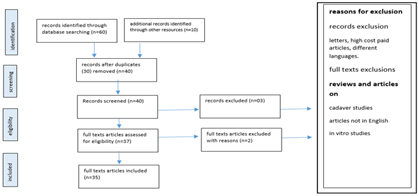
Figure 1: Study Selection process using the preferred reporting items for systematic Reviews and Meta analyses (PRISMA) guidelines
Surgical site infections
As the name suggests, these are the infections happening post-surgery in affected part or surrounding it. Any invasive surgery involves taring and incision in the skin which is the natural hindrance to the external pathogenic invasion. The skin is the largest organ and provides a protective coverage to all the internal organs and tissues [7–9]. A surgical procedure involves incision in skin layers of various degrees. So, there is always a potential to cause in the infection in that site. It can be limited to the site of the incision or it can spread to the other parts for example implanted material or the organ which was operated for any anomaly. It is one of the infections which comes under the ambit of the healthcare associated infections. The general occurrence of the surgical site infections (SSI) ranges from 1 to 3 percentages of all the surgical procedures but the severity various according to the patient’s condition. According to the severity and site if the infections there are three types of SSI categorized as follows. The first is the superficial incisional SSI in which the infection is only limited to the part of the skin where the incision was made to operate. This is visibly seen and observed through naked eye. The second is the deep incisional SSI in which the infection site is under the skin where the incision was made. Generally, it is not seen with the help of naked eye but if the wound is open, the health care professional can see the disintegrating tissues and pus formed in that area. The third is the space or organ SSI in which the organ or space surrounding a surgical area is affected and can be observed using the procedure for extracting the pus formed [10–12].
The visibility of the infection in the incisional SSI is the prime sign and symptoms but is not limited to it. SSI can effectuate redness, prolonged healing of the wound, fever and tenderness associated with the surgery, swelling at the site of the incisions and so on. In case of the Superficial incisional SSI and deep incisional SSI the pus formation can be detected and the culture can be grown to check the bacteria. In case of space or organ SSI, the drain can extract the pus and it can be grown in culture to identify the pathogen. X ray examination and drain procedure can reveal the abscess inside the patient’s body. The infection is mainly caused by the pathogenic invasion of the mound. The pathogens which mainly includes streptococcus, staphylococcus and pseudomonas are of bacterial origin. These pathogens can enter through wounds which are cut open via infected air, the pathogens which already exists in the body and so on. It can pass on through the health care professional as well as through infected surgical instrument which may not be sterilized [13–15]. The severity of the risk of the SSI also depends upon the wounds. There are clean wounds, contaminated wound and dirty wound which according to their nature tend to increase the severity of the SSI. There are several factors which can have adverse impact on the patients with respect to SSI. These risk factors include having the surgical procedure extending more than two hours, American Society of Anesthesiologists (ASA) score, comorbidity or underlying medical illnesses, obesity, history of smoking, diabetes and so on. These are the risk factors which needs to be watched out for to decrease the risk of the SSI.
Surgical site infections in abdominal surgeries
Surgeries involved cutting open a part of the body so as to fix things which were not working properly at the first place. Abdominal surgeries involved opening of the abdomen which is also known as laparotomy. Abdominal surgeries can deal with various organs like stomach, kidney, liver and so on. The surgical site infection (SSI) is defined as the infection in the wounds of the surgery within 30 days of the surgery. If any material is implanted in the patient, then the duration extended up to a year. IT is regarded as the common happening post surgeries [16–18]. Up to every 3 out of 100 operated subjects faces this issue. In case of abdominal surgeries, the rate is as high as up to every one of the four patients operated for abdominal ailments. Among all the other surgeries, surgical site infections in abdominal surgeries are most common and widely reported. Although they are preventable but can cause a greater degree of the damage to the patient as it has high morbidity rate as well as case fatality rate. The surgical procedure itself thrown in jeopardy and the patients stay at the health acre facility may prolong along with increase in cost of the health care services.
