Case Report
Screening of Cervical Cancer Uptake and Associated Factors Among Women Aged 30-49 Years Old at Public Health Facilities of Kellam Wollega Zone, Western Ethiopia, 2023
1Department of Public Health, Institute of Health Science, Dambi Dollo University, Dambi Dollo, Ethiopia
2Department of Midwifery, Institute of Health Science, Dambi Dollo University, Dambi Dollo, Ethiopia
3Technical Advisor, Maternal and Child Health Directorate, Federal Ministry of Health, Addis Ababa, Ethiopia.
*Corresponding Author: Gadisa Fitala Obssie, Department of Public Health, Institute of Health Science, Dambi Dollo University, Dambi Dollo, Ethiopia
Citation: Obssie G.F., Mojo E.B., Ayele H.M. (2024). Screening of cervical cancer Uptake and associated factors among women aged 30-49 years old at public health facilities of Kellam Wollega zone, western Ethiopia, 2023. Clinical Case Reports and Studies, BioRes Scientia Publishers. 6(6):1-09. DOI: 10.59657/2837-2565.brs.24.166
Copyright: © 2024 Gadisa Fitala Obssie, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: July 26, 2024 | Accepted: August 20, 2024 | Published: September 02, 2024
Abstract
Background: The second most common cancer affecting women’s lives is cervical cancer. Globally, it causes many thousands of deaths annually among women. If women are screened for cervical cancer once in their life between the age of 30 and 49 years old, the chance of obtaining cervical cancer will be decreased by 25–36%. However, including Ethiopia, the coverage of cervical cancer screening is restricted in low and middle-income countries. Therefore, this study goes to assess cervical cancer screening uptake and associated factors among women aged 30-49 years old at public health facilities of Kellam, Wellega zone, Oromia regional state, western Ethiopia, 2023.
Objective: To assess screening of cervical cancer uptake and associated factors among women aged 30-49 years old at public health facilities of Kellam Wollega Zone, Oromia regional state, western Ethiopia, 2022.
Methods: A facility-based cross-sectional study was conducted at the public health facilities of Kellam Wollega zone, western Ethiopia, from February 1 to 30, 2023. The total sample size for the study was 451. A systematic random sampling method was applied to select study participants. Variables with P-value < 0.05 in the multiple binary logistic regression model were used to declare statistical significance. An odds ratio with a 95% confidence interval was used to show the strength of the association.
Result: Of all respondents; screen uptake was 20.6% (table 2). Multiple binary logistic regression analysis found that good knowledge (AOR=2, 95% CI:0.6,7.9), higher self-efficacy (AOR=3.3, 95% CI: 1.2,9.8), good perceived benefit (AOR=6.2, 95% CI: 2.6,14.9), urban residency (AOR=5.8, 95% CI: 2.5,13) and having above five family size (AOR=5.7, 95% CI: 2.4,13) were significantly associated with cervical cancer screening uptake (Table 3).
Conclusion: The proportion (20.6%) of cervical cancer screening uptake in the Kellam Wollega zone was low compared to the national target of above 80%.
