Review Article
Surgical Procedures with Questionable Indications Used in Russia
Peoples’ Friendship University of Russia, 117198 Moscow, Russia.
*Corresponding Author: Sergei V. Jargin, Peoples’ Friendship University of Russia, 117198 Moscow, Russia.
Citation: Sergei V. Jargin. (2024). Surgical Procedures with Questionable Indications Used in Russia, Clinical Research and Reports, BioRes Scientia Publishers. 2(5):1-12. DOI: 10.59657/2995-6064.brs.24.033
Copyright: © 2024 Sergei V. Jargin, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: July 10, 2024 | Accepted: July 30, 2024 | Published: August 06, 2024
Abstract
This review summarizes available data on invasive procedures applied with questionable indications in Russia in the recent past: mastectomy with the removal of muscles, gastrectomy for peptic ulcers, spleno-renal anastomosis for diabetes mellitus, thoracic surgery for bronchial asthma, overuse of surgery in tuberculosis, excessive and compulsory treatments of alcohol-dependent patients, etc. Among factors contributing to the use of invasive procedures with unproven efficiency have been the partial isolation from international scientific community, insufficient consideration of the principles of professional autonomy, informed consent and scientific polemics, training of medical personnel. It is known that invasive procedures can exert a placebo effect, which might have contributed to reported efficiency of some methods discussed here. However, by definition, placebo must be free of risks.
Keywords: peptic ulcers; gastrectomy; diabetes; portosystemic shunting; asthma; lung denervation; medical ethics
Introduction
The main topic of this review is excessive use of invasive procedures in the Russian healthcare. Clinical recommendations are generally avoided here. This gave to the author a possibility to limit citation of international literature: the number of references supporting the narration is quite large already. It is known that invasive procedures can exert a placebo effect, which might have contributed to reported efficiency of some methods discussed here. However, by definition, placebo must be free of risks and adverse effects. Factors contributing to the persistence of suboptimal practices in Russian Federation (RF) include a partial isolation from the international scientific community, shortages of medical education, unavailability of many internationally used handbooks [1,2]. Admittedly, foreign literature is available via the Internet today, many guidelines being adjusted to international standards. It is taken for granted and nobody gives thanks. On the contrary, some writers analyze complications of therapy in foreign countries without mentioning similar phenomena in RF [3]; details and references are in the book [4].
Certain published guidelines have remained without due commentaries, so that a comeback of outdated methods is not excluded. Suboptimal practices have been used as per instructions by healthcare authorities and leading experts’ publications. The lacking professional autonomy has contributed to the persistence of outdated methods [5]. Some colleagues encountered impediments to their careers when they did not collaborate in dubious research and practice. Manipulation of statistics has been not unusual [4]. In conditions of paternalism, misinformation of patients, persuasion and compulsory treatments are deemed permissible [6]. Justifications of surgical hyper-radicalism could be heard in private conversations among medics, for example: “The hopelessly ill are dangerous” i.e., may commit reckless acts undesirable by the state. For example, glioblastoma patients have been routinely operated on, while it was believed by some staff that the treatment was generally useless, just forcing patients to spend the rest of their lives in bed [7]. One of the motives to overuse invasive procedures was personnel training, among others, with the purpose of readiness for war. Some invasive methods with questionable indications were introduced or advocated by first generation military surgeons. In this connection, the limitations of medical education in the former Soviet Union (SU) should be mentioned. The Soviet period brought about an expansion of admission numbers to universities and medical educational institutions, sometimes with little regard for the quality of the academic preparation of students [2]. Of note, military and medical ethics are not the same. The comparatively short life expectancy in RF is a strategic advantage as it necessitates less healthcare investments and pensions. Military functionaries and their relatives will become more dominant thanks to the Ukraine war. Those participating in it, factually or on paper, are obtaining the veteran status and hence privileges over fellow-citizens. Some of them will occupy leading positions at universities, scientific and healthcare institutions without adequate preparation and selection. War veterans enjoy advantages in the healthcare and everyday life; there are, however, misgivings that the status has been awarded gratuitously to some individuals from the privileged milieu. At the same time, some relatives of superior officers evaded military service under various pretexts. In particular, many institutions of higher education grant exemption from the conscription. Being not accustomed to hard and meticulous work, some of the functionaries’ children have been involved in professional and other kind of misconduct [4, 8].
As far as we know, the Soviet and present rulers, the party and military nomenklatura [9], did not allow the use of invasive procedures without indications on themselves and their relatives. Functionaries’ sons did not treat gonorrhea by tamponade and bougienage of the urethra [10]; alcoholics from their milieu have not been compulsorily treated by drip infusions being infected with viral hepatitis [11]. As for the medical personnel, it is unlikely that they cauterized cervical ectopies (discussed below) or performed Halstead mastectomy on their family members. Dentists would not apply dry cutting to discolored pits and fissures or demineralized enamel surfaces in their children [12]. This means that there has been deliberate infliction of bodily harm. Finally, the obstacles to the importation of drugs and medical equipment should be mentioned. Domestic products are promoted sometimes despite suboptimal quality and possible counterfeiting.
Methods
This is a narrative review based predominantly on the Russian-language and partly on international literature. The search of literature was performed mainly on the PubMed, on the Internet, in libraries and the electronic database eLibrary.ru. The data from the literature have been reviewed and synthesized on the basis of the author's observations since the 1970s. It should be mentioned in this connection that, unlike other countries, public libraries are rarely used in RF and usually contain no professional medical literature. Medical libraries are hindered from using by the general public, including even retired doctors, by technical difficulties [13].
Breast cancer
According to the author’s estimates after a practice of pathology abroad (repeatedly during 1990-2013), an average size of malignant tumors in surgical specimens was larger in Moscow university clinics than in hospitals in Europe, Southern Africa and Iraq [14], which reflects the timeliness of cancer diagnostics. Another difference: almost all mastectomy specimens abroad were without muscle. The worldwide tendency towards a more sparing breast cancer management was not followed in the former SU for decades. In the 1980s and decreasingly in the 1990s, the Halsted procedure with the removal of both Pectoralis muscles was a predominant method of breast cancer (BC) management [15-18]; it was presented as the main treatment modality of BC in some textbooks and monographs published in the 21st century [19-21].