A study was done to assess the risk factors associated with the SSI especially in abdominal surgery and incidences among 337 patients which were enrolled in the study conducted in Saudi Arabia. Patients were observed and monitored for 30 days after their surgical procedure is done. Among the 193 females and 144 males studied, the mean age was 43.6 years. 4 patients obtained fatal clinical outcome before the completion of the 30 days period and rest completed the follow up. Most of the 337 patients that is 239 patients had ASA score less than 3. Most of the patient were having Laparoscopic cholecystectomy in which the proportion of the SSI was low as compared to the laparotomy in which the overall figure was low but the occurrence of the SSI was high. Several risk factors were identified for the occurrence of the SSI. In one finding, open laparotomy was found to be increasing the risk of SSI 6.5 times. Patients having operating procedure greater than 350 minutes, they were most likely to extend the hospital stay by a week. Microbiological examination of the bacterial culture is also important in determining the type of culprit pathogen. 52 percentage were found to be Escherichia coli followed by gram positive. Only 23 percentage of the bacteria found were sensitive or responsive to the antibiotics which are given to the patient prior to the operating procedure. Finally, study concludes that around 16 percentage of the patients develop SSI which when converted to figures stood at 55. The study concluded that antibiotic prophylactic course should be designed according to the commonly identified cultures from the pus samples of the SSI which can be beneficial to prevent the infection at first place [19–21].
Generally, the skin of the abdominal region is closed by the sutures which are subcuticular or the way of stapling. Various randomized controlled trials and meta-analyses shown the efficacy of the subcuticular sutures than the stapling ones. The subcuticular sutures are the intradermal stitches which are placed below the upper layer of the skin. These are stitches with the absorbable material filament which helps to seal and reconnect skin tissues. Where a certain study has shown no to low inflammatory response from the surgical stapler usage. It seals and is used to the reconnect the various organs which are operated for any medical anomaly [22–24]. There contradictory studies and hence larger cohort studies are needed in order to establish the correlation. But is certain that suture choices can influence the chances of the patient’s clinical outcome with respect to the surgical site infection. Wound splitting open and dehiscence along with other complications are result of the improper closure of the abdominal wall and subcuticular layer. Some common sutures used are polyglactin, pds, polypropylene, pga, polyglyconate, nylon, triclosan-coated polyglactin, triclosan-coated polydioxanone, steel, plg and ethibond. Appropriate clinical intervention can be initiated in order to preempt the spread of the bacterial clout.
The patient’s category highly influences the SSI outcome post-surgery. Especially patients with diabetes mellitus are on greater verge of catching the surgical site infections. Diabetes mellitus extends the duration of the healing due to high blood glucose levels. More than half a billion people are suffering from active diabetes at various stages. In addition any kind of immunosuppressive stage in life whether it be due to the increasing age and the cause is natural or due to any comorbidity then it can prove facilitating factor for the SSI to proliferate [25–27].
In a study done in the Iranian health care facility on more than 800 patients have insightful conclusions to offer. All the patients were followed 30 days post operation and questionnaire was served.
Among added determinants that delay wound curative or increase the contamination rate are really high, that increases the examination contamination rate 5-fold, and the use of steroids, that delays wound curative and increases the contamination rate by 9 allotment points from 7% to 16%. Aseptic surgical methods are demanded to decrease the contamination rate, though not to nothing. However, the presidency of protective medicines 30 to 60 record before incision, decreases the occurrence of SSI. Obviously, detached contaminations increase SSI. Other donating determinants are the type of section and subordinate contaminations. The object concerning this study search out determine SSI, and the occurrence of the determinants donating to aforementioned contaminations. Among added determinants that delay wound curative or increase the contamination rate are really high, that increases the examination contamination rate 5-fold, and the use of steroids, that delays wound curative and increases the contamination rate by 9 allotment points from 7% to 16%. Aseptic surgical methods are demanded to decrease the contamination rate, though not to nothing. However, the presidency of protective medicines 30 to 60 record before incision, decreases the occurrence of SSI. Obviously, detached contaminations increase SSI. Other donating determinants are the type of section and subordinate contaminations. The object concerning this study search out determine SSI, and the occurrence of the determinants donating to aforementioned contaminations [28–30].