Keywords: visual inspection of acetic acid; cervical cancer; screening; uptake; acceptability dambi dollo; ethiopia
Introduction: Background
Cervical cancer is caused by the Human papilloma Virus (HPV). This virus is passed from one person to a different throughout sex. Most sexually active individuals can have HPV at some point in their lives, however, few women can get cervical cancer [1]. It's the fourth most typically diagnosed cancer among females with 570,000 new cases and 311,000 deaths worldwide. Eighty-fifths of this occurred in developing countries [2]. The best incidence rate area unit in Southern, Eastern, and Western Africa also as South-Central Asia and South America. In Ethiopia, cervical cancer becomes the leading cause of death among females with 6294 new cases and 4884 deaths [2]. World Health Organization (WHO) developed a comprehensive approach to intervening and managing cervical cancer[3]. The first intervention was through the human papillomavirus vaccine [4] and visual inspection with acetic acid was the secondary intervention for cervical cancer [5, 6]. The program targets women aged 30-49 unless HIV-positive [7]. Once a lady is endorsed to ascertain and treat programs, acetic acid [3%–5%] is applied to the cervix. The cervix is visually inspected with acetic acid [VIA] and if the Aceto white lesion area unit is noted, she is going to be offered cryotherapy treatment in real-time [3]. Currently, VIA screening of cervical cancer is that the suggested technique in African countries [7]. The Ethiopian Federal Minister of Health (EFMOH] has developed a national cancer management setup enforced from 2016–2020 considering cervical cancer a priority cancer for intervention. The set-up targeted to launch of an HPV vaccination demonstration program and achieve 80% of girls within the target population and 80% coverage of VIA among target women by 2020 [7]. However, the screening coverage in African countries is just too low and its only 2.9% in 2017 [8]. Anticipated high price of the take, look at, spiritual denial, husband approval, anticipated long waiting time, fear of test outcome, Poor training experience, poor knowledge regarding cervical cancer screening, unskilled health care supplier, long distance from health establishments and a female provider determining women’s cervical cancer screening acceptance [11-14]. Therefore, this study assesses cervical cancer screening uptake and associated factors among women aged 30-49 in Kellam Wollega zone public health facility, Western Ethiopia, 2022.
Methods
Study design and set up
The facility-based cross-sectional study was conducted at selected public health facilities within the Kellam Wellega zone from February 01 to 30, 2022. The zone is found 652 kilometers from Addis Ababa, the capital city of Ethiopia. From a total of 55 health facilities, only 9 have been providing cervical cancer screening using visual inspection of the cervix with acetic acid.
Sample Size Determination and Sampling procedure
The study’s sample size was calculated using Epi-info version 7 software and the single population proportion formula. The subsequent assumptions were used; 10% proportion of cervical cancer screening service uptake [15], 95% Confidence level, 80% power, a d a 5% margin of error. Finally, the sample sizes become 451 after adding a 10% contingency for possible nonresponse and 1.5 as a design effect. The samples were selected randomly from the list of all health facilities providing cervical cancer screening using a visual inspection of the cervix with acetic acid in the zone using a simple random sampling technique.
Data collection tools, and quality assurance
A structured, interviewer-administered questionnaire was used to collect the data. The questionnaire was first prepared in English, translated into the local language (Afan Oromo) to ensure consistency. The questionnaire was pretested on 5% of the total sample size 5 days before the actual data collection day among women aged 30-49 years old at Keto health center which has VIA. Amendments were taken to some questionnaires. Fifteen experienced data collectors were recruited and collected the data for one month after they received three days of training.
Result
Socio-demographic characteristics of respondents
Respondents’ mean age was 37 years old with a standard deviation 5. Respondents who participated in the study were females. Of the whole respondents, 398 (88.2%) respondents’ marital status was married. Similarly, 302 (67%) of the participants were Oromo in ethnicity and 305 (67.6%) of the respondents were protestant in religion. The study postulated that 121(26.8%) and 84(18.6) of the respondents were unable to read and write & able to read and write in educational status, respectively, and 270(59.9%) of the respondents’ occupations were housewives. Likewise, the study documented that 283(62.7%) of the participants had less than 1500 income ETB, and about 374 (82.9%) of the participants had 0-5 family size (Table 1).
Table 1: Sociodemographic characteristics of respondents in Kellam wollega zone, Oromia, western Ethiopia, 2022.