The principle of informed consent was often disregarded. Patients with early cancers underwent mastectomies with resection of pectoral muscles. A surgery could be extended to a radical (Halsted) procedure if an intraoperative frozen section found an early (2 cm) BC [22]. The latter operation is known to be associated with complications. Even more radical methods with removal of parasternal and other lymphatic collectors were recommended and applied [23]. Newly developed mastectomy modalities with the muscle resection have been patented [24, 25]. Advanced age was not regarded as contraindication to a radical surgery [26]. In view of complications, some experts recommended the modified radical mastectomy of Patey with resection of only the smaller pectoral muscle for T1-2 laterally located BCs [27-29]. Other experts advocated the Halsted procedure [30].
The Patey operation is also associated with adverse effects; nonetheless, it has been broadly used in the RF during last decades. At the time of the author’s practice (1995-1998) at the Ostroumov hospital in Moscow, incorporating the Center for Breast Diseases, almost all mastectomy specimens independently of tumor size included the smaller pectoral muscle; but the Halsted procedure was applied as well. The “gradual abandonment of the Halsted operation” was discussed in 2007 [31]. The study of symptoms after mastectomy in 247 women included 121 (48%) patients who underwent the operation of Patey and 73 (29%) that of Halsted [32]. In papers dated 2015-2022, the Patey operation was still mentioned as a routine procedure [33-35]; but the preservation of both pectoral muscles was finally becoming a standard.
Today, the recommendations are adjusted to international patterns. However, another extreme is observed: mastectomy without removal of pectoral muscles is called mutilation allegedly causing severe moral injury, whereas “the reconstruction has become an integral part of the breast cancer management” [36]. Such statements are accompanied by images of patients after reconstructive surgery, where breasts look (almost) as if not operated on. Apparently, the motive is economic one as the costs of plastic surgery are borne by patients. Indications to different methods of breast cancer management are beyond the scope of this review. Obviously, esthetic demands can be met in many cases by external prostheses.
Diabetes mellitus
The surgical spleno-renal anastomosis with the shunting of pancreatic blood into the systemic circulation was introduced by Eduard Galperin [37-40] and applied for the treatment of insulin-dependent diabetes mellitus. At the same time, Galperin wrote: “Diabetic patients generally tolerate surgery very poorly” [40]. The method was applied in type 2 diabetes as well [41,42]. The supposed mechanism was “creating a more optimal interaction of subcutaneously injected insulin and glucagon produced in pancreas” [38]. Of note, in patients with liver cirrhosis the surgical portocaval shunting resulted in deterioration of glucose tolerance [43]. Diabetes mellitus was regarded as a contraindication for portocaval anastomosis [44].
In a series of 415 patients, early post-operative complications were observed in 28 patients including 2 cases of sepsis, 5 of pyelonephritis, 5 of pneumonia; 2 patients died in the first post-surgery week. Ketonuria was observed in 18 patients [45], in agreement with the known fact that surgical stress may trigger ketosis in diabetics. Comparable percentages of complications were quoted in another paper [38]. The patients were subdivided into groups with a strong, moderate and absent effect [39]. There was no group with worsening, so that the assessment was probably biased.
According to another report, thrombosis of the shunt was found by angiography in 27% of the patients within eight months after the operation [46]. Severe acidosis was designated as a typical complication [46, 47]. The anti-diabetic efficiency of the shunting was moderate both in humans and in experimental dogs, whereas a majority of the animals did not survive the diabetes induction by streptozotocin or pancreatic resection with a subsequent shunting surgery [37]. During one-year (1990) engagement in the United States, Galperin used his methods on dogs and rats deploring that there was no opportunity to apply it in humans [40].
By 2011, the surgical treatment of diabetes described above was still in use while a risk of shunt thrombosis was pointed out [47, 48]. The same experts applied renoportal venous anastomosis for the treatment of chronic hepatitis and arterial hypertension [47, 49]. In the course of the operations, wedge biopsies from the pancreas (~0.64 cm) and core biopsies from kidney were collected. Histological descriptions included glomerulitis with proliferation of mesangial cells, their relocation to the periphery of capillary loops, mesangial interposition and formation of double-contoured basement membranes. The authors postulated that mesangioproliferative glomerulonephritis is the initial stage of diabetic glomerulopathy [50,51]. In fact, mesangial interposition and double-contoured basement membranes are typical for membranoproliferative glomerulonephritis. This condition, if found in a diabetic patient, should be seen as a superimposed condition, potentially needing immunosuppressive therapy. Renal biopsy is generally indicated for diabetics only if a kidney disease other than diabetic nephropathy is suspected; more details and references are in the preceding paper [52]. The misrepresentation of histological criteria of glomerulonephritis as features of diabetic nephropathy may lead to inadequate therapy. Of note, renal and pancreatic biopsies are associated with risks. Invasive procedures applied within the framework of the surgical treatment of diabetes included also renal and splenic venography and celiac arteriography [38, 45].
Peptic ulcers
The surgical treatment of gastro-duodenal ulcers in the former SU has been different from the international practice. Gastrectomy became the predominant method of peptic ulcer management after the 24th All-Union Congress of Surgeons in 1938 [53,54]. According to the author’s observations, gastric resections were comparatively rarely performed abroad for peptic ulcers; their volume was more limited, often corresponding to antrectomy. For perforations, an ulcer excision was usually performed and an annular specimen was sent to the pathology department. Laparoscopic repair is used increasingly these days. In RF, primary gastric resection (2/3-4/5 of the stomach), antrectomy with vagotomy, or a simple suture have been applied in ulcer perforations [55-60]. Relapses after gastric resections or suturing of perforated ulcers were treated by gastrectomy [61]. At the same time, adverse effects of resections were generally known by experts [53, 62]. The limited availability of modern medical therapy was designated as a social indication for gastrectomy [57].
The hyper-radicalism in the gastric surgery originates from the well-known surgeon Sergei Yudin (lately spelled Iudin), who was a “passionate supporter of gastric resections in ulcer perforations” [63]. During the Second World War, Yudin was one of the leading surgeons of the Red Army. He was known for his radical approach: wide resection rather than drainage of wounds [63]. His leitmotif was: “Unhesitatingly excise muscular tissue to access fractured bone” [64]. The former health minister B.V. Petrovsky wrote that Yudin’s hyper-radicalism in the military surgery, followed by colleagues, led to hemorrhages, extensive defects of bone and soft tissues [65, 66].