Preventive clinical practices
Various practices prior to the operation can be undertaken in order to avoid the infection in the surgical place. Patients must be cleaned through preoperative shower. This shower contains antiseptic agents which presents any kind of septic in future. Although through washing of the body is necessary and must be the part of the standard operating procedure. As it is seen that it is not uniform across all the surgical facilities around the world leaving the patient in jeopardy. It is advisable that first shower should be performed two days prior to the surgery and second shower be one day prior to the surgery and third one on the day of the surgery. One study pointed out that the use of soap for the bathing procedure is of less efficient than use of chlorohexidine which can reduce the risk of SSI. In fact, there was a nine-fold decrease in the occurrence of the SSI. Another study done on 700 patients which undergone preoperative shower which is antiseptic nature shows remarkable decrease in the bacterial count on their body subsequently decreasing the chance of obtaining SSI at the first place. Patient adherence is another key factor in success of the procedure. Pre-operative shower before surgery has been found to be decreasing the concentration of the gram positive and gram negative bacteria on the patients reducing the exposure of the wound [31–33].
Administration of prophylactic medicine such as antibiotics would also decreases the chance of developing the SSI. Studies have shown the combined impact of the preoperative shower and administration of the prophylactic regime can have preventive impact with respect to the surgical site infection. Like the usage of the preoperative prophylactics, there also the need of the post-operative medicine which are antibiotics and are given after the surgery within one day. But it also related to the antibiotic resistance which can complicate the situation. The post-operative antibiotics must be administered in case where the need arises. Patients who are high risk and have various underlying medical illness and have age more than 60 years are the risk category of the patients where it is necessitated. It must be left with the local health care professional who can better assess the situation according to the clinical history of the patient [34,35].
| Author | Year | Study type | Conclusion |
| David Muchuweti & Kent UG Jonsson | 2013 | Original Article | Several risk factors for developing SSI has been identifies which includes comorbidity, diabetes, delayed use of prophylactics etc [35]. |
| Utsumi et al | 2022 | Research Article | High risk patients are more prone to the superficial incisional SSI[30]. |
| Tomsic et al | 2020 | Research Article | Administration of prophylactic medicine such as antibiotics would also decreases the chance of developing the SSI[23]. |
| Patel et al | 2012 | Research Article | Patients who are high risk and have various underlying medical illness and have age more than 60 years are the risk category of the patients where it is necessitated[26]. |
Conclusion
Three types of the SSI namely superficial incisional SSI, Deep incisional SSI and Space organ SSI among which the occurrence of the SI SSI. Various studies have shown that the preventive measures are more effective than the curative one. Usage of prophylactic such as antibiotics and preoperative showers are found to be effective in controlling the SSI in the abdominal surgical patients. The occurrence of the SSI is more in the abdominal surgical procedures and therefore extra caution is needed in order to curb the increasing figure of the SSI. 52 percentage were found to be Escherichia coli followed by gram positive. Only 23 percentage of the bacteria found were sensitive or responsive to the antibiotics which are given to the patient prior to the operating procedure. Finally, study concludes that around 16 percentage of the patients develop SSI which when converted to figures stood at 55. The study concluded that antibiotic prophylactic course should be designed according to the commonly identified cultures from the pus samples of the SSI which can be beneficial to prevent the infection at first place.
References
- Calderwood MS, Huang SS, Keller V, Bruce CB, Kazerouni NN, et al. (2017). Variable Case Detection and Many Unreported Cases of Surgical-Site Infection Following Colon Surgery and Abdominal Hysterectomy in a Statewide Validation. Infect Control Hosp Epidemiol, 38:1091-1097.
Publisher | Google Scholor - Danan E, Smith J, Kruer RM, Avdic E, Lipsett P, et al. (2018). Use and Effectiveness of Peri-Operative Cefotetan versus Cefazolin Plus Metronidazole for Prevention of Surgical Site Infection in Abdominal Surgery Patients. Surg Infect (Larchmt)., 19:388-396.
Publisher | Google Scholor - Henriksen NA, Deerenberg EB, Venclauskas L, Fortelny RH, Garcia-Alamino JM, et al. (2017). Triclosan-coated sutures and surgical site infection in abdominal surgery: the TRISTAN review, meta-analysis and trial sequential analysis. Hernia, 21:833-841.
Publisher | Google Scholor - Eeftinck Schattenkerk LD, Musters GD, Nijssen DJ, de Jonge WJ, de Vries R et al. (2021). The incidence of abdominal surgical site infections after abdominal birth defects surgery in infants: A systematic review with meta-analysis. J Pediatr Surg.
