Research Article
Spontaneous or Nonsurgical Pneumoperitoneum: A Retrospective Study with A Review of Literature
1Assistant Professor, Department of Surgery ESICMCH Faridabad, India.
2Professor, Department of Surgery ESICMCH Faridabad, India.
*Corresponding Author: Saumya Chopra,Assistant Professor, Department of Surgery ESICMCH Faridabad, India.
Citation: Chopra S, Goyal S. (2024). Spontaneous or Nonsurgical Pneumoperitoneum: A Retrospective Study with A Review of Literature. International Journal of Medical Case Reports and Reviews, BioRes Scientia Publishers. 3(3):1-5. DOI: 10.59657/2837-8172.brs.24.048
Copyright: © 2024 Saumya Chopra, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: February 27, 2024 | Accepted: March 23, 2024 | Published: April 01, 2024
Abstract
Background: The presence of free air in the peritoneal cavity is called pneumoperitoneum. It is an emergency that requires immediate laparotomy. It is present in about 90% of the cases with a hollow viscous perforation. On the other hand, spontaneous, nonsurgical or idiopathic pneumoperitoneum is a benign surgical entity that needs no immediate surgery. It is a diagnostic dilemma for the surgeon as the clinical presentation and radiological findings imitate perforated viscous and may result in unnecessary laparotomy. History and physical examination are very important to rule out visceral perforation. A diagnostic peritoneal lavage, CECT, contrast studies, or laparoscopic evaluation can help prevent a patient from having unnecessary laparotomy.
Methodology: This retrospective study was done from Jan 2021 to June 2022. Fifty cases of pneumoperitoneum due to visceral perforation were admitted during this period. Only one case of spontaneous pneumoperitoneum was reported with a diagnostic dilemma treated conservatively.
Conclusion: This retrospective study identifies the presence of such a surgical entity, which can be managed conservatively, thus preventing the needless surgical burden of morbidity and mortality.
Keywords: spontaneous pneumoperitoneum; visceral perforation; laparoscopic evaluation; diagnostic peritoneal lavage; cect
Introduction
The pneumoperitoneum is described as free air under the diaphragm [1]. Intraperitoneal free air indicates hollow viscous perforation in over 90% of the patients, which is considered a surgical emergency. Rarely, the presence of pneumoperitoneum may not be due to intra-abdominal perforations (10 -15%) and thus may not require unnecessary emergency exploratory laparotomy. Such a condition poses a diagnostic dilemma to treating surgeons or ICU critical care team and is termed a "nonsurgical", "spontaneous", or "idiopathic" pneumoperitoneum. The causes may be intrathoracic, intra-abdominal, gynecological and idiopathic [2,3]. Emergency surgical intervention is important in patients with perforated viscous as delay may cause major morbidity and mortality due to sepsis, third space volume shift resulting in shock and multiple organ dysfunction syndrome [4]. The surgeons tend to operate at the earliest for pneumoperitoneum due to suspected perforated viscous. The patients might undergo unnecessary surgical intervention in case of spontaneous pneumoperitoneum, adding morbidity to the already sick patients. The decision to go for laparotomy cannot be made solely on the presence of pneumoperitoneum without any signs of peritonitis. In cases of high suspicion of perforated viscus, laparoscopy provides a good diagnostic and therapeutic tool. So, surgeons must know about this rare "spontaneous pneumoperitoneum" entity and should avoid unnecessary laparotomy. Hereby, we present a case of a middle-aged patient with spontaneous pneumoperitoneum managed conservatively.
Material & Method
This retrospective study was conducted from Jan 2021 to June 2022 at ESIC Medical College in Faridabad, India. Fifty cases of pneumoperitoneum due to visceral perforation were admitted to the surgery department during this period. All except one presented with features of peritonitis. This patient presented with pneumoperitoneum without any symptoms or signs of peritonitis. We faced a diagnostic dilemma.