According to Yudin’s teachings, the pylorus and lesser curvature must be removed at an ulcer surgery. His articles advocating gastrectomy for peptic ulcers were republished with favorable editorial commentaries [67]. References to Yudin’s publications continued until recently, quoting the fact that he performed gastrectomy in 75% of perforated ulcers [66]. Resection of the stomach in case of perforation has been advocated by many experts from the former SU [53, 57, 68-73]. The supposed benefit from resections was ascribed to the limited availability of modern drugs. In some articles recommending gastrectomy, it was claimed that medical therapy does not achieve a complete recovery, so that resection should be performed early enough to prevent complications [69]. The definition “complete recovery” seems to be hardly applicable to the condition after gastrectomy. Anyway this strategy has been in disagreement with that applied in other countries [74]. Like in many topics discussed here, recommendations are currently adjusted to international patterns. Recent guidelines included laparascopic treatments and ulcer excision along with the suturing and resection as treatment options for perforated ulcers. A drastic decrease in surgery rate among ulcer patients during last decades with almost complete disappearance of elective resections [75-77] confirms the fact of overtreatment in the recent past.
Bronchial asthma and respiratory diseases
Another method to be commented is the thoracic surgery with the denervation of lungs as a treatment of bronchial asthma [78-80] depicted as “the most accepted procedure” in the Guidelines by the Ministry of Health [81]. Among others, the “skeletonization” of pulmonary roots with transection of nerves, auto-transplantation of lungs (complete separation with immediate re-implantation) or cross-section of trachea with subsequent suturing were applied [80,82,83].
The theoretical ground was the hypothesis that denervation “prevents abnormal nervous impulsation” [78]. Such argumentation was usual at that time, when the so-called ideas of nervism, based on the concept of trophic function of nerves, were officially promoted. Exaggerated histological descriptions of “dystrophy” or degeneration in the autonomic nervous system, claimed to be irreversible, were presented as a theoretic basis of the denervation [78, 84].
Stepan Babichev, the main protagonist of the asthma surgery, was a first-generation military surgeon, later the chancellor of Moscow Medical Stomatological Institute (currently named University) and assistant of the health minister. The surgical treatment of asthma was officially recommended by the Ministry of Health; whereas thoracotomy with lung denervation was designated as “the most accepted surgical treatment” [81]. The skeletonization was recommended for steroid-dependent and infectious-allergic asthma forms [81, 85]. Repeated bronchoscopies were applied post-surgery because of the bronchial drainage impairment [80]. The overuse of bronchoscopy in children and adults has been discussed elsewhere [86].
The pulmonary denervation and lung resections were recommended also for asthma cases when drug and inhalation therapy had been efficient. It was suggested that medical treatment prior to the operation must be limited in time [81]. In one study, indications for surgery were found in 41.7% of 986 asthma patients; 457 operations were performed with complications recorded in 58 (12.3%) of the cases. The following adverse effects were observed: in 27 patients – inflammatory complications; 12 – neurological symptoms including dysphagia, vocal fold palsy or Horner syndrome; 11 – pulmonary complications such as pneumonia, empyema, pneumothorax, 8 – bleeding and/or local circulatory derangements; 2 cases of paraplegia and hemiparesis; 6 patients died within 32 days after the operation [87].
In 2002, the surgical modality was still in use [79]. Denervation was sometimes performed simultaneously with lung resection, lobectomy or bilobectomy [88]. In this connection, a quote from the recommendations of the Health Ministry deserves attention: “The widespread concept that indication for surgery in asthma is the ineffectiveness of conservative therapy is incorrect. The presence of foci of chronic inflammation in the lungs and bronchi, even with a good effect from medical treatment, is an indication for surgery. Delaying the operation serves to involve other parts of the bronchial tree in the inflammatory process, enhances the degree of allergy, degenerative changes in the innervation apparatus and endocrine organs” [81]. Such instructions could lead to resections without sufficient indications.
As mentioned above, the denervation surgery was sometimes combined with removal of pulmonary segments or lobes regarded by the operators as pathologically altered [81]. Lung resections in asthma were applied also without denervation, even in the cases where drug and inhalation therapy were effective. Among indications for the surgical treatment have been focal lesions: chronic pneumonia, bronchiectasis and “bronchitis deformans” [89]. Sokolov and co-workers reported that ≤10% of their asthma patients had been operated on [90]. The operations were performed also in patients with bilateral inflammatory or fibrous lesions, both in exacerbations and in remissions, supposed to be indicated for a radical treatment of asthma. This concept was propagated by Fedor Uglov, who claimed a “resection of infected foci” to be the purpose of asthma management [89, 91]. The therapy was based on his belief that “in 98% of cases, the cause of asthma is focal chronic pneumonia” [89].
Asthma patients were transferred from medical departments for the surgical and endoscopic treatment. “After a course of therapeutic bronchoscopies”, Uglov and co-workers performed resections of the parts of lungs regarded by them to be pathologically changed [89, 91]. Resections were applied to children with recurrent bronchitis and/or pneumonia; while particular efficiency of pneumonectomy was stressed, also in bilateral chronic pneumonia [92]. The recommendation for progressive chronic pneumonia was “lobectomy for segmentary lesions and pneumonectomy in all other patients” [93]. The claimed purpose of the operation was the removal of focal infection. Localized chronic pneumonia with bronchial lesions was by itself regarded to be indication for lung resection [89,91].
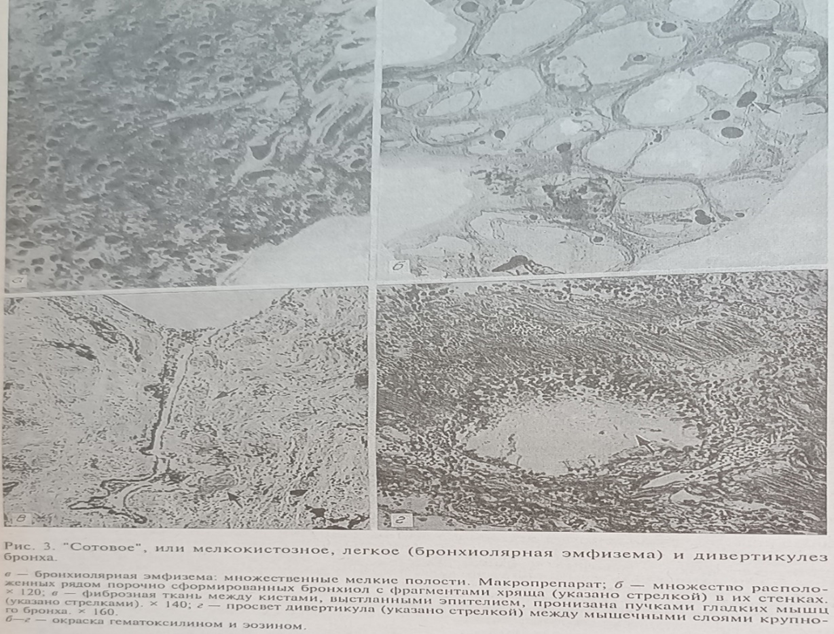
Reportedly, “dysontogenetic” lung diseases in children were a more frequent indication for radical surgery than acquired conditions; whereas lobe- and pneumonectomies were predominantly applied [94]. Irina Esipova and co-workers found malformations in 66% of resected specimens from children operated on for relapsing pneumonia or “bronchitis deformans” [95] (Figure 1). The same authors claimed that, contrary to preceding publications, the changes in the lungs were not diffuse but local, thus justifying resections.