| Variables | Frequency | Percentage |
| Age | ||
| 30-34 | 181 | 40.1 |
| 35-39 | 146 | 32.4 |
| 40-44 | 70 | 15.5 |
| 45-49 | 54 | 12 |
| Residence | ||
| Urban | 262 | 58.1 |
| Rural | 189 | 41.9 |
| Marital status | ||
| Married | 398 | 88.2 |
| Widowed | 33 | 7.3 |
| Divorced | 13 | 2.9 |
| Single | 6 | 1.3 |
| Others | 1 | 0.2 |
| Ethnicity | ||
| Oromo | 302 | 67 |
| Gambela | 6 | 1.3 |
| Amhara | 51 | 11.3 |
| Gurage | 43 | 9.5 |
| Silte | 42 | 9.3 |
| Others | 7 | 1.6 |
| Religion | ||
| Protestant | 305 | 67.6 |
| Orthodox | 79 | 17.5 |
| Muslim | 45 | 10 |
| Catholic | 6 | 1.3 |
| Apostle | 16 | 3.5 |
| Educational status | ||
| unable to read and write | 121 | 26.8 |
| able to read and write | 84 | 18.6 |
| primary education | 83 | 18.4 |
| secondary education | 69 | 15.3 |
| Certificate | 27 | 6 |
| Diploma | 32 | 7.1 |
| degree and above | 35 | 7.8 |
| Occupation | ||
| Housewife | 270 | 59.9 |
| Merchant | 65 | 14.4 |
| Daily laborer | 31 | 6.9 |
| government employee | 40 | 8.9 |
| Student | 14 | 3.1 |
| private employee | 19 | 4.2 |
| Others | 12 | 2.7 |
| Family size | ||
| 0-5 | 374 | 82.9 |
| 6-10 | 77 | 17.1 |
| Monthly income of the head by ETB | ||
| <1500> | 283 | 62.7 |
| 1500-3000 | 87 | 19.3 |
| 3000-4500 | 23 | 5.1 |
| 4500-6000 | 28 | 6.2 |
| 6000-7500 | 13 | 2.9 |
| ≥7500 | 17 | 3.8 |
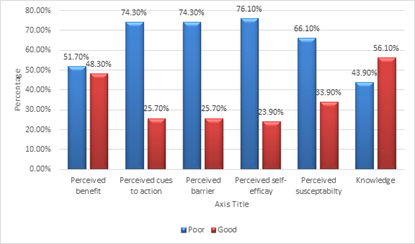
Perception and knowledge of respondents about cervical cancer and screening
Of a total of 451 respondents, 198 had poor knowledge, 253 had good knowledge, 233 had the poor perceived benefit, and 218 had good perceived benefit about perception and knowledge on cervical cancer and screening (figure 1).
Figure 1: Perception and Knowledge of respondents about cervical cancer and screening in Kellam wollega zone, Oromia, western Ethiopia, 2022.
Cervical cancer screening uptake by respondents
From a total of 451, only 93 respondents were screened which gives a screen uptake of 20.6 %. Of a total of 93 screened respondents, 79 were negative and 14 of them were positive for the pre-cancerous lesion (Table 2).
Table 2: Cervical cancer screening uptake by respondents in Kellam wollega zone, Oromia, western Ethiopia, 2022.
| Variables | Yes | No | ||
| Frequency | Percentage | Frequency | Percentage | |
| Cervical cancer screening uptake | 93 | 20.6 | 358 | 79.4 |
| Yes | ||||
| Result | Positive | Negative | ||
| 14 | 3.1 | 79 | 17.5 | |
Factors significantly associated with screening of cervical cancer acceptance by respondents in Kellam wollega zone, Oromia, western Ethiopia, 2022.
Multiple binary logistic regression analysis found that good knowledge (AOR=2, 95% CI:0.6,7.9), higher self-efficacy (AOR=3.3, 95% CI: 1.2,9.8), good perceived benefit (AOR=6, 95% CI: 2.6,14.9), urban residency (AOR=5.8, 95% CI: 2.5,13) and having above five family members (AOR=5.7, 95% CI: 2.4,13) were significantly associated with cervical cancer screening uptake (Table 3).