Table 1: Agewise Distribution
| Age (yrs) | Number |
| 10-20 | 5 |
| 20-40 | 25 |
| 40-60 | 18 |
| >60 | 2 |
Table 2: Perforated Organs
| Organ | Number |
| Duodenal Perforation | 44 |
| Small Bowl | 6 |
Case Report
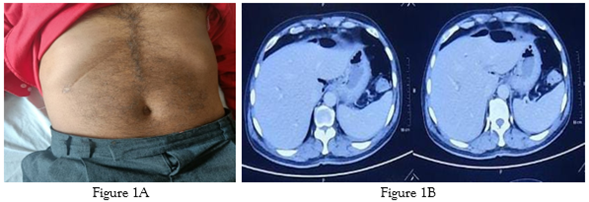
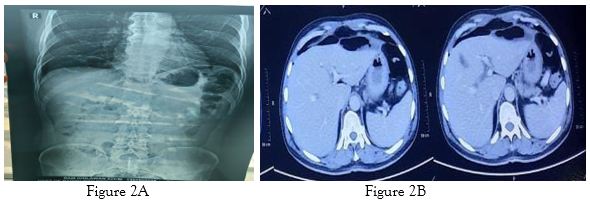
A 50-year-old male underwent Percutaneous Coronary Intervention stenting 4 years back for coronary disease. He has been maintaining well since then, when he presented to the casualty department with pain in the precordium for one day for admission and evaluation under the Cardiology department. There was a history of open cholecystectomy 20 years back. ECG, Echocardiography, cardiac enzymes and other cardiac causes were within normal limits. Chest X-ray showed significant free air under the diaphragm. On examination, there was no tachycardia, hypotension, fever, or abdominal signs or symptoms of peritonitis. Total leukocyte counts and ESR were within the normal limit. X-ray chest, including the upper abdomen, showed air under the right dome of the diaphragm. CECT Thorax and Abdomen with oral and IV contrast revealed free air under the diaphragm and no bowel leak [Fig-2A, B]. Delayed films were also taken, which showed no leak to the rectum. The patient's photo and abdomen X-rays at presentation are also shown. [Fig-1A, 1B].
Diagnostic laparoscopy ruled out visceral perforation, and the patient managed conservatively.
Discussion
Pneumoperitoneum, or gas in the peritoneal cavity, is a surgical emergency in adults and children. In about >90% of cases, perforated intra-abdominal viscous, e.g., peptic ulcer, Meckel's diverticulum, toxic megacolon, necrotizing enterocolitis, Crohn's disease, and/or perforation of the bowel due to trauma or tumors, are responsible for pneumoperitoneum [3]. The entity of 'benign', 'spontaneous',' nonsurgical (NSP) ', 'asymptomatic', or idiopathic pneumoperitoneum is reported in the literature, which, when identified, needs conservative management only. Surprisingly, not all hollow viscous perforations result in pneumoperitoneum, and only 69% of the cases of gut perforation are present with air under the diaphragm on X-ray [4]. This can happen due to spontaneous perforation sealing with invisible minimal gas leakage. Similarly, all pneumoperitoneum is not due to perforated viscus. The decision to go for laparotomy cannot be made solely on the presence of pneumoperitoneum without signs of peritonitis. Such cases in the literature are explained as nonsurgical pneumoperitoneum or spontaneous pneumoperitoneum [2,5,6]. Most nonsurgical (spontaneous) pneumoperitoneum cases may occur as a procedural complication or a complication of medical intervention. The most common abdominal aetiology of NSP can be retained postoperative air (prevalence 25% to 60%). NSP frequently occurs after peritoneal dialysis catheter placement (10% to 34%) and gastrointestinal endoscopic procedures (0.3% to 25%, varying by procedure) [7]. The pathophysiology of spontaneous pneumoperitoneum is unclear. When there is increased intra-thoracic pressure, air may dissect its way downwards along the oesophagus and aorta into the retroperitoneal tissue 8. The air can also dissect/tear through the diaphragm defects in the posterolateral region secondary to arrest in the closure of the pleuroperitoneal canal and diaphragmatic defects at the sternocostal and lumbo-coastal region [9]. Another suggested theory is that there are micro-perforations (2 to 4 mm) in the anterior wall of the stomach, which can cause pneumoperitoneum [10].
The causes of spontaneous pneumoperitoneum can be divided into
Intrathoracic, Abdominal, Gynecological and Idiopathic.
1. Thoracic
Pneumothorax, pleuroperitoneal fistula, pneumomediastinum due to thoracic trauma, barotraumas, cardiopulmonary resuscitation and pneumonia.
2. Abdomina
Abdominal causes include pneumatosiscystoides intestinalis. In this disease, gas-filled submucosal or sub-serosal cysts are mostly found in the terminal ileum and are the most important cause due to the bursting of these air-filled cysts.
Upper gastrointestinal endoscopy, emphysematous cholecystitis and post-surgical pneumoperitoneum are other possible causes.
3. Gynecological
Forceful coitus, vaginal douching, pelvic inflammatory disease & postpartum knee-chest exercise are possible gynecological causes [11].
4. Idiopathic
In the current era of increasing critical care, ventilator management and COVID cases, idiopathic pneumoperitoneum is no longer a diagnosis of exclusion. It should be kept in mind while evaluating critically ill patients in ICU with sepsis and ventilator support. If feasible, moving ahead with exploratory laparotomy must be planned after cross-sectional imaging with oral and IV contrast.