Professor Esipova, a well-known specialist in pulmonary pathology, claimed that misdiagnosis of malformations as chronic bronchitis led to undue postponements of lung resections [95]. In accordance with this doctrine, pathologists described in resected lobes and segments inflammatory infiltration, fibrosis, dystrophy and malformations without specifying their extent and severity, while descriptions deviated from those in standard editions on pulmonary pathology, histological specimens being poor quality (Figure 1) [95, 96]. Contemporary international literature was referenced scarcely in suchlike papers.
Figure 1
Figure 1
Figure 1: Histological images described as lung malformations in children: top adapted from [95]; middle and bottom from [96], commented in the text. The nature, extension and clinical significance of these lesions are unclear.
Some proposed criteria of malformations were formulated and illustrated unconvincingly: large bronchi with uneven, serrated (jagged) contours, bush-like aggregations of small bronchi and bronchioles, variously differentiated mesenchyme with lymphoid infiltration, rhythmic muscular fascicles, local agenesis of alveoli represented by connective tissue, abnormal tissues alternating with normal structures, etc. (Figure 1) [96]. Reading descriptions by Esipova and co-workers, it is evident for an ex-Soviet pathologist that some resected pulmonary lobes or segments were not significantly abnormal: macroscopically whitish foci and coal pigment, singular cysts 2-3 mm; microscopically atypical bronchial branching, lack of a bronchus narrowing from the center to periphery, “nudity” of bronchi, hypoplasia of bronchial walls, abnormal epithelial cilia, and so forth [95]. Descriptions of this kind were sometimes used for largely normal specimens; clinical significance of the findings being unclear. However, such reports from pathology departments were suitable to justify resections.
Undoubtedly, in some cases the surgery was indicated; but there has been an overtreatment tendency. It was rightly noted that many authors made no distinction between congenital malformations and developmental variants [97]. In a more recent publication, an opinion was expressed that some histological phenomena described as malformations are common in postnatal lungs normally or after resolved pneumonia [98]. It was also noticed that diagnostics of lung malformations was difficult; the percentage of wrong diagnoses amounting to 65-75% [99]. Nevertheless, the patients were operated based on the assumption that inflammatory complications are inevitable in future [99]. Concluding their articles, some pathologists generalized that the “disease that affects children in the first year of life, against the background of morpho-functional immaturity of the lungs, intense metabolic processes and imperfection of local nonspecific and immunological defense, is accompanied by a breakdown of typical protective reactions, impaired regeneration and postnatal development of the lungs, excessive expression and rapid depletion of compensatory and adaptive processes. The latter underlies the alterative-exudative changes, the impossibility to delimit inflammation, determines the progressive course of bronchiectasis and requires surgical treatment at the age of 2-6 years (emphasis added)” [100]. An overuse of surgery in tuberculosis and/or alcoholism has been discussed elsewhere [12,101].
Cauterization of ectocervix
Electro- and thermocoagulation of cervical ectopy, regardless of the presence of epithelial dysplasia, has been routinely applied in RF. It should be commented that cervical ectopy or ectropion is called pseudo-erosion (colloquially erosion) in Russia, while the term ectropion is mainly used for the cervix eversion after delivery.
The ectopy per se was regarded to be precancerous or “predisposing” to cancer [102-104]. Cylindrical endocervical-type epithelium and mucous glands within the ectopy were designated as “pathological tissue” that must be removed [105]. It was also claimed that cervical pseudo-erosions contribute to infertility and complications of pregnancy [106]. Cervical erosions and pseudo-erosions were found at mass preventive checkups (so-called dispensarisations [107]) and coagulated by electro- or thermocautery [108,109]. It occurred in accordance with the Soviet-time concept of prophylaxis priority in the healthcare. It was recommended to start the treatment of pseudo-erosions possibly early, while large lesions were to be treated by “diathermoconization” by means of an electrocautery electrode [104], a procedure associated with complications [110]. It should be noted that according to the international literature, in many women during the reproductive period, the mucin-secreting columnar epithelium of the endocervix is present on the cervical surface, forming the endocervical ectropion or ectopy, which is considered to be normal [111].
At the same time, Pap smears have been performed rarely and not up to the quality standards, cervical cancer being diagnosed later than in other developed countries [112]. Ablative methods are advertized and recommended by some contemporary Russian-language literature; images and references are in [113]. For example, relapsing endocervical ectopy without epithelial dysplasia has been presented as an indication for cryotherapy although this method impedes histological examination [114]. Other experts recommend laser, cryo- or electrocoagulation for acquired endocervical ectopy [115]. For leukoplakia without cell atypia a loop excision is recommended [116]. Some medical practices possess only one device for ablative therapy [114] and use it sometimes with questionable indications.
Conclusion
Factors contributing to the use of invasive procedures with questionable indications have included the partial isolation from international scientific community, insufficient consideration of the principles of professional autonomy, informed consent and scientific polemics, as well as paternalistic attitude to patients. Today, there is a possibility to acquire modern equipment; and research is on the rise. Under these conditions, the purpose of this review was to remind that, performing surgical or other invasive procedures, the risk-to-benefit ratio must be kept as low as reasonably possible. Insufficient international coordination of medical studies and partial isolation from the scientific community may lead to parallelism in research with repetition of studies on a low-quality level, unnecessary experimentation, and application of invasive procedures without sufficient indications. Considering shortcomings of medical practice, research and education, governmental directives and increase in funding are unlikely to be a solution. Measures for improvement of the healthcare in RF must include participation of authorized foreign advisors.
Declarations
Funding
There was no funding
Conflict of interest
The author declares no conflict of interest.
References
- Senokosova EK. (2019). Prestupnaja nekompetentnost' i nedobrosovestnost' v medicine (Criminal incompetence and dishonesty in medicine).