Publisher | Google Scholor - Gheorghe A, Calvert M, Pinkney TD, et al. (2012). Systematic review of the clinical effectiveness of wound-edge protection devices in reducing surgical site infection in patients undergoing open abdominal surgery. Ann Surg. 255:1017-1029.
Publisher | Google Scholor - Li X, Lin H, Zhu L, Chen J, Lei S, et al. (2022). The clinical effectiveness of wound edge protectors in reducing surgical site infection after abdominal surgery: meta-analysis. BJS Open.
Publisher | Google Scholor - Zucker BE, Simillis C, Tekkis P, Kontovounisios C. (2019). Suture choice to reduce occurrence of surgical site infection, hernia, wound dehiscence and sinus/fistula: a network meta-analysis. Ann R Coll Surg Engl. 101:150-161.
Publisher | Google Scholor - Di Re AM, Wright D, Toh JWT, et al. (2021). Surgical wound infection prevention using topical negative pressure therapy on closed abdominal incisions - the ‘SWIPE IT’ randomized clinical trial. J Hosp Infect, 110:76-83.
Publisher | Google Scholor - Whitehead-Clarke T, Windsor (2021). A: Surgical Site Infection: The Scourge of Abdominal Wall Reconstruction. Surg Infect (Larchmt), 22:357-362.
Publisher | Google Scholor - Tubre DJ, Schroeder AD, Estes J, Eisenga J, Fitzgibbons RJ (2018). Surgical site infection: the ‘Achilles Heel’ of all types of abdominal wall hernia reconstruction. Hernia, 22:1003-1013.
Publisher | Google Scholor - Alkaaki A, Al-Radi OO, Khoja A, et al. (2019). Surgical site infection following abdominal surgery: a prospective cohort study. Can J Surg., 62:111-117.
Publisher | Google Scholor - Bhangu A, Ademuyiwa AO, Aguilera ML, et al. (2018). Surgical site infection after gastrointestinal surgery in high-income, middle-income, and low-income countries: a prospective, international, multicentre cohort study. The Lancet Infectious Diseases. 18:516-525.
Publisher | Google Scholor - Langenberg JCM, Kluytmans JAJW, de Groot HGW, Ho GH, Veen EJ, et al. (2018). Surgical Site and Graft Infections in Endovascular and Open Abdominal Aortic Aneurysm Surgery. Surg Infect (Larchmt). 19:424-429.
Publisher | Google Scholor - Lioce CG, Davis EC, Bennett JW, Townsend FI, Bloch CP (2019). Scalpel blade contamination and risk of postoperative surgical site infection following abdominal incisions in dogs. BMC Res Notes. 12:459.
Publisher | Google Scholor - Bediako-Bowan A a. A, Mølbak K, Kurtzhals J a. L, Owusu E, Debrah S, et al. (2020). Risk factors for surgical site infections in abdominal surgeries in Ghana: emphasis on the impact of operating rooms door openings. Epidemiol Infect, 148:e147.
Publisher | Google Scholor - Ahmed K, Bashar K, Connelly TTM, Fahey T, Walsh SR. (2016). Reducing Surgical Site Infections in Abdominal Surgery: Are Ring Retractors Effective? A Systematic Review and Meta-Analysis. Surg Infect (Larchmt). 17:138-151.
Publisher | Google Scholor - Orth K. (2018). Preventing Surgical Site Infections Related to Abdominal Drains in the Intensive Care Unit. Crit Care Nurse. 38:20-26.
Publisher | Google Scholor - Winfield RD, Reese S, Bochicchio K, Mazuski JE, Bochicchio GV. (2015). Obesity and the Risk for Surgical Site Infection in Abdominal Surgery. Am Surg., 82:331-836.
Publisher | Google Scholor - Kong B, Bruns P, Raulefs S, et al. (2015). Metabolism gene signatures and surgical site infections in abdominal surgery. Int J Surg. 14:67-74.
Publisher | Google Scholor - Wu X, Tian W, Kubilay NZ, Ren J, Li J. (2016). Is It Necessary To Place Prophylactically an Abdominal Drain To Prevent Surgical Site Infection in Abdominal Operations? A Systematic Meta-Review. Surg Infect (Larchmt). 17:730-738.