Table 3: Factors associated with cervical cancer screening uptake in Kellam wollega zone, Oromia, western Ethiopia.
| Variables | Cervical screening uptake | ||
| Yes n (%) | No n (%) | AOR (95% CI) | |
| Residence | |||
| Urban | 70 | 192 | 5.78(2.54, 13.17) * |
| Rural | 23 | 166 | 1 |
| Family size | |||
| 0-5 | 58(49.7) | 296(50.3) | 5.66(2.36, 13.56) * |
| 6-10 | 35(46.5) | 62(53.5) | 1 |
| Perception | |||
| Poor Perceived benefit | 23(49) | 194(51) | 1 |
| Good Perceived benefit | 70 | 164 | 6.2(2.58, 14.91) * |
| Poor Perceived self-efficacy | 54(28) | 289(72) | 1 |
| Good Perceived self-efficacy | 39 | 69 | 3.33(1.13, 9.84) * |
| Knowledge about Cervical cancer | |||
| poor knowledge | 25(53) | 167(47) | 1 |
| good knowledge | 68(32) | 191(68) | 2(0.55, 7.94) * |
*Statistically Significant at P less than0.05
Discussion
WHO recommends screening for all women aged thirty to forty-nine years to spot the metastatic tumor lesion. Eighty percent of cervical cancers are often prevented if early treated and screened [16]. The finding of this study is 20.6%, which is below the national target of 80% of cervical cancer screening [17].
The result of this study were below the study findings in Canada 58% [18], England 85.7% [19], Catalonia 50.6% [20] and Republic of Kenya 46% [21]. Variations within the socio-demographic and economic status of the study respondents furthermore because the countries’ health policies may be the potential reason for this variation. For example, in Canada, screening utilization can be multiplied as even distribution of screening service centers and universal access to health care is obtainable. However, in Ethiopia, since the cervical screening service was initiated a few years back, the cervical cancer screening activities area units distended at a restricted variety of health establishment, and furthermore as continuous and arranged health education and awareness creation programs do not seem to be well established [22]. The distinction might be partly justified by the time gap between the studies, furthermore because the study space may be completely different among the studies. [23].
The finding of this study is higher than the study conducted in Ghana 2.4% [24], Nigeria 8%, Uganda 4.8% [25]and 17.5% Kenya [13]. This may be because of socio-demographic characteristics and the time gap between the studies, furthermore because the study area may be totally different between the studies [23]. Additionally, it may be because of variations in countries’ promotional policies, increased nationwide support, and media concern [26]. For example, the reason for the low coverage of cervical cancer screening services in Ghana may be there is still no national policy or program concerning cervical cancer screening which may well be causative to the low screening of cervical cancer in Ghana. Currently, in Federal Democratic Republic of Ethiopia, the growth of cervical cancer screening service centers was done. Associate in Nursing integration of services with the delivery case team at the health center level, making awareness for health extension workers and health development army to activate the community for cervical cancer screening service uptake were additionally done by the government.
The results of this study were higher than the study findings at the national level of 2.9% [27], meta-nalysis study in Ethiopia 18.17% [17], 16.4% in Gondar [28], 10% in Gondar [26], 10.6% in Addis Ababa [29]], SNNPR 18.59%, Oromia 16%, Tigrai 15.41%, Addis Ababa 14.32%, Amhara 13.62%, Dessie 11% [30], Arbaminch 5.9% [[31], Dessie and Mekele towns 20% [[32]. The uptake report from these studies was supported by retrospective assessment, not once invited and a few studies were from HIV clinics alone. For example, the previously conducted study in Gondar targeted to HIV-positive women who visited the referral hospital compared to the present study, including women regardless of HIV status attending health facilities and hospitals along. Thus, the exaggerated uptake discovered within the current study may be as a result of the recent replacement of VIA screening at the health center level within the town, that is nearer to the partakers than wherever it had been only at the hospital level. Moreover, eligible women were actively requested and offered VIA screening within the current study compared to the previous studies. This might need helping women to simply establish and access the service and utilize it consequently. Current cervical cancer interference promotion programmed spread throughout the country and there are sensitization implementation activities, which can lead to higher uptake in our study.
The results of this study were lower than the study findings in Debremarkos town, 21% [23]. This distinction may be due to variations in population characteristics and study settings. It may be attributed to the inadequate number of health facilities that give cervical cancer screening services, health-seeking behavior of the study participants, and knowledge of the women of the preventive measures for cervical cancer [33].
