Research Article
Spontaneous Intracranial Hematoma (ICH) Registry in A Tertiary Care Center in South India-Disease and Surgery Profiles Explained
- Sibhi Ganapathy *
- Nair A
- Jagadeesh A
- Munireddy A
- Raykar R
- Shailesh AVR
Department of Neurosurgery, St. Johns Medical College, Bangalore, India.
*Corresponding Author: Sibhi Ganapathy, Department of Neurosurgery, St. Johns Medical College, Bangalore, India.
Citation: S Ganapathy, Nair A, Jagadeesh A, Munireddy A, Raykar R, et al. (2023). Spontaneous Intracranial Hematoma (ICH) Registry in A Tertiary Care Center in South India-Disease and Surgery Profiles Explained. Journal of Neuroscience and Neurological Research, BRS Publishers 2(1); DOI: 10.59657/2837-4843.brs.23.005
Copyright: © 2023 Sibhi Ganapathy, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: September 21, 2022 | Accepted: January 30, 2023 | Published: February 04, 2023
Abstract
Objective: To assess the feasibility of plain decompressive hemicraniectomy in the treatment of spontaneous hypertensive intracranial bleeds as a low-cost and low-skill alternative for decompression and hematoma evacuation.
Methodology: A retrospective cohort analysis of all the spontaneous hypertensive bleeds operated in a tertiary care center in southern India was planned, all surgical cases were analyzed and the mortality and morbidity differences between procedures employed were understood.
Results: Of the 18 patients operated on with decompression with hematoma evacuation, a high mortality rate of 26 cases was noticed (50%), significantly more than plain decompressive hemicraniectomy (12.5% was seen across all patients irrespective of preoperative GCS or comorbidities.
Conclusion: Decompressive hemicraniectomy is a viable alternative to decompression with hematoma evacuation. This is especially relevant in rural settings where expertise and equipment are in short supply and transport to higher centers implies a delay in surgery, often associated with significant morbidity and mortality.
Keywords: decompressive hemicraniectomy; decompression with hematoma evacuation; spontaneous intracranial hematomas; rural neurosurgery
Introduction
Neurosurgical emergencies are time-bound. The emergent nature of the disease along with a sudden rise in intracranial pressure can precipitate a crisis of existence for the patient. The problem is acutely felt in rural centers where the lack of facilities and expertise can hamper the delivery of efficient and timely neurosurgical care to patients who require it. The decompressive hemicraniectomy (DHC) is a simple procedure to decrease ICP and limit the damage to the brain while at the same time promoting recovery and healing. It requires minimal expertise and facilities, making it the mainstay of neurosurgical emergencies.
We in this study attempted to retrospectively compare the efficacy and efficiency of this procedure with decompression with hematoma evacuation (DHCE) which is practiced in centers with better facilities and expertise, to determine if DHC can be made a standard of care in rural areas to ensure timely and efficient treatment of neurosurgical emergencies such as Spontaneous intracerebral bleeds (SICH or ICH) without compromising on the quality of care.
Materials and Methods
Data regarding all spontaneous Intracerebral hematomas (ICH) secondary to hypertension were collected retrospectively from the records in tertiary care high volume centers in Bengaluru city, in south India. The patients and surgeries were collected for a period of one year. The data regarding demographics, Glasgow Coma Scale (GCS) pre and after surgery, distribution of bleed, surgery, outcomes, deficits, and other parameters were tabulated and analyzed. Ultimately, in one group (n = 32), DHC was performed without clot evacuation, while in the other (n = 18), craniotomy with clot evacuation was done. The data compiled, collated, and analyzed is presented below.
Results
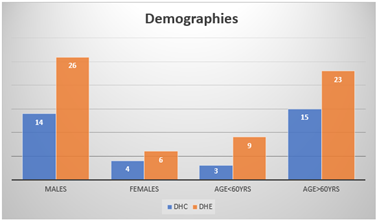
Most patients who suffered a spontaneous intracranial haemorrhage were males and above the age of 60 years. Factors like old age, male sex, Asian ethnicity, chronic kidney disease, and hypertension are already known to increase the risk of ICH.