Table 3: Causes of spontaneous pneumoperitoneum in tabular form. [12].
| Cause | Mechanism |
| Pneumomediastinum | Trauma or foreign body in the oesophagus, causing pneumoperitoneum that later filters through the diaphragm. |
| Pneumothorax | It is the same as in pneumomediastinum. |
| Cardiopulmonary resuscitation | Blunt chest trauma secondary to chest compressions or as a consequence of visceral perforation. |
| Mechanical ventilation | Vol trauma and air filtration in the perivascular and peribranchial space. |
| Thoracic abscess | Due to the difference in pressures between atelectasis and open alveoli. |
| Vaginal warm showers, postpartum, postcoital state | Through the fallopian tubes that communicate the uterine cavity with the abdominal cavity. |
| Pneumatosis intestinalis | Filtration through the perivascular space. |
Reviewing the literature revealed that watchful waiting is important with favourable outcomes. It also helps decrease hospital stays and avoid unnecessary surgeries with related morbidity and mortality. Conservative treatment was successful in Idiopathic cases without signs of peritonitis [13].
Review of literature for spontaneous pneumoperitoneum
Table 4: Shows cases of Spontaneous pneumoperitoneum and its causes
| Sno | Author | NO. of cases | Symptoms | Investigations | Treatment | Possible Diagnosis |
| 1 | Wright AR [10] | 1 | Pain in epigastric region | Xray abdomen – air under the diaphragm | Exploratory laparotomy no hollow viscus peroration. Dye through the left fimbriae passed easily to the uterus. | Post tubal insufflation |
| 2 | Van Gelder HM et al. [14] | 7 | Clinically acute abdomen | Xray abdomen – air under the diaphragm In 1 patient, Diagnostic Peritoneal Lavage- negative | Exploratory laparotomy- no hollow viscus peroration for 6 patients. 1 patient with negative DPL was managed conservatively. | Idiopathic |
| 3 | Kadkhodaie HR [15] | 1 | Post blunt trauma injury to the left upper limb. Emphysema after induction of general anaesthesia. No abdominal signs or symptoms. | Xray abdomen – air under the diaphragm, no pneumothorax CT abdomen- free air, no other pathology visible. | Conservative Management | Emphysema |
| 4 | Wang H et al. [16] | 1 | Kcometscapancreas, ERCP stenting, 1 year back. | Response CT scan revealed pneumoperitoneum. Post-conservative management CT showed resolution of pneumoperitoneum. | Conservative Management | Post-ERPC stenting |
| 5 | Hannan E et al. [17] | 1 | Recurrent LRTI, No abdominal signs or symptoms. | CT thorax and abdomen revealed pneumoperitoneum, no other bowel pathology. | Conservative Management | Recurrent LRTI |
| 6 | Sidiqi MM et al. [18] | 1 | KCO Small cell carcinoma lung in remissionwith COPD, presented with dyspnea, no abdominal signs or symptoms | PCTA- Free air in peritoneum | Conservative Management | ? COPD |
| 7 | Sakaguchi T [19] | 1 | Kcosarcoidosis and PE, on apixaban. | Screening CT – Pneumoperitoneum, UGIE edematous stomach mucosa. No ulcer. | Conservative Management | Sarcoidosis |
| 8 | Gemio del Rey IA [20] | 1 | COVID-positive pt on ventilator support with decreasing counts and rising CRP | CXR- Free gas under the diaphragm CECT thorax and abdomen with oral and IV contrast- Free air, no bowel leak | Conservative Management | Covid pneumonia |
Management
This condition is demanding as most cases are misdiagnosed as perforated viscus. The literature review advocates for conservative management if peritoneal signs of visceral perforation are absent. However, if peritoneal signs of perforation are present, then laparotomy is necessary. Avoid negative exploratory laparotomy in patients with spontaneous pneumoperitoneum and thus save the patients from unnecessary morbidity [21].
Diagnostic laparoscopy is a good diagnostic and therapeutic tool in a hemodynamically stable patient with pneumoperitoneum without obvious features of viscera perforation. It will prevent unnecessary exploratory laparotomy with morbidity in already sick patients, especially in the COVID era, when many patients need prolonged ICU stay and mechanical ventilation (both risk factors for spontaneous pneumoperitoneum).
Conclusion
Spontaneous pneumoperitoneum means air under the diaphragm without hollow viscous perforation. It is an uncommon surgical entity and is a diagnostic dilemma in the patient without signs of peritonitis, where the X-ray shows gas under the diaphragm. The treating surgeon should maintain a high index of suspicion for nonsurgical causes of pneumo-peritoneum and recognize that conservative management may be indicated in many cases. In stable patients with elements of pneumoperitoneum, diagnostic laparoscopy can be considered to rule out visceral perforations. In pneumoperitoneum patients with features of peritonitis, laparotomy is justified.