The higher odds of cervical cancer screening uptake were determined among respondents who had good knowledge. The odds of cervical cancer screening uptake were about two times more likely among women who had good knowledge in comparison to women who had poor knowledge regarding cervical cancer screening uptake. The result's supported by studies done in Tanzania [34], Botswana [35], and China [35]. The possible reason may be explained by the fact that the rise of women’s knowledge regarding cervical cancer and screening benefits directly leads women to utilize the screening service. This finding is comparable to alternative previous studies [19, 29, 36]. Women’s having good knowledge regarding the severity and risk factors of cervical cancer will have higher health-seeking behavior, in order that they will utilize screening services for cervical cancer uptake. This study is consistent with studies in developing countries normally wherever knowledge of cervical cancer and screening is poor.
Women who have a good perceived benefit about cervical cancer screening uptake were about 2 times more likely to undergo screening in comparison to their counterparts. This result is similar to the findings of a study in Uganda [37]. This was consistent with the hypothesis of the health belief model that state that perceived severity and therefore the threat of cervical cancer, perceived benefit, perceived self-efficacy, and net benefit about the preventive action of cervical cancer screening necessitates individuals to have an interaction with preventive actions like cervical cancer screening service uptake [38]. Similarly, it might be explained by women’s view of cervical cancer screening benefits. If they perceive that they are benefiting from cervical cancer screening, they look for screening and treatment to safeguard themselves.
The odds of cervical cancer screening uptake were about 3 times more likely to undergo cervical cancer screening among higher self-efficacy women compared to their counterparts. This is consistent with the study done in Bishoftu, East Shoa [38], Nigeria [39], and Gonder [26] reported that the confidence of women concerning screening resulted in increased screening uptake. This may be because of developing confidence through information dissemination for cervical cancer screening.
The odds of cervical cancer screening uptake were about 6 times more likely to occur among women living in urban compared to women living in rural. This study is in line with the studies done in Ethiopia [8] and Kenya [21]. This may be because of the high coverage of mass media and health facilities in urban compared to rural.
The odds of cervical cancer screening uptake were about 6 times more likely to occur among women who have above five family numbers compared to their counterparts. The probability of cervical cancer screening uptake is increasing as family size will increase. This is often may be as a result of as family size will increase, they will be multipara so that they would possibly visit a hospital.
Strength of the study
This study reflects a real-life observe and results of the VIA approach presently enforced by the Ethiopian Federal Ministry of Health during which women’s visiting a health facility for routine services were invited and uptake was measured. We tend to postulate that this magnitude of uptake throughout one visit is representative of the strategy while not extra campaigns.
Limitations of the study
Since the study was cross-sectional, the temporal -cause-effect relationship may not be well addressed.
Conclusions and Recommendations
The proportion (20.6%) of cervical cancer screening uptake in the Kellam Wellega zone was low compared to the national target which is above 80%. Good knowledge, higher self-efficacy, good perceived benefit, urban residency, and above five family size were significantly associated with cervical cancer screening uptake in the Kellam Wellega zone. Therefore, to extend the uptake of cervical cancer screening among age-eligible women, it is better to form awareness programs for early detection and treatment of cervical cancer, and promotion through the mass media, and health talks concerning cervical cancer screening, and therefore the obtainable facilities. Timeserving screening in health facilities may be promoted to boost cervical cancer screening uptake for all age-eligible women. Moreover, to push cervical cancer screening, it is better to integrate cancer management programmers into existing primary sexual and generative health care services, strengthen multi-sectoral collaboration, and improve public health awareness to tackle the devastating impact of cervical cancer. its additionally vital to tell that each woman is liable to cervical cancer, particularly when beginning gender, and screening remains elementary within the fight against cervical cancer before turning into invasive or dead. Health acquisition that teaches in small stages, the application of cervical screening to push favorable attitudes towards screening and boost women's confidence to endure screening is additionally counseled. Therefore, ladies management, rising information towards cervical cancer screening, enhancing perceived susceptibleness and severity to cancer, and characteristic history of ladies area unit are essential methods to boost cervical cancer screening of ladies’.
Declarations
Acknowledgments
The authors would like to thank all respondents for their willingness to participate in the study.