Publisher | Google Scholor - Jargin SV. (2013). Some aspects of medical education in Russia. Am J Med Stud, 1(2):4-7.
Publisher | Google Scholor - Vovk EI, Vertkin AL, Zairatyants OV, Frolova YuV. (2007). Foreign experience in registering and analyzing the poor outcomes of treatment. Arkh Patol, 69(5):16-24.
Publisher | Google Scholor - Jargin SV. (2020). Misconduct in medical research and practice. New York: Nova Science Publishers.
Publisher | Google Scholor - Danishevski K, McKee M, Balabanova D. (2009). Variations in obstetric practice in Russia: a story of professional autonomy, isolation and limited evidence. Int J Health Plann Manage, 24:161-171.
Publisher | Google Scholor - Mikirtichan GL, Kaurova TV, Pestereva EV. (2022). Vvedenie v bioetiku (Introduction to bioethics). St. Petersburg: Pediatric Medical University.
Publisher | Google Scholor - Jargin SV. (2024). The treatment of glioblastoma: Letter from Russia. J Cancer Sci, 9(1):1.
Publisher | Google Scholor - Jargin SV. (2022). Military aspects of malingering, sexual and reproductive coercion: Report from Russia. J Forensic Investigation, 10(1):5.
Publisher | Google Scholor - Voslensky MS. (1984). Nomenklatura: the Soviet ruling class. Garden City, NY: Knopf Doubleday.
Publisher | Google Scholor - Jargin SV. (2016). Treatment of gonorrhea in Russia: Recent history. Global Journal of Dermatology & Venereology, 4(1):5.
Publisher | Google Scholor - Jargin SV. (2024). Alcohol and alcoholism in Russia: An update. J Addiction Prevention, 12(1):1.
Publisher | Google Scholor - Jargin SV. (2022). Dentistry in Russia: Past and presence. J Oral Biol, 8(1):6.
Publisher | Google Scholor - Murphy J, Jargin S. (2017). International trends in health science librarianship part 20: Russia. Health Info Libr J, 34:92-94.
Publisher | Google Scholor - Jargin S. (2011). Histopathology in Iraq: reliable diagnostics in spite of shortages. Turk Patoloji Derg, 27(2):177-179.
Publisher | Google Scholor - Letiagin VP. (1992). The treatment of primary breast cancer. The late results. Ter Arkh, 64(10):33-37.
Publisher | Google Scholor - Levin AO, Miasnikova MO. (1992). Saving the musculus pectoralis minor in radical mastectomy. Vopr Onkol, 38(1):80-84.
Publisher | Google Scholor - Pereslegin IA, Nikitina TP. (1990). Surgical, radiation and drug treatment of breast cancer. Med Radiol (Mosk), 35(6):39-44.
Publisher | Google Scholor - Pronin VI, Rozanov IuL, Zolotarevskii VIa, Akimov AA, Vel'sher LZ. (1990). Radical mastectomy technics. Khirurgiia (Mosk), 2:52-55.
Publisher | Google Scholor - Kazachenok VM, Baryash VV. (2005). Zabolevaniia molochnoi zhelezy (Breast diseases). Minsk: Belarusian Medical University.
Publisher | Google Scholor - Kovanov VV, Perelman MI. (2001). Operacii na grudnoi stenke i organah grudnoi polosti (Operations on the chest and thoracic cavity organs). In: Kovanov VV, editor. Operativnaia hirurgia i topograficheskaia anatomia (Operative surgery and topographic anatomy). Moscow: Meditsina, 297-321.
Publisher | Google Scholor - Semiglazov VV, Topuzov EE. (2009). Rak molochnoi zhelezy (Breast cancer). Moscow: Medpress-inform.
Publisher | Google Scholor - Demidov VP, Pak DD, Ostrovtsev LD. (1990). Errors in the treatment of breast cancer. Khirurgiia (Mosk), (4):90-95.
Publisher | Google Scholor - Kholdin SA, Dymarskii LIu. (1975). Rasshirennye radikalnye operacii pri rake molochnoi zhelezy (Extended radical operations in breast cancer). Leningrad: Meditsina.
Publisher | Google Scholor - Druzhkov BK, Druzhkov OB. (1996). The method of extended mastectomy. Patent of Russian Federation RU95106525A1.
Publisher | Google Scholor - Tsejlikman EG, Patsyrova LA, Vaganov. NV. (2008). Method of mastectomy with preservation of greater pectoral muscle. Patent of Russian Federation RU2335249C2.
Publisher | Google Scholor - Suspitsyn IuV, Letiagin VP, Ivanov VM, Orlova PN. (1990). Treatment of breast cancer in middle-aged and elderly menopausal women. Sov Med, 3:72-76.
Publisher | Google Scholor - Bazhenova AP, Madich KK, Khakhanashvili GN, Sikharulidze AV. (1987). Experience in performing the Patey-Dyson operation in cancer of the breast. Khirurgiia (Mosk), (4):37-42.
Publisher | Google Scholor - Kuzin MI, Shkorob OS, Kulakova AM, Bukhteeva NF. (1977). Indications for Patey's operation in breast cancer. Khirurgiia (Mosk), (2):19-23.
Publisher | Google Scholor - Kuzin MI, Shkrob OS, Kulakova AM, Zal'tsman IN, Zolotarevskii VB. (1981). Diagnosis and treatment of nonpalpable breast tumors. Vopr Onkol, 27(5):3-10.
Publisher | Google Scholor - Datsenko VS, Abisheva AB. (1977). Patey mastectomy in the combined treatment of breast cancer. Vopr Onkol, 23(2):48-53.
Publisher | Google Scholor - Khvastunov RA, Kireev AV, Nikolskiy IV, Suvorov VA. (2007). Single-step mastectomy and laparoscopic ovariectomy in the treatment of breast cancer. Journal of Modern Oncology, 9(3):24-28.
Publisher | Google Scholor - Shihkerimov RK, Savin AA, Stulin ID, Velsher LZ, Stakhanov ML, et al. (2008). Neurological disorders in women after mastectomy. Klinicheskai︠a︡ gerontologii︠a︡, 14(8):15-18.
Publisher | Google Scholor - Bektursynov SM, Bayduvaliev AM. (2015). Treatment of breast cancer with the use preoperative radiotherapy. International Journal of Applied and Fundamental Research, (10):80-83.
Publisher | Google Scholor - Bukkieva T, Pospelova M, Efimtsev A, Fionik O, Alekseeva T, et al. (2022). Functional network connectivity reveals the brain functional alterations in breast cancer survivors. J Clin Med, 11(3):617.