References
- Ostrowski A, Williams R, Broderick G, Panagopoulos V, Kyriazis I, et al. (2017). Scientific program of 35th World Congress of endourology program book and abstracts. J Endourol, 31:1-474
Publisher | Google Scholor - Mularski RA, Ciccolo ML, Rappaport WD. (2000). Nonsurgical causes of pneumoperitoneum. West J Med,170: 41-46.3.
Publisher | Google Scholor - Mann CM, Bhati CS, Gemmell D, Doyle P, Gupta V, et al. (2010). Spontaneous pneumoperitoneum: Diagnostic and management difficulties. Emerg Med Aust, 6:568-570.4.
Publisher | Google Scholor - Winek TG, Mosely HS, Grout G, Luallin D. (1998). Pneumoperitoneum and its association with ruptured abdominal viscus. Arch Surg, 123:709-712.5
Publisher | Google Scholor - Pitiakoudis M, Zezos P, Oikonomou A, Kirmanidis M, Kouklakis G, et al. (2011). Spontaneous idiopathic pneumoperitoneum presenting as an acute abdomen: A case report. J Med Case Rep, 5:86.
Publisher | Google Scholor - Estridge P, Akoh JA. (2017). Recurrent spontaneous pneumoperitoneum: A surgical dilemma. Int J Surg Case Rep. 30:103-105.
Publisher | Google Scholor - Mularski RA, Sippel JM, Osbourne ML. (2000). Pneumoperitoneum: A review of nonsurgical causes. Crit Care Med, 28:2638-2644.
Publisher | Google Scholor - Gummalla P, Mundakel G, Agaronov M, Lee H. (2017). Pneumoperitoneum with‑out intestinal perforation in a neonate: case report and literature review. Case Rep Pediatr, 1-5.
Publisher | Google Scholor - He TZ, Xu C, Ji Y, Sun XY, Liu M. (2015). Idiopathic neonatal pneumoperitoneum with the favorable outcome: a case report and review. World J Gastroenterol, 21(20):6417-6421.
Publisher | Google Scholor - Wright AR. (1959). Spontaneous Pneumoperitoneum AMA Arch Surg, 78(3):500-502.
Publisher | Google Scholor - Hovelius L. (1973). Pneumocholecystitis: An uncommon cause of pneumoperitoneum. Acta Chir Stand, 139:410.
Publisher | Google Scholor - Williams NM, Watkin DF. (1997). Spontaneous pneumoperitoneum and other nonsurgical auses of intraperitoneal free gas. Postgrad Med J, 73(863):531-537.
Publisher | Google Scholor - Williams NM, Watkin DF. (1997). Spontaneous pneumoperitoneum and other nonsurgical causes of intraperitoneal free gas. Postgrad Med J, 73:531-537.
Publisher | Google Scholor - van Gelder HM, Allen KB, Renz B, Sherman R. (1991). Spontaneous pneumoperitoneum. A surgical dilemma. Am Surg, 57(3):151-156.
Publisher | Google Scholor - Kadkhodaie HR*, Vaziri M. (2008). Asymptomatic Spontaneous Pneumoperitoneum. Shiraz E Medical Journal, 9(4):2008.
Publisher | Google Scholor - Wang H, Batra V. (2018). Massive Pneumoperitoneum Presenting as an Incidental Finding. Cureus, 10(6):e2787.
Publisher | Google Scholor - Hannan E, Saad E, Hoashi S, Toomey D. (2019). The clinical dilemma of the persistent idiopathic pneumoperitoneum: A case report. Int J Surg Case Rep, 63:10-12.
Publisher | Google Scholor - Sidiqi MM, Fletcher D, Billah T. (2020). The enigma of asymptomatic idiopathic pneumoperitoneum: A dangerous trap for general surgeons. Int J Surg Case Rep, 76:33-36.
Publisher | Google Scholor - Sakaguchi T, Kotsuka M, Yamamichi K, Sekimoto M. (2021). Management of incidentally detected idiopathic pneumoperitoneum: A case report and literature review. Int J Surg Case Rep, 87:106463.
Publisher | Google Scholor - Gemio del Rey IA, de la Plaza Llamas R, Ramia JM, Medina Velasco AA, Dı´az Candelas DA. (2021). Neumoperitoneoesponta´neo no quiru´ rgico en paciente COVID-19 positivo con neumonı´a bilateral severa.Cir Esp, 99:469-471.
Publisher | Google Scholor - Tung-Lung W. (2013). Spontaneous pneumoperitoneum: Report of one case. J. Acute, 3: 20-22.
Publisher | Google Scholor