Competing interests
No conflicts of interest in this work among authors.
Ethics approval and consent to participate
All methods of this study were carried out under the Declaration of Helsinki’s ethical principle for medical research involving human subjects. Ethical approval to conduct this study was obtained from the ethical review committee of Dambi Dollo University (Ref. No: DaDURE/004/21). An offial letter was sent to the Kellam Wollega zonal health office. Permission letter was delivered to woreda health office. Then, woreda health office sent supportive letter to respective public health facilities. For un educated participants informed consent was obtained from their parents or friends and for educated participants it was taken from participants themselves. Confidentiality and privacy of the information was maintained. The participants were informed that participation is voluntary.
Publication consent
All authors of the study were agreed to publish the study on Pub Med journal. Publication consent was obtained from publication office of Dambi Dollo Univesity after reviewing the mother document.
Availability of Data
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Funding
Dambi Dollo University is the main source of our study fund.
Authors contribution
EB has been working on data analysis and writing up the final results, HM has been working on proposal preparation and GF has been working on overall activities.
References
- Saslow, D., Castle, P. E., Cox, J. T., Davey, D. D., Einstein, M. H., Ferris, D. G., & others. (2007). American Cancer Society guideline for human papillomavirus (HPV) vaccine use to prevent cervical cancer and its precursors. CA: A Cancer Journal for Clinicians, 57(1):7-28.
Publisher | Google Scholor - Bray, F., Ferlay, J., Soerjomataram, I., Siegel, R. L., Torre, L. A., & Jemal, A. (2018). Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA: A Cancer Journal for Clinicians, 68(6):394-424.
Publisher | Google Scholor - World Health Organization. (2006). Comprehensive cervical cancer control: A guide to essential practice. World Health Organization.
Publisher | Google Scholor - Romanowski, B., Schwarz, T. F., Ferguson, L. M., Peters, K., Dionne, M., Schulze, K., & others. (2011). Immunogenicity and safety of the HPV-16/18 AS04-adjuvanted vaccine administered as a 2-dose schedule compared to the licensed 3-dose schedule: Results from a randomized study. Human Vaccines, 7(12):1374-1386.
Publisher | Google Scholor - Kunckler, M., Schumacher, F., Kenfack, B., Catarino, R., Viviano, M., Tincho, E., & others. (2017). Cervical cancer screening in a low-resource setting: A pilot study on an HPV-based screen-and-treat approach. Cancer Medicine, 6(7):1752-1761.
Publisher | Google Scholor - Shiferaw, N., Salvador-Davila, G., Kassahun, K., Brooks, M. I., Weldegebreal, T., Tilahun, Y., & others. (2016). The single-visit approach as a cervical cancer prevention strategy among women with HIV in Ethiopia: Successes and lessons learned. Global Health: Science and Practice, 4(1):87-98.
Publisher | Google Scholor - Federal Ministry of Health Ethiopia. (2015). National Cancer Control Plan 2016–2020. Addis Ababa: Disease Prevention and Control Directorate.
Publisher | Google Scholor - Gelibo, T., Roets, L., Getachew, T., & Bekele, A. (2017). Coverage and factors associated with cervical cancer screening: Results from a population-based WHO STEPS study in Ethiopia. Advances in Oncology Research & Treatment, 1(115):2.
Publisher | Google Scholor - Selmouni, F., Zidouh, A., Alvarez-Plaza, C., & El Rhazi, K. (2015). Perception and satisfaction of cervical cancer screening by visual inspection with acetic acid (VIA) at Meknes-Tafilalet Region, Morocco: A population-based cross-sectional study. BMC Women's Health, 15(1):1-6.
Publisher | Google Scholor - Belete, N., Tsige, Y., & Mellie, H. (2015). Willingness and acceptability of cervical cancer screening among women living with HIV/AIDS in Addis Ababa, Ethiopia: A cross-sectional study. Gynecologic Oncology Research and Practice, 2(1):1-6.