Figure 1
Figure 2
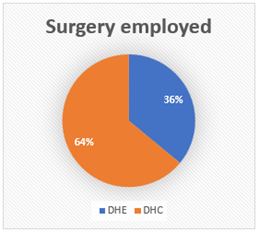
The preference for decompressive hemicraniectomy (DHC) vs hematoma evacuation (DHE) was left to the preference of the operating surgeon. The surgeons’ experience varied from 4-5years post-graduation to trainees performing surgery under supervision. As the analysis is a retrospective one, control over the types of surgery done could not be exercised. In our study, 36% were simple DHC while most of the surgeries were DHE (64%) as shown in the table
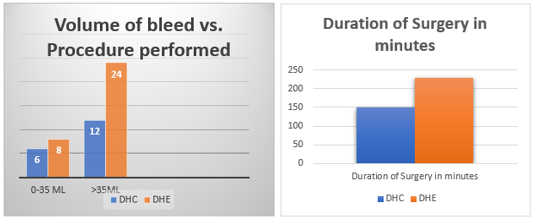
Most bleeds operated for were with a volume of more than 35ml. A decompressive hemicraniectomy was opted for as the procedure in more cases than a hematoma evacuation. Reasons for this could be multifactorial, like
- Shorter duration of the surgery – which was an average of 150 minutes for a simple hemicraniectomy compared to 230 minutes for an evacuation.
- Expertise of the operating surgeon
- Need for rapid ICP correction
Figure 3
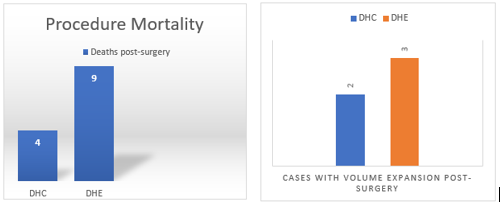
Out of the 13 deaths following an intervention, we found that those who underwent a hematoma evacuation were more at risk of mortality. On average, decompressive hemicraniectomy opens an additional space of 79 mL,15 larger than the size of most intraparenchymal hematomas which may reduce the harm from hematoma while trauma to the brain parenchyma from hematoma evacuation may offset the benefits of the additional mass effect reduction. 5 of our cases developed volume expansion after the procedure with a higher incidence after a hematoma evacuation.
Figure 4
Figure 5
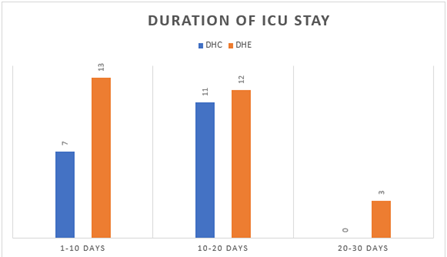
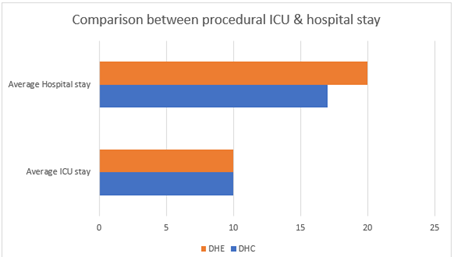
All 18 patients who underwent an evacuation of the hematoma needed ICU management (100%). In comparison, 56.25% of post-DHC patients were admitted in intensive care. However, none of the patients who underwent a hemicraniectomy required an ICU stay beyond 20 days, and the average number of days a patient spent in the hospital was more after an evacuation.
Figure 6
Discussion
In this review, we describe evidence regarding the feasibility of performing a decompressive hemicraniectomy instead of a decompression and hematoma evacuation. Several parameters have been considered to measure the role of the procedure in the management of intracranial bleeds. A hemicraniectomy was attempted for 42% of bleeds below 35ml and 33% of bleeds with a volume that was higher and procedure mortality in patients who underwent a craniectomy was 6% lesser than in those who underwent an evacuation. A hemorrhage can trigger a series of negative pathogenic mechanisms soon after its onset. ICP elevation can be caused by the additional volume of the hematoma undergoing expansion and overpowering the cerebral autoregulatory mechanism. Hematoma expansion seemed to occur in 5 cases and data proves that the chances of its occurrence were far superior after an evacuation. Decompressive hemicraniectomy can be a solution to this problem. Besides, the trauma of open craniotomy and especially to the brain parenchyma for hematoma evacuation may not be necessary. Hematoma evacuation takes much longer to perform and needs more expertise. Surgical hematoma evacuation can ironically also cause an increase in ICP due to tissue manipulation and venous obstruction from the coagulation of veins during surgery. On the contrary, a decompressive craniectomy may achieve a lower ICP by channeling edema away from the midline structures and towards the bone defect instead.
Conclusion
This study highlights the numerous merits of treating a DHC namely a decreased risk of trauma to the brain, speed of the procedure, and a comparative decrease in the incidence of complications. A DHC should hence be considered a part of the armamentarium in the management of hypertensive intracranial bleeds, especially in smaller centers with less experienced surgeons.
Acknowledgements
No financial interests are present to declare.
Funding: None.
Conflicts of interest: None declared.
References
- Takeuchi S, Wada K, Nagatani K, Otani N, and Mori K. (2013). Decompressive hemicraniectomy for spontaneous intracerebral hemorrhage. Neurosurgical Focus. 34(5):5.