Publisher | Google Scholor - Yarema VI, Fatuev OE, Stepanyants NG, Safronova VV. (2019). Immediate and remote results of surgical interventions on the breast. Research’n Practical Medicine Journal (Issled Prakt Med), 6(2):110-119.
Publisher | Google Scholor - Khailenko VA, Khailenko DV, Makarov ES. (2023). Radikalnaya mastektomia i odnomomentnye rekonstruktivno-plasticheskie operacii pri rake molochnoi zhelezy s primeneniem endoprotezov (Radical mastectomy and simultaneous reconstructive plastic surgery for breast cancer using endoprostheses). In: Ryabchikov DA, Petrovsky AV, editors. Rak molochnoi zhelezy (Breast cancer). Moscow: Geotar-Media, 201-210.
Publisher | Google Scholor - Galperin EI, Kuzovlev NF, Diuzheva TG, Aleksandrovskaia TN. (1983). Approaches to surgical treatment of diabetes mellitus (experimental study). Khirurgiia (Mosk), 1:13-20.
Publisher | Google Scholor - Galperin EI, Diuzheva TG, Petrovsky PF, ChevokinAYu, Dokuchayev KV, et al. (1996). Results of pancreatic blood shunting into the systemic blood flow in insulin-dependent diabetics. HPB Surg, 9(4):191-197.
Publisher | Google Scholor - Galperin EI, Diuzheva TG, Rabinovich SE, Platonova LV, Severgina ES, et al. (1996). Distal spleno-renal shunt. A surgical approach to the management of diabetes mellitus patients. Annaly Khirurgicheskoy Gepatologii (Annals of Surgical Hepatology), (1):77-90.
Publisher | Google Scholor - Galperin EI. (2017). O sebe vsluh (Aloud about myself). Moscow: Vidar-M.
Publisher | Google Scholor - Kirnus LM, Che V, Makarov NA, Burovkin BA, Shvartsshtein VIa, et al. (1995). Method for surgically treatmet of second type diabetes mellitus. Patent of Russian Federation RU2036610C1.
Publisher | Google Scholor - Putintsev AM, Shraer TI, Sergeev VN, Maslov MG, Strukova OA. (2010). Variants of surgical management for severe arterial hypertension combined with type 2 diabetes mellitus. Angiol Sosud Khir, 16(2):120-125.
Publisher | Google Scholor - Pezzarossa A, Contini S, Bonora E, Marni A, Colotto G, et al. (1986). Glucose tolerance after portacaval shunt in liver cirrhosis. Diabete Metab, 12(4):197-202.
Publisher | Google Scholor - Dittrich H. (1964). Der Diabetes mellitus, eine Kontraindikation für portocavale Anastomosenoperationen. Langenbecks Arch Klin Chir Ver Dtsch Z Chir, 308:594-598.
Publisher | Google Scholor - Diuzheva TG. (1992). Hirurgicheskoe lechenie bolnyh insulinzavisimym saharnym diabetom (Surgical treatment of patients with insulindependent diabetes mellitus). Dissertation. Moscow: I.M. Sechenov Medical Academy.
Publisher | Google Scholor - Nikonenko AS, Kovalev AA, Zavgorodnii SN, Volkova NA. (1996). Surgical treatment of insulin-dependent diabetes mellitus and its complications. Khirurgiia (Mosk), (2):81-83.
Publisher | Google Scholor - Torgunakov SA, Torgunakov AP. (2010). Possible causes of thrombus-related hazard of a distal splenorenal venous anastomosis. Angiol Sosud Khir, 16(4):184-188.
Publisher | Google Scholor - Torgunakov AP, Torgunakov SA, Magerramova EF. (2011). Method for surgical treatment of diabetes mellitus. Patent of Russian Federation RU2421163C1.
Publisher | Google Scholor - Pokrovskii AV, Kazanchian PO, Babloian GV, Sharipov EM. (1986). Renoportal venous anastomosis in the treatment of patients with arterial hypertension. Khirurgiia (Mosk), (6):44-50.
Publisher | Google Scholor - Severgina ES, Ponomarev AB, Diuzheva TG, Shestakova MV, Maiorova EM. (1994). Diabetic glomerulonephritis - the first stage of diabetic glomerulopathy. Arkh Patol, 56(4):44-50.
Publisher | Google Scholor - Severgina ES. (1995). Morphology and pathogenesis of insulindependent diabetes mellitus. Dissertation. Moscow: I.M. Sechenov Medical Academy.
Publisher | Google Scholor - Jargin SV. (2024). Renal biopsy: History and perspectives. J Pathol Diagn Microbiol, 101.
Publisher | Google Scholor - Balalykin DA. (2004). Introduction of pathogenic principles of surgical treatment of ulcer disease in Russian surgery. Khirurgiia (Mosk), (10):73-78.
Publisher | Google Scholor - Brekhov EI, Skobelkin OK, Bashilov VP, Korepanov VI, Smol'ianinov MV. (1983). Stomach resection in peptic ulcer and cancer. Khirurgiia (Mosk), (3):33-37.
Publisher | Google Scholor - Afendulov SA, Zhuravlev GIu, Smirnov AD, Krasnolutskii NA. (2006). Preventive surgical treatment of ulcer disease. Vestn Khir Im I I Grek, 165(3):18-23.
Publisher | Google Scholor - Chernousov AF, Khorobrikh TV, Bogopolsky PM. (2016). Hirurgia iazvennoi bolezni zheludka i dvenadcatiperstnoi kishki (Surgery for gastric and duodenal ulcers). Moscow: Prakticheskaia medicina,
Publisher | Google Scholor - Gostishchev VK, Evseev MA, Golovin RA. (2009). Radical operative treatment of perforative gastroduodenal ulcer disease. Khirurgiia (Mosk), (3):10-16.
Publisher | Google Scholor - Potashov LV, Semenov DIu, Ushveridze DG, Osmanov ZKh, Chekmasov IuS, Panina AV. (2005). Long-term results of closure of perforated pyloro-duodenal ulcers. Vestn Khir Im I I Grek, 164(5):40-42.
Publisher | Google Scholor - Sazhin IV, Sazhin VP, Bronshtein PG, Savel’ev VM, Nuzhdikhin AV, Klimov DE. (2014). Laparoscopic treatment of perforated ulcers. Khirurgiia (Mosk), (7):12-16.