Publisher | Google Scholor - Ezechi, O. C., Gab-Okafor, C. V., Ostergren, P. O., & Odberg Pettersson, K. (2013). Willingness and acceptability of cervical cancer screening among HIV positive Nigerian women. BMC Public Health, 13(1):1-8.
Publisher | Google Scholor - Modibbo, F. I., Dareng, E., Bamisaye, P., Jedy-Agba, E., Adewole, A., Oyeneyin, L., & others. (2016). Qualitative study of barriers to cervical cancer screening among Nigerian women. BMJ Open, 6(1):e008533.
Publisher | Google Scholor - Morema, E. N., Atieli, H. E., Onyango, R. O., Omondi, J. H., & Ouma, C. (2014). Determinants of cervical screening services uptake among 18–49 year old women seeking services at the Jaramogi Oginga Odinga Teaching and Referral Hospital, Kisumu, Kenya. BMC Health Services Research, 14(1):1-7.
Publisher | Google Scholor - Ndejjo, R., Mukama, T., Musabyimana, A., & Musoke, D. (2016). Uptake of cervical cancer screening and associated factors among women in rural Uganda: A cross-sectional study. PLOS ONE, 11(2):e0149696.
Publisher | Google Scholor - Nega, A. D., Woldetsadik, M. A., & Gelagay, A. A. (2018). Low uptake of cervical cancer screening among HIV positive women in Gondar University referral hospital, Northwest Ethiopia: Cross-sectional study design. BMC Women's Health, 18(1):1-7.
Publisher | Google Scholor - Teame, H., Addissie, A., Ayele, W., Hirpa, S., Gebremariam, A., Gebreheat, G., & others. (2018). Factors associated with cervical precancerous lesions among women screened for cervical cancer in Addis Ababa, Ethiopia: A case-control study. PLOS ONE, 13(1):e0191506.
Publisher | Google Scholor - Dessalegn Mekonnen, B. (2020). Cervical cancer screening uptake and associated factors among HIV-positive women in Ethiopia: A systematic review and meta-analysis. Advances in Preventive Medicine, 1-12.
Publisher | Google Scholor - Leece, P., Kendall, C., Touchie, C., Angel, J., Jaffey, J., & Pottie, K. (2010). Cervical cancer screening among HIV-positive women. Canadian Family Physician, 56:425-431.
Publisher | Google Scholor - Ogunwale, A. N., Coleman, M. A., Sangi-Haghpeykar, H., Valverde, I., Montealegre, J., Jibaja-Weiss, M., & others. (2016). Assessment of factors impacting cervical cancer screening among low-income women living with HIV-AIDS. AIDS Care, 28(4):491-494.
Publisher | Google Scholor - Stuardo, V., Agustí, C., & Casabona, J. (2013). Low prevalence of cervical cancer screening among HIV-positive women in Catalonia (Spain). Journal of AIDS and Clinical Research, 5(S3).
Publisher | Google Scholor - Njuguna, E., Ilovi, S., Muiruri, P., Mutai, K., Kinuthia, J., & Njoroge, P. (2017). Factors influencing cervical cancer screening in a Kenyan health facility: A mixed qualitative and quantitative study. International Journal of Reproduction, Contraception, Obstetrics and Gynecology, 6(4):1180-1185.
Publisher | Google Scholor - Maar, M., Wakewich, P., Wood, B., Severini, A., Little, J., Burchell, A. N., & others. (2016). Strategies for increasing cervical cancer screening amongst First Nations communities in Northwest Ontario, Canada. Health Care for Women International, 37(4):478-495.
Publisher | Google Scholor - Bante, S. A., Getie, S. A., Getu, A. A., Mulatu, K., & Fenta, S. L. (2019). Uptake of pre-cervical cancer screening and associated factors among reproductive age women in Debre Markos town, Northwest Ethiopia, 2017. BMC Public Health, 19(1):1-9.
Publisher | Google Scholor - Calys-Tagoe, B. N., Aheto, J. M., Mensah, G., Biritwum, R. B., & Yawson, A. E. (2020). Cervical cancer screening practices among women in Ghana: Evidence from wave 2 of the WHO study on global AGEing and adult health. BMC Women's Health, 20(1):1-9.