Publisher | Google Scholor - Fung C, Murek M, Z’Graggen W.J, Krähenbühl A.K, Gautschi O.P, Schucht P, Gralla J, Schaller K, Arnold M, Fischer U and Mattle H.P. (2012). Decompressive hemicraniectomy in patients with supratentorial intracerebral hemorrhage. Stroke. 43(12):3207-3211.
Publisher | Google Scholor - Heuts S.G, Bruce S.S, Zacharia B.E, Hickman Z.L, Kellner C.P, Sussman E.S, McDowell M.M, Bruce R.A and Connolly E.S. (2013). Decompressive hemicraniectomy without clot evacuation in dominant-sided intracerebral hemorrhage with ICP crisis. Neurosurgical Focus. 34(5):4.
Publisher | Google Scholor - Murthy J.M.K, Chowdary G.V.S, Murthy T.V.R.K, Bhasha P.S.A and Naryanan T.J. (2005). Decompressive craniectomy with clot evacuation in large hemispheric hypertensive intracerebral hemorrhage. Neurocritical care. 2(3):258-262.
Publisher | Google Scholor - Rasras S, Safari H, Zeinali M and Jahangiri M. (2018). Decompressive hemicraniectomy without clot evacuation in supratentorial deep-seated intracerebral hemorrhage. Clinical neurology and neurosurgery. 174:1-6.
Publisher | Google Scholor - Li L, Molian V.A, Seaman S.C, Zanaty M, Howard M.A, Greenlee J.D, Hasan D.M and Leira E.C. (2021). Impact of Intracerebral Hematoma Evacuation During Decompressive Hemicraniectomy on Functional Outcomes. Stroke. 52(3):1105-1108.
Publisher | Google Scholor - Poblete R.A, Zheng L, Arenas M, Vazquez A, Yu D, Emanuel B.A, Kim-Tenser M.A, Sanossian N and Mack W. (2019). Older Age Is Not Associated with Worse Outcomes Following Decompressive Hemicraniectomy for Spontaneous Intracerebral Hemorrhage. Journal of Stroke and Cerebrovascular Diseases. 28(11):104320.
Publisher | Google Scholor - Ramnarayan R, Anto D, Anilkumar T.V and Nayar R. (2009). Decompressive hemicraniectomy in large putaminal hematomas: an Indian experience. Journal of Stroke and Cerebrovascular Diseases. 18(1):1-10.
Publisher | Google Scholor - Takeuchi S, Takasato Y, Masaoka H, Hayakawa T, Yatsushige H, Shigeta K, Nagatani K, Otani N, Nawashiro H and Shima K. (2013). Decompressive craniectomy with hematoma evacuation for large hemispheric hypertensive intracerebral hemorrhage. In Brain Edema. 277-279.
Publisher | Google Scholor - Bösel J, Zweckberger K and Hacke W. (2015). Hemorrhage and hemicraniectomy: refining surgery for stroke. Current opinion in neurology. 28(1):16-22.
Publisher | Google Scholor - Pedro K.M, Chua A.E and Lapitan M.C.M. (2020). Decompressive hemicraniectomy without clot evacuation in spontaneous intracranial hemorrhage: A systematic review. Clinical neurology and neurosurgery. 192:105730.
Publisher | Google Scholor - Kim D.B, Park S.K, Moon B.H, Cho B.R, Jang D.K and Jang K.S. (2018). Comparison of craniotomy and decompressive craniectomy in large supratentorial intracerebral hemorrhage. Journal of Clinical Neuroscience. 50:208-213.
Publisher | Google Scholor - Musallam KM, Tamim HM, Richards T, Spahn DR, Rosendaal FR, Habbal A, et al. (2011). Preoperative anaemia, and postoperative outcomes in non-cardiac surgery: a retrospective cohort study. Lancet. 378:1396-1407.
Publisher | Google Scholor - Maira G, Anile C, Colosimo C, Rossi GF. (2002). Surgical treatment of primary supratentorial intracerebral hemorrhage in stuporous and comatose patients. Neurol Res. 24:54-60.
Publisher | Google Scholor - Nishihara T, Nagata K, Tanaka S, Suzuki Y, Izumi M, Mochizuki Y, et al. (2005). Newly developed endoscopic instruments for the removal of intracerebral hematoma. Neurocrit Care. 2:67-74.
Publisher | Google Scholor - Zazulia AR, Diringer MN, Derdeyn CP, Powers WJ. (1999). Progression of mass effect after intracerebral hemorrhage. Stroke. 30:1167-1173.
Publisher | Google Scholor - Abode-Iyamah KO, Stoner KE, Close LN, DeVries Watson NA, Flouty OE, Grosland NM, Howard MA. (2018). Volume of brain herniation after decompressive craniectomy in patients with traumatic brain injury.World Neurosurg. 118:414-421.
Publisher | Google Scholor