Publisher | Google Scholor - Vachev AN, Koryttsev VK, Antropov IV. (2014). Method of selecting operation volume in case of perforated ulcers of stomach and duodenum. Patent of Russian Federation RU2506886C1.
Publisher | Google Scholor - Bachev II. (1990). Reoperations in ulcer recurrence after surgical treatment of peptic ulcer. Khirurgiia (Mosk), (2):66-69.
Publisher | Google Scholor - Pantsyrev IuM, Mikhalev AI, Fedorov ED, Cherniakevich SA. (2008). Hirurgicheskoe lechenie oslozhnennoi jazvennoi bolezni (Surgical treatment of complicated ulcer disease). In: Abakumov MM; Saveliev VS (ed). 80 lekcii po hirurgii (Eighty lectures in surgery). Moscow: Litterra, 468-480.
Publisher | Google Scholor - Alexi-Meskishvili V, Konstantinov IE. Sergei S. (2006). Yudin: an untold story. Surgery,139(1):115-122.
Publisher | Google Scholor - Iudin SS. (1943). Metodika operacii pri ognestrelnyh perelomah bedra v usloviah sovremennoi voiny (Surgical methods for gunshot hip fractures in modern warfare). Moscow: Medgiz.
Publisher | Google Scholor - Petrovsky BV. (1989). Hirurg i zhizn (The surgeon and life). Moscow: Meditsina.
Publisher | Google Scholor - Petrovsky BV. (1991). About Sergei Sergeevich Iudin. In: Iudin SS. Selected works. Moscow: Meditsina, 356-375.
Publisher | Google Scholor - Iudin SS. (1991). Sketches of gastric surgery. Khirurgiia (Mosk), (9):152-161.
Publisher | Google Scholor - Nishanov FN, Batirov AK, Abdiraiimov BA, Abdullazhanov BR, Nishanov MF. (2011). Current state of the problem of surgical treatment of perforating duodenal ulcers. Vestn Khir Im I I Grek, 170(5):97-100.
Publisher | Google Scholor - Babalich AK. (1999). Surgical treatment of patients with duodenal ulcer. Khirurgiia (Mosk). (7):19-22.
Publisher | Google Scholor - Komarov NV, Maslagin AS, Komarov RN. (2001). Surgical treatment of patients with complications of peptic ulcer of the stomach and duodenum under conditions of a regional hospital. Vestn Khir Im I I Grek, 160(2):104-106.
Publisher | Google Scholor - Kuzin MI, Chistova MA. (1995). The stomach and duodenum. In: Kuzin MI (ed). Hirurgicheskie bolezni (Surgical diseases). Moscow: Meditsina, 337-407.
Publisher | Google Scholor - Repin VN, Kostylev LM, Poliakov SN, Matveeva NA. (2011). Choice of the operation for perforated ulcers of the stomach and duodenum. Vestn Khir Im I I Grek, 170(2):48-51.
Publisher | Google Scholor - Vachev AN, Korytsev VK, Antropov IV. (2013). The choice of resection volume by the combination of perforative duodenal ulcer with other complications of the ulcer disease. Khirurgiia (Mosk), (11):29-31.
Publisher | Google Scholor - Chung KT, Shelat VG. (2017). Perforated peptic ulcer - an update. World J Gastrointest Surg, 9(1):1-12.
Publisher | Google Scholor - Larichev AB, Maiorov MI, Favstov SV, Shalop'ev AG. (2014). Clinical-epidemiological aspects of gastric and duodenum ulcer. Vestn Khir Im I I Grek, 173(2):100-104.
Publisher | Google Scholor - Mariyko VA, Romanova NN, Kremyansky MA, Tretyakov VO, Mariyko AV. (2019). Current state of elective surgery for peptic ulcer. Khirurgiia (Mosk), (4):24-29.
Publisher | Google Scholor - Vlasov AP. (2020). New technologies for stomach resection surgery in atypical conditions. Khirurgiia (Mosk), (9): 20-27.
Publisher | Google Scholor - Babichev SI, Kharlampovich SI, Tarasova LB, Smakov GM, Savchenko ZI. (1985). Partial denervation of the lungs in bronchial asthma. Khirurgiia (Mosk), (4):31-35.
Publisher | Google Scholor - Gudovskii LM, Karashurov SE, Karashurov ES, Volkov AA, Parshin VD. (2002). Surgical treatment of bronchial asthma. Khirurgiia (Mosk), (7):14-18.
Publisher | Google Scholor - Meshalkin EN, Al'perin LIa. (1978). Razlichnye metody denervacii legkih v hirurgii bronhialnoj astmy (Various methods of lung denervation in bronchial asthma surgery). Tashkent: Meditsina.
Publisher | Google Scholor - (1988). Health Ministry of RSFSR. Pokazania i protivopokazania k operativnomu lecheniu bronhialnoi astmy (Indications and contraindications for the surgical treatment of bronchial asthma). Moscow.
Publisher | Google Scholor - Meshalkin EN. (1968). Primi tentativi di una terapia chirurgica dell’asma bronchiale con il metodo dell'autotrapianto polmonare. G Ital Mal Torace, 22:15-22.
Publisher | Google Scholor - Giller BM, Giller DB, Giller GV. (1998). New methods of the surgical treatment of bronchial asthma. Probl Tuberk, (4):60-61.
Publisher | Google Scholor - Babichev SI, Lapin SK, Kharlampovich SI, Tarasova LB, Sazonova VI. (1983). Substantiation of the surgical treatment of patients with bronchial asthma and chronic pneumonia. Khirurgiia (Mosk), (4):5-10.
Publisher | Google Scholor - Smakov GM. (1999). Pathogenetic substantiation of lung denervation in bronchial asthma and it’s indications. Khirurgiia (Mosk), (2):67-69.
Publisher | Google Scholor - Jargin SV. (2017). Bronchoscopy in children for research with questionable indications: an overview of russian patents and publications. Recent Pat Drug Deliv Formul, 11(2):83-88.
Publisher | Google Scholor - Smakov GM. (1990). Complications of surgical treatment of patients with bronchial asthma. Khirurgiia (Mosk), (2):124-127.
Publisher | Google Scholor - Babichev SI, Batishchev NG, Bareisha VM. (1972). Surgical treatment of bronchial asthma. Khirurgiia (Mosk), 48(12):52-56.
Publisher | Google Scholor - Uglov FG. (1976). Patogenez, klinika i lechenie hronicheskoi pnevmonii (Pathogenesis, clinic and therapy of chronic pneumonia). Moscow: Meditsina.