Publisher | Google Scholor - Idowu, A., Olowookere, S. A., Fagbemi, A. T., & Ogunlaja, O. A. (2016). Determinants of cervical cancer screening uptake among women in Ilorin, North Central Nigeria: A community-based study. Journal of Cancer Epidemiology, 1-8.
Publisher | Google Scholor - Desta, M., Getaneh, T., Yeserah, B., Worku, Y., Eshete, T., Birhanu, M. Y., & others. (2021). Cervical cancer screening utilization and predictors among eligible women in Ethiopia: A systematic review and meta-analysis. PLOS ONE, 16(11):e0259339.
Publisher | Google Scholor - Destaw, A., Midaksa, M., Addissie, A., Kantelhardt, E. J., & Gizaw, M. (2021). Cervical cancer screening see and treat approach
Publisher | Google Scholor - Shiferaw, S., Addissie, A., Gizaw, M., Hirpa, S., Ayele, W., Getachew, S., & others. (2018). Knowledge about cervical cancer and barriers toward cervical cancer screening among HIV-positive women attending public health centers in Addis Ababa city, Ethiopia. Cancer Medicine, 7(3):903-912.
Publisher | Google Scholor - Mitiku, I., & Tefera, F. (2016). Knowledge about cervical cancer and associated factors among 15–49-year-old women in Dessie town, Northeast Ethiopia. PLOS ONE, 11(9):e0163136.
Publisher | Google Scholor - Gebru, Z., Gerbaba, M., & Dirar, A. (2016). Utilization of cervical carcinoma screening service and associated factors among currently married women in Arba Minch town, southern Ethiopia. Journal of Women’s Health Care, 5(297):2167-0420.1000297.
Publisher | Google Scholor - Bayu, H., Berhe, Y., Mulat, A., & Alemu, A. (2016). Cervical cancer screening service uptake and associated factors among age-eligible women in Mekelle Zone, Northern Ethiopia, 2015: A community-based study using the health belief model. PLOS ONE, 11(3):e0149908.
Publisher | Google Scholor - Natae, S. F., Nigatu, D. T., Negawo, M. K., & Mengesha, W. W. (2021). Cervical cancer screening uptake and determinant factors among women in Ambo town, Western Oromia, Ethiopia: Community-based cross-sectional study. Cancer Medicine, 10(23):8651-8661.
Publisher | Google Scholor - Lyimo, F. S., & Beran, T. N. (2012). Demographic, knowledge, attitudinal, and accessibility factors associated with uptake of cervical cancer screening among women in a rural district of Tanzania: Three public policy implications. BMC Public Health, 12(1):1-8.
Publisher | Google Scholor - Mingo, A. M., Panozzo, C. A., DiAngi, Y. T., Smith, J. S., Steinhoff, A. P., Ramogola-Masire, D., & others. (2012). Cervical cancer awareness and screening in Botswana. International Journal of Gynecologic Cancer, 22(4).
Publisher | Google Scholor - Leung, S. S., & Leung, I. (2010). Cervical cancer screening: Knowledge, health perception, and attendance rate among Hong Kong Chinese women. International Journal of Women’s Health, 2:221-228.
Publisher | Google Scholor - Marlow, L. A., Waller, J., & Wardle, J. (2015). Barriers to cervical cancer screening among ethnic minority women: A qualitative study. Journal of Family Planning and Reproductive Health Care, 41(4):248-254.
Publisher | Google Scholor - Solomon, K., Tamir, M., & Kaba, M. (2019). Predictors of cervical cancer screening practice among HIV positive women attending adult anti-retroviral treatment clinics in Bishoftu town, Ethiopia: The application of a health belief model. BMC Cancer, 19(1):1-11.
Publisher | Google Scholor - Arulogun, O. S., & Maxwell, O. O. (2012). Perception and utilization of cervical cancer screening services among female nurses in University College Hospital, Ibadan, Nigeria. Pan African Medical Journal, 11(1).
Publisher | Google Scholor