Publisher | Google Scholor - Ruiz-Tovar J, Llavero C, Jimenez-Fuertes M, Duran M, Perez-Lopez M, et al. (2020). Incisional Surgical Site Infection after Abdominal Fascial Closure with Triclosan-Coated Barbed Suture vs Triclosan-Coated Polydioxanone Loop Suture vs Polydioxanone Loop Suture in Emergent Abdominal Surgery: A Randomized Clinical Trial. J Am Coll Surg,. 230:766-274.
Publisher | Google Scholor - Alkhaibary A, Alharbi A, Khairy S. (2020). In Reply to the Letter to the Editor Regarding ‘Predictors of Surgical Site Infection in Cranioplasty: A Retrospective Analysis of Subcutaneously Preserved Bone Flaps in Abdominal Pockets’. World Neurosurg. 139:658.
Publisher | Google Scholor - Tomsic I, Heinze NR, Chaberny IF, Krauth C, Schock B, et al. (2020). Implementation interventions in preventing surgical site infections in abdominal surgery: a systematic review. BMC Health Serv Res. 20:236.
Publisher | Google Scholor - Wojcik BM, Han K, Peponis T, Velmahos G, Kaafarani HMA. (2019). Impact of Intra-Operative Adverse Events on the Risk of Surgical Site Infection in Abdominal Surgery. Surg Infect (Larchmt), 20:174-183.
Publisher | Google Scholor - Maehara Y, Shirabe K, Kohnoe S, et al. (2017). Impact of intra-abdominal absorbable sutures on surgical site infection in gastrointestinal and hepato-biliary-pancreatic surgery: results of a multicenter, randomized, prospective, phase II clinical trial. Surg Today, 47:1060-1071.
Publisher | Google Scholor - Patel SV, Coughlin SC, Malthaner RA. (2013). High-concentration oxygen and surgical site infections in abdominal surgery: a meta-analysis. Can J Surg. 56:E82-E90.
Publisher | Google Scholor - Miyoshi N, Fujino S, Nishimura J, et al. (2022). Effectiveness of Triclosan-Coated Sutures Compared with Uncoated Sutures in Preventing Surgical Site Infection after Abdominal Wall Closure in Open/Laparoscopic Colorectal Surgery. J Am Coll Surg, 234:1147-1159.
Publisher | Google Scholor - Kılıç E, Uğur M. (2018). Effect of therapeutic hypothermia on superficial surgical site infection and postoperative pain in urgent abdominal surgery. Ulus Travma Acil Cerrahi Derg., 24:417-412.
Publisher | Google Scholor - Yerra P, Sistla SC, Krishnaraj B, Shankar G, Sistla S, et al. (2021). Effect of Peri-Operative Hyperoxygenation on Surgical Site Infection in Patients Undergoing Emergency Abdominal Surgery: A Randomized Controlled Trial. Surg Infect (Larchmt). 22:1052-1058.
Publisher | Google Scholor - Utsumi M, Yamada T, Yamabe K, et al. (2022). Differences in risk factors for surgical site infection between laparotomy and laparoscopy in gastrointestinal surgery. PLoS One, 17:e0274887.
Publisher | Google Scholor - Rasheed H, Diab K, Singh T, et al. (2021). Contemporary Review to Reduce Groin Surgical Site Infections in Vascular Surgery. Ann Vasc Surg. 72:578-588.
Publisher | Google Scholor - Roy S, Patkar A, Daskiran M, Levine R, Hinoul P, Nigam S. (2014). Clinical and economic burden of surgical site infection in hysterectomy. Surg Infect (Larchmt). 15:266-273.
Publisher | Google Scholor - Narueponjirakul N, Breen KA, El Hechi MW, et al. (2021). Abdominal Wall Thickness Predicts Surgical Site Infection in Emergency Colon Operations. J Surg Res. 267:37-47.
Publisher | Google Scholor - Chang Y-WW, Murphy K, Yackzan D, et al. (2021). Abdominal Wall Thickness is a Predictor for Surgical Site Infections in Patients Undergoing Colorectal Operations. Am Surg, 87:1155-1162.
Publisher | Google Scholor - Muchuweti D, Jönsson KUG. (2015). Abdominal surgical site infections: a prospective study of determinant factors in Harare, Zimbabwe. Int Wound J. 12:517-522.
Publisher | Google Scholor