Case report
Scrotal Cavernous Haemangioma: A Case Report
- Pranshu Saxena *
- Praveen Kumar
1Department of Information Technology, ABES Engineering College, Ghaziabad, India.
2Pediatric Specialist, ESIC hospital, Delhi, India.
*Corresponding Author: Pranshu Saxena, Department of Information Technology, ABES Engineering College, Ghaziabad, India.
Citation: Saxena P., Kumar P. (2023). Scrotal Cavernous Haemangioma: A Case Report. Clinical Case Reports and Studies, BioRes Scientia Publishers. 3(2):1-3. DOI: 10.59657/2837-2565.brs.23.064
Copyright: © 2023 Pranshu Saxena, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: August 14, 2023 | Accepted: August 28, 2023 | Published: September 04, 2023
Abstract
A case of scrotal hemangioma in a 21-month-old boy is described. There is evidence of a well-defined heterogeneously hypoechoic mass arising from the anterior-inferior aspect of the scrotal sac in the midline since birth. Mild vascularity is noted when tested on the colour doppler. The mass Lesion is well separated from the bilateral testicles. The mass lesion showed features of benign hemangioma.
Keywords: haemangioma; scrotal; hypoechoic mass lesion; cavernous; vascularity
Case Report
A 21-months-old boy has a dark reddish colour mass over the scrotal area, inline more over the left side and encroaching over the right side. Mass lesions are present since birth and gradually increase in size. On scrotal ultrasonography examination, the enlargement measured (2.5×1.3 cm) at seven months of age (figure 1(a)) was firm in consistency, non-tender, and well separated from bilateral testicles. The left testis (1.3×0.75 cm)and Right testis (1.2×0.9 cm)are measured in size. The shape and echotexture of both testicles are normal, no focal lesion is seen, and no free fluid is seen between layers of tunica vaginalis. There was no evidence of trauma or any other disease in the past. The baby was born healthy after 38 months of pregnancy, and the birth weight was 2.95 kg. Recent history suggests discomfort and hardness in the scrotal region. Doctors suggest not operating immediately and prescribing some medicine/ointment treatment and follow-up check-ups. Again, at the age of 21 months, the boy was brought to the hospital with a complaint of a reddish bogy mass in the midline of the scrotum, more on the left side. Initially, the swelling was small in size and, with age encroaching on to the right side. There is no history of bleeding/sudden increase in size/change in consistency.
(a) (b)
Figure 1: (a) Clinical image showing Scrotal Swelling at the age of seven months
(b) Clinical image showing Scrotal Swelling at the age of 21 months.
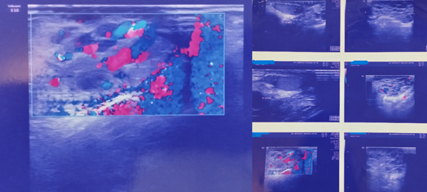
Repeat USG (figure 1(b)) of the scrotum showed evidence of a heteroechoic cystic lesion arising from the scrotal wall almost in the midline, seen separately from both the testes, cystic Lesion, measuring approx.* 3.8 × 2.0 cms. The Lesion appears highly vascular, with low flow seen within the cystic spaces (figure 2 (a)). The Lesion is likely to be benign, with the possibility of it being a vascular malformation is likely (in conjunction with a history of the Lesion being congenital). The left testis (1.38×0.67 cm)and the Right testis (1.06×0.89 cm)are measured in size. The boy had been advised to Tab. propranolol and timolol. There is a recent history of discomfort and an increase in the hardness of the swelling. He is now being admitted for further surgical evaluation and management.
(a) (b)
Figure 2: USG Study, (a) low blood flow seen within cystic spaces (b) USG image showing the position of the testis, EPIDI, and imagery view of extra testicular swelling.
Before being posted for surgery, the physical examination of the baby was as follows; pulse was 100/minute, BP: 90/60, temperature: 37 degrees C, weight: 10 kg, followed by some general examination, boy was conscious, playful, afebrile, no pallor, icterus, clubbing, cyanosis, lymphadenopathy oredema. Systemic examination shows RS- chest clear bilaterally, air entry equal, no crepitations or wheeze, CVS, sounds normal, and no murmur heard. Physical examination shows the abdomen is soft, not tender, and not distended; no hepatosplenomegaly. Bowel sounds are normal. B/L kidneys and bladder not palpable. L/E: A well-localized cystic swelling in the scrotum- more towards the left side, separate from the testes-narrow. No ulceration, no sign of inflammation/change in colour/bleeding/or any other discharge.
The boy was posted for surgery and excision of scrotal haemangioma under GA. Haemostasis was achieved by an incision around the Lesion and excised, taking the scrotal skin as the margin. Closure in layers is done by Fat-Vicarly 5/0, and the skin is closed with interrupted mattress- Vicryl Rapide 5/0. Finally, the dressing is done. (Figure 3) The excised tissue was sent for histopathological study for confirmation.