Publisher | Google Scholor - Sokolov SN, Gerasin VA, Moiseev NV, Leont’ev AI. (1975). Results of lung resections in bronchial asthma. Grudn Khir, (1):105-108.
Publisher | Google Scholor - Uglov FG. (1984). Pod beloi mantiei (Under the white mantle). Moscow: Sovietskaia Rossia.
Publisher | Google Scholor - Glkova TM, Volkova AV. (1968). Late results of surgery in children with chronic pneumonia. Vopr Okhr Materin Det, 13(8):13-17.
Publisher | Google Scholor - Shulutko ML, Kazak TI, Korobov VI, Mazur GI. (1972). Progressive chronic pneumonia. Grudn Khir,14(2):51-55.
Publisher | Google Scholor - Zolotarev SE. (1976). Osobennosti i otdalennye rezultaty radikalnyh operacii po povodu dizontogeneticheskih gnoinyh zabolevanii legkih u detei i podrostkov (Features and long-term results of radical operations for dysontogenetic purulent lung diseases in children and adolescents). In: Toluzakov VL, Shiriaeva KF, editors. Poroki razvitia i geneticheski obuslovlennye formy hronicheskih nespecificheskih zabolevanii legkih (Malformations and genetically determined forms of chronic nonspecific lung diseases). Collected volume. Leningrad: 1st Medical Institute, 35-36.
Publisher | Google Scholor - Esipova IK, Vladimirtseva AL, Biriukov VV. (1990). Branching defects and mucosal diverticulosis of the bronchi in children as factors predisposing to the development of chronic inflammatory processes in the lungs. Arkh Patol, 52(2):6-10.
Publisher | Google Scholor - Esipova IK, Vladimirtseva AL. (1996). Congenital malformations of the lungs. Arkh Patol, 58(3):49-54.
Publisher | Google Scholor - Perelman MI, Platov II. (1976). K voprosu o klassifikacii porokov razvitia legkih (On the classification of lung malformations). In: Toluzakov VL, Shiryaev KF, editors. Poroki razvitia i geneticheski obuslovlennye formy hronicheskih nespecificheskih zabolevanii legkih (Developmental defects and genetically determined forms of chronic nonspecific lung diseases). Collection of scientific works. Leningrad: 1st Medical Institute, 63-65.
Publisher | Google Scholor - Putov NV, Varlamov VV. Poroki razvitia legkih. (1999). Bronhoektaticheskaia bolezn (Malformations of the lungs. Bronchiectasis). St. Petersburg Medical University.
Publisher | Google Scholor - Lovacheva OV. (1984). Diagnostika porokov razvitia legkih v sochetanii s tuberkulezom. (Diagnosis of lung malformations in combination with tuberculosis). Dissertation. Moscow: Research Institute of Tuberculosis.
Publisher | Google Scholor - Bubnova NI. (1991). Morphogenesis of bronchiectasis in children of preschool age. Arkh Patol, 53(12):40-45.
Publisher | Google Scholor - Jargin SV. (2024). Invasive procedures used in tuberculosis with questionable indications: report from Russia. Preprints, 2024041176.
Publisher | Google Scholor - Abdushukurova KhM, Maidanik DI. (1981). Gynaecology. Dushanbe: Maorif.
Publisher | Google Scholor - Sivochalova OV. (1984). Cervix erosion. Feldsher Akush. 49(4):21-24.
Publisher | Google Scholor - Timoshenko LV. (1988). Prakticheskaia ginekologia (Practical Gynaecology). Kiev: Zdorov’ia.
Publisher | Google Scholor - Kiriushchenkov AP. (1986). Acute cervicitis and erosion of the cervix uteri. Feldsher Akush, (12):50-53.
Publisher | Google Scholor - Milianovskii AI, Senchuk AIa. (1990). Reproductive and menstrual functions in women after cryosurgical treatment of cervical diseases. Akush Ginekol (Mosk), (8):40-42.
Publisher | Google Scholor - Jargin SV. (2021). Potential issues associated with dispensarisations in Russia. Public Health, 198:e29-e30.
Publisher | Google Scholor - Lesiuk VS. (1963). On the problem of treatment of erosion of the cervix uteri and endocervicitis by different methods of heat coagulation. Akush Ginekol (Mosk), 39:83-86.
Publisher | Google Scholor - Bokhman IaV. (1985). Prevention of cancer of uterine cervix and corpus. In: Vsesoiuznyi simpozium “Ranniaia diagnostika, lechenie predopuholevyh i opuholevyh zabolevanii sheiki matki i dispanserizacia zhenskogo naselenia” All-Union Symposium in Pskov, USSR. “Early diagnostics, treatment of pretumorous and tumorous diseases of the uterine cervix and dispensarization of the female population.” Leningrad, 31-33.
Publisher | Google Scholor - Bychkov VI, Bykov EG, Bratus' AM. (1990). Complications and late results of the treatment of precancerous conditions of the cervix uteri by diathermic conization. Akush Ginekol (Mosk), (2):61-22.
Publisher | Google Scholor - Machado Junior LC, Dalmaso AS, Carvalho HB. (2008). Evidence for benefits from treating cervical ectopy: literature review. Sao Paulo Med J, 126:132-139.
Publisher | Google Scholor - Syrjänen S, Shabalova IP, Petrovichev N, Kozachenko VP, Zakharova T, et al. (2002). Human papillomavirus testing and conventional pap smear cytology as optional screening tools of women at different risks for cervical cancer in the countries of the former Soviet Union. J Low Genit Tract Dis, 6:97-110.
Publisher | Google Scholor - Jargin SV. (2024). Munchausen Syndrome by Proxy: A Report from Russia. J of Gyne Obste and Mother Health, 2(1):01-06.
Publisher | Google Scholor - Damirov MM. (2023). Kriogennyi metod lechenia zabolevanii sheiki matki (Cryogenic method of treatment of cervical diseases). Moscow: Geotar-Media.
Publisher | Google Scholor - Gantsev ShH. (2014). Zabolevania sheiki matki (Diseases of the cervix). Moscow: Geotar-Media.
Publisher | Google Scholor - Kuznetsova IA, Grechkanev GO, Kachalina OV, Borovkova LV. (2017). Diagnostika i lechenie zabolevanii sheiki matki. Sovremennye vozmozhnosti, analiz oshibok (Diagnosis and treatment of cervical diseases. Modern possibilities, error analysis). Nizhny Novgorod Medical Academy.
Publisher | Google Scholor