Short Communication
Sole Epidural Anaesthesia for Patient Posted for Emergency Splenectomy with Splenic Abscess: A New Perspective
Shri Sathya Sai Medical College and RI, Sri Balaji Vidyapeeth, Ammapettai, Kanchipuram, India.
*Corresponding Author: Krishna Prasad T, Shri Sathya Sai Medical College and RI, Sri Balaji Vidyapeeth, Ammapettai, Kanchipuram, India.
Citation: Krishna P V V S, Dilip G K, Hemaa S, Prasad T K. (2024). Sole Epidural Anaesthesia for Patient Posted for Emergency Splenectomy with Splenic Abscess: A New Perspective. Clinical Case Reports and Studies, BioRes Scientia Publishers. 7(3):1-5. DOI: 10.59657/2837-2565.brs.24.193
Copyright: © 2024 Krishna Prasad T, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: October 12, 2024 | Accepted: October 29, 2024 | Published: November 05, 2024
Abstract
An emergency splenectomy is required due to sepsis spreading through the bloodstream. We would like to discuss an unusual case involving a splenic abscess in a patient with compromised cardiac function who is scheduled for the procedure.
Keywords: crystalloids; patient; Oxygen; blood; ICU
Introduction
The 65-year-old male patient arrived with a fever and intense pain in the epigastric region and left flank. Upon reaching the emergency department, he was found to be sweating profusely and had mottled skin on his lower limbs. His temperature was 39.5 degrees Celsius; pulse probe showed a saturation of 94% at room air. His pulse rate was 119 beats per minute, and he was tachypnoeic, with a respiratory rate of 25 breaths per minute. He received treatment with intravenous piperacillin/tazobactam and gentamicin and was resuscitated with intravenous crystalloid fluids. An emergency laparotomy was performed, which revealed a primary splenic abscess. The abscess had penetrated the left side of the diaphragm and torn the capsule of the spleen, leading to pus collecting in the pelvic area. Top of Form Bottom of Form A splenectomy was carried out along with a primary repair of the left hemidiaphragm. Blood investigations are complete blood count: Hb-9.0g/dl, Total leucocyte count-14,300, Platelet count-2 lakh/mm3, Serum lactate 4mmol/L, C reactive protein 12mg/dl. The echocardiogram showed No RWMA, mild MR, Eccentric LVH, and Ejection fraction -40%. CT abdomen showing well-defined hypodense lesion with peripheral enhancement. Ascites and pleural effusion with ipsilateral raised hemidiaphragm. The patient was positioned sitting, with the area painted and draped. Using aseptic techniques, an 18 G epidural needle was inserted at the T10-T11 level to identify the epidural space via the loss of resistance technique and the hanging drop method. An epidural catheter was then placed, with its tip positioned at the T7 level. A test dose of 3 mL of 2% lignocaine was administered to confirm catheter placement. Additionally, 1 mg of intravenous midazolam, 30 mcg of intravenous fentanyl, and 50 mg of intravenous ranitidine were given. Oxygen supplementation was provided through a Hudson mask. The initial dose of 5 mL of 0.5% ropivacaine, combined with 3 mL of 2% ligno-adrenaline and 20 mcg of fentanyl, was administered 5 minutes after the test dose. Once the block was confirmed to range from T4 to T12, the surgery began, and a nasogastric tube was inserted. The effect of the initial dose lasted for 45 minutes. Epidural bolus of 5 mL of 0.5% ropivacaine were given at one-hour intervals, twice. Subsequently, 6 mL of 0.2% ropivacaine was administered every 30 minutes, with a maximum dose of 24 mg. Surgical site muscle relaxation was adequate. Pulse rate, arterial blood pressure, ECG, and SpO2 were continuously monitored and recorded every 3 minutes throughout the 4-hour surgery. The patient's vital signs remained stable during the procedure, and ABG measurements indicated normal acid-base status. The patient received blood products like 3 units of fresh frozen plasma and 1 unit of packed red blood cells after the splenic vessels were clamped, along with a total of 1500 mL of crystalloids. The total blood loss was 500 ml, with a urine output of 400 ml. The intraoperative temperature ranged from 35°C to 35.5°C. In the intensive care unit, a Dexmedetomidine infusion at 0.5 mcg/kg/min was initiated to enhance pain management. The epidural catheter was removed on POD 4 and the patient was discharged on POD 7. While epidural anaesthesia is typically the standard for managing pain in post-laparotomy patients, patient-controlled analgesia with opioids is also a viable alternative. Due to ongoing pain, an infusion of fentanyl was initiated, along with paracetamol and gabapentin for additional pain relief.
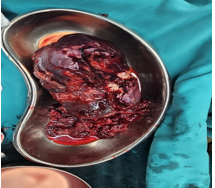
Figure 1: Excised Specimen of Spleen
Figure 2: Ct Abdomen Showing Splenic Abscess
sum
A definitive diagnosis of the case was not made clinically or radiologicallyTop of FormBottom of Form until the primary splenic abscess was discovered during laparotomy. The patient was successfully treated with a combination of surgery (including splenectomy and surgical drainage), antimicrobial therapy, and ICU care during the perioperative period, following 'gold standard' recommendations. Epidural anesthesia was selected for this patient primarily due to his bronchial asthma and poor cardiac reserve.
Conclusion
We emphasize the difficulties in diagnosis along with the complexities and the need for a multidisciplinary approach to its treatment.
References
- Myatra SN, Kothekar A, Siddiqui SS, Divatia JV. Central neuraxial blockade for splenectomy in myeloproliferative disease: A word of caution. Indian J Anaesth [Internet]. 2015 [cited 2024 Aug 16];59(10):670.
Publisher | Google Scholor - Hutton M, Brull R, Macfarlane AJR. Regional anaesthesia and outcomes. BJA Educ [Internet]. 2018;18(2):52–6.
Publisher | Google Scholor - Qu Y, Ren S, Li C, Qian S, Liu P. Management of postoperative complications following splenectomy. Int Surg [Internet]. 2013 [cited 2024 Aug 16];98(1):55–60.
Publisher | Google Scholor