Case Report
Scedosporium Apiospermum Cellulitis: A Case Report
- Miauro Cynthia Victoria *
- Giraldo Cardona Joaquín
- Gonzalez Yasmin Soledad
- Zanetta Anabela
- Metta Viviana
- Buono Monica Estela
Internal Medicine, Dr B. A. Houssay Hospital, Vicente Lopez, Buenos Aires.
*Corresponding Author: Miauro Cynthia Victoria, Internal Medicine, Dr B. A. Houssay Hospital, Vicente Lopez, Buenos Aires.
Citation: Victoria M. C., Joaquín G. C., Soledad G. Y., Anabela Z., Viviana M. et al. (2024). Scedosporium Apiospermum Cellulitis: A Case Report. Clinical Case Reports and Studies, BioRes Scientia Publishers. 5(5):1-05. DOI: 10.59657/2837-2565.brs.24.123
Copyright: © 2024 Miauro Cynthia Victoria, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: March 21, 2024 | Accepted: April 10, 2024 | Published: April 25, 2024
Abstract
Scedosporium apiospermum infections are part of the low-frequency mycoses caused by emerging fungi. The natural habitat of these fungi is soil, water and decomposing organic matter. Although inhalation is the route of exposure of most concern, systemic infections secondary to ingestion, trauma or contamination of wounds by conidia or environmental sporangiospores are not uncommon. We present a case of cellulitis in a 68-year-old male patient who was admitted to our institution due to a left lower limb's soft tissue infection. Scedosporium apiospermum was reported later in cultures. Therefore, he received adjusted treatment with Voriconazole. We highlight the importance of this rare case given its low frequency and high mortality associated with its resistance to most of the available antifungals, especially in immunocompromised hosts whose prognosis will depend on rapid diagnosis and early antifungal treatment.
Keywords: scedosporium apiospermum; cellulitis; emerging mycoses; scedosporium
Introduction
Scedosporium is a genus of filamentous fungi. It originally included the species Scedosporium prolificans and Scedosporium apiospermum, which were the only known species of the genus Scedosporium (also called Lomentospora) until a few years ago. However, recent molecular studies have shown that S. apiospermum is actually a complex composed of eight species: Scedosporium boydii (Pseudallescheria boydii teleomorph), Scedosporium apiospermum (Pseudallescheria apiosperma teleomorph), Pseudallescheria ellipsoidea, Pseudallescheria angusta, Pseudallescheria fusoidea, Pseudallescheria minutispora, Scedosporium dehoogi and Scedosporium aurantiacum 8,9. Differentiation between the species of the complex is difficult and its correct identification must be done using DNA sequencing techniques [1]. Scedosporium apiospermum is a ubiquitous fungus with a worldwide distribution, that can be found in soil, potting soil, sewers, stagnant water, streams and manure [2]. Although inhalation is the route of exposure of most concern, systemic infections due to ingestion, trauma or contamination of wounds by conidia or environmental sporangiospores are not uncommon [1, 4]. Invasive systemic infections due to these fungi are diagnosed above all, in immunosuppressed patients, mostly onco-hematological, patients going under treatment with corticosteroids, recipients of hematopoietic stem cell transplant and solid organ transplant. Among these, lung transplant recipients are the most frequently affected, since patients with cystic fibrosis are usually colonized by Scedosporium before being transplanted [1].
Case Report
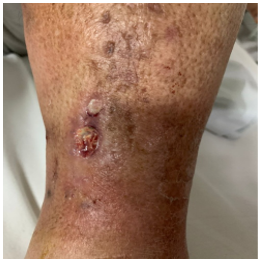
A 68-year-old male patient with a medical history of obesity, chronic obstructive pulmonary disease, arterial hypertension, systemic erythematosus lupus diagnosed in 2013, treated with prednisone 40 mg daily, Hydroxychloroquine and Cyclophosphamide, presented to our institution with progressive dyspnea and peripheral edema predominantly on the left leg. Physical examination revealed ulcerative lesions in the lower limbs with signs of phlogosis, Homan and Ollow signs were positive on the left leg as well. Relevant laboratory data included white blood cells of 14,200/mm3 with 95% polymorphonuclear, blood glucose of 226 mg/dl. A chest x-ray was performed showing signs of flow redistribution and cardiothoracic index >0.5. The patient was diagnosed with fluid overload due to clinical suspicion of acutely decompensated heart failure secondary to skin and soft tissue infection; hence empirical treatment with Ciprofloxacin and Clindamycin was initiated. During his hospitalization, diagnosis of heart failure was confirmed and specific treatment was established.
According to the high probability of venous thrombosis, a Doppler ultrasound of the lower limbs showed signs of superficial venous thrombosis in the left lower limb and an organized hypodense heterogeneous collection measuring 72x14x26 mm. A puncture sample of it was performed with culture samples taken, with a subsequent positive result for filamentous fungi compatible with Scedosporium. After these outcomes, a second sample was sent to the national institute of microbiology Dr. Malbrán for confirmation, typification and sensitivity analysis, reporting Scedosporium apiospermum with minimum inhibitory concentration of 0.25 ug/ml for Voriconazole. With these results associated with progression of ulcerative lesion, a mechanical surgical toilette was performed by Orthopedics and Traumatology service and treatment with Voriconazole 400 mg every 12 hours intravenously was indicated. Oral treatment was initiated later (Voriconazole 200 mg every 12 hours) and hospital discharge was given when clinical improvement was acknowledged, with indication of treatment for 6 months and follow-up on an outpatient basis by mycology at Muñiz Hospital.
Figure 1: Patient’s left leg showed ulcerative lesions surrounded by erythema, swelling and tenderness.
Discussion
We emphasize the relevance of this case due to its low frequency, being potentially serious and fatal infections due to its resistance to most of the available antifungals. Patient prognosis will depend on early diagnosis and antifungal treatment.
Competing interests
All authors declare that they have no competing interests.
Expression of gratitude
Infectious Disease Service, Dr Professor Bernardo Houssay Hospital
Bacteriology Service, Dr. Antonio A. Cetrángolo, Chest Hospital
References
- Pemán J, Salavert M. (2014). Invasive fungal disease due to Scedosporium, Fusarium and Mucorales. Rev Iberoam Micol., 31(4):242-248.
Publisher | Google Scholor - Centellas Pérez FJ, Martinez Antolinos C, Piqueras Sanchez S, Lorenzo Gonzalez I, Llamas Fuentes F, et al. (2019). Scedosporium apiospermum infection in a kidney transplant recipient. Rev Iberoam De Micol. 36(1):48-50.
Publisher | Google Scholor - R. San Juan, J. Berenguer, J.M. (2003). Aguado. Emerging filamentous fungi: Scedosporium. Control de Calidad SEIMC, 1-6
Publisher | Google Scholor - Pemán J, Salavert M. (2013). Epidemiology and prevention of nosocomial invasive infections by filamentous fungi and yeasts. Enferm Infecc Microbiol Clin, 31:328-341.
Publisher | Google Scholor