Figure 3: Post-operation Imaginary
Gross Description of Scrotum shows a single skin-covered tissue piece measuring 3 × 2.0 × 1.5 cm. The skin surface shows a congested lesion measuring 2.5×1 cm. The cut surface is haemorrhagic and congested, showing tiny cystic spaces filled with blood clots. The specimen is unoriented, and the base is not identified grossly. The rest of the cut surface is congested. Microscopic examination suggests that the section from the scrotal skin shows the epidermis and dermis. The dermis shows thin-walled dilated vascular channels of varying sizes. Few of the channels are congested, and few show the presence of fresh and organized thrombus. Histopathological diagnosis suggests Cavernous Haemangioma with fresh and organizing thrombus.
Discussion
Not many studies in the literature describe penile haemangiomas [6]. Froehner and Tsatalpas [5] have documented a giant penile cavernous haemangioma with intrapelvic extension. Deepak and Anita [1] reported a case study of a mixed variant of capillary and cavernous haemangioma in a 14 years old boy. According to Nouira et al., [4], a case with several haemangiomas of the scrotum, perineum, and pelvis coupled with a giant penis and related to agenesis of the corpus spongiosum has been recorded. The finding reported in the present instance are comparable to those seen in the example discussed by the authors above. Scrotal cavernous haemangioma often first appears in children. A diagnostic and treatment problem may arise from a subcutaneous scrotal-perineal haemangioma that resembles an inguinal hernia [7]. The heat produced by a large scrotal haemangioma is thought to cause testicular injury in some cases [3]. Imaging can be used to check the haemangioma’s size and look for any related abnormalities. The most common radiography finding is a soft tissue mass or prominence containing phleboliths (small calcifications). Phleboliths strongly indicate the presence of a cavernous haemangioma [2, 3]. Typically, simple radiography or CT scans are better at displaying phleboliths.
Cavernous haemangiomas may look hyperechoic or hypoechoic in ultra-sonographic images depending on the Lesion’s composition (such as septa, blood-containing units). Phleboliths can be observed as echogenic foci with acoustic shadowing at their distal ends. The presence of these lesions cannot be ruled out in the absence of blood flow, as shown by the color doppler within these lesions [8]. Using CT and MRI, these lesions can be easily identified; their extent can be defined. These imaging methods are thus the ones to use for this problem and are thoughts to be necessary before any surgical operations are performed [2]. A soft tissue mass containing phleboliths is seen on CT images. They appear as nodular wall thickening with phleboliths in the rectum and sigmoid. Haematuria may result from urinary bladder involvement. The Lesion has a non-homogeneous, light to strong enhancement on the postcontrast image. Selective arteriography may find the lesions, but its value for diagnosis is minimal. Due to the existence of thrombosis in dilated vascular spaces inside the haemangioma, it also shows normal outcomes in the majority of patients. Recently, it has been proposed that radionuclide tests, particularly Tc-99 scans, may be useful in determining how far these lesions have spread [2]. Elimination of the Lesion should be advised when a diagnosis has been made. A sclerosing agent, such as alcohol, surgery, or laser therapy, is available as treatment. According to one study, laser therapy had a 92.8 percent success rate with a low risk of acute complications (around 3.57 percent), which included little to no scarring and deformity. There was no long-term side effect of laser treatment. According to the study, these lesions respond well to laser therapy and encounter relatively few problems. Surgery and other therapy forms have a greater complication rate, offer equal or less effective results, and are not necessarily as effective. In some circumstances, laser therapy may be the preferred form of treatment.
Declarations
Acknowledgment
Thanks to Prof (Dr) Satish Agarwal (Paediatric Surgery), Dr Natasha Kacher (Radiologist), and Dr Pallav Gupta (Pathologist) for valuable support in carrying out this research work.
Financial or Other Competing Interests
None
References
- Deepak Chavan and Anita P Javalgi. (2014). Scrotal Haemangioma: A Case Report. J Clin Diagn Res., 8(12).
Publisher | Google Scholor - D Hervias, JP Turrion, M Herrera, et al. (2004). Diffuse cavernous haemangioma of the rectum: an atypical cause of rectal bleeding. Rev Esp Enferm Dig. 2004;96(5):346-352.
Publisher | Google Scholor - M Gotoh, S Tsai, T Sugiyama, K Miyake, H Mitsuya. (1983). Giant scrotal haemangioma with azoospermia. Urology. 1983;22(6):637-639.
Publisher | Google Scholor - Y Nouira, I Kbaier, F Attyaoui, E Menif, A Horchani. (2001). Megapenis associated to corpus spongiosum agenesis with Scrotal and Pelvic Haemangiomas. Eur Urol., 40(5):571-574.
Publisher | Google Scholor - M Froehner, P Tsatalpas. (1999). Giant penile cavernous haemangioma with intrapelvic extension-review of the literature. Urology. 1999;53(2):414-415.
Publisher | Google Scholor - Y Lin, GH Sun, DS Yu, et al. (2002). Intrastromal haemangioma. Arch Androl., 48(4):259-265.
Publisher | Google Scholor - FA Ferrer, PH McKenna. Cavernous haemangioma of the scrotum: a rare benign genital tumour of childhood. J Urol. 1995;153(4):1262-1264.
Publisher | Google Scholor - LJ Yeoman, D Shaw. (1989). Computerized tomography appearances of pelvic haemangioma involving the large bowel in childhood. PediatrRadiol, 19(6-7):414-416.
Publisher | Google Scholor