Research Article
Risk Factors for Seromucous Otitis in Children
1ENT and CCF service. Army Central Hospital. Algiers, Algeria.
2Faculty of Medicine, Boubenider University, Algeria.
*Corresponding Author: Mohamed Cherif, ENT and CCF service. Army Central Hospital. Algiers, Algeria.
Citation: Cherif M, Benchaoui M. (2024). Risk Factors for Seromucous Otitis in Children, International Journal of Biomedical and Clinical Research, BioRes Scientia Publishers. 1(4):1-8. DOI: 10.59657/2997-6103.brs.24.021
Copyright: © 2024 Mohamed Cherif, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: July 08, 2024 | Accepted: August 06, 2024 | Published: August 13, 2024
Abstract
Introduction: Sero-mucosal otitis (SMO) is one of the most common chronic otologic conditions of childhood, constituting the leading cause of acquired hearing loss in children. It is a pathology which is recognized as multifactorial where numerous parameters are involved in causing and perpetuating the disease. Several risk factors (more than 30) have been reported in the literature and we will look for them in our group of children with SMO.
Material and Methods: This is a prospective, descriptive study, targeting a group of 80 children, aged between 04 and 14 years old and presenting confirmed SMO, associated or not with adenoid hypertrophy (AH). This study spanned 24 months, from January 2020 to January 2022. In all of our patients, the diagnosis of OSM was confirmed. A questionnaire was sent to the children's parents, containing questions on the risk factors sought.
Results: The risk factors found in relation to SMO are: young age, promiscuity, low to medium social level, urban living environment with proximity to an industrial zone, low to medium level of education of the mother, passive smoking, recurrent VAS infections, recurrent AOM, allergy. On the other hand, co-sanguineous marriage, prematurity, stay in nurseries, gastroesophageal reflux disease (GERD) and obesity seem to have no relationship with the pathogenesis of this pathology. Sufficient breastfeeding and pneumococcal vaccination appear to be protective factors.
Discussion: Our results are quite close to those found in the international literature. It should be emphasized that the figures obtained constitute only a simple descriptive study of risk factors and only a comparative and multivariate statistical study can link one or more factors to the occurrence of OSM.
Conclusion: The analysis of the different risk factors in relation to SMO can contribute to a better understanding of this pathology and to perhaps instituting a prevention and/or screening program in the infant population.
Keywords: sero-mucosal otitis; risk factors; screening; prevention
Introduction
Sero-mucosal otitis (SMO) is one of the most common chronic otologic conditions of childhood, constituting the leading cause of acquired hearing loss in children. It is an extremely common pathology since almost all preschool children are affected by it at some point in their development. It is estimated that 80% of children have had an episode of SMO before the age of 10(1). SMO is a complex, multifactorial pathology where different processes are self-perpetuating to create the vicious circle of intra-tympanic effusion [2]. Several risk factors (more than 30) have been reported in the literature [3], the risk of occurrence does not appear to be the same for all patients. In our study, we tried to search in our study population for the majority of risk factors reported by the different authors.
Material and Methods
This is a prospective, descriptive study targeting a group of 80 children (160 ears) with confirmed seromucous otitis, associated or not with hypertrophy of the adenoids. This study spanned 24 months, from January 2020 to January 14, 2022. This study took place at the level of the ENT and CCF department of the Regional Military University Hospital of Constantine and the ENT and CCF department of the Benbadis University Hospital Center of Constantine. Children with craniofacial malformations, Down syndrome (trisomy 21), Crouzon syndrome or cleft palates are excluded, as well as SMO complicating another adjacent disease (cavum tumors, etc.), to eliminate any organic pathogenic risk factor.
A questionnaire was sent to the children's parents, including the following parameters:
Age.
Number of siblings.
Consanguineous marriage or not.
Socio-Economic Conditions
- The area and type of habitat: rural or urban, coastal or inland.
- The social level based on the monthly income of the parents.
- The number of bedrooms and the number of people in the house (promiscuity).
- Mother’s education level.
Personal History
- Concept of prematurity.
- Birth weight.
- Breast feeding.
Vaccination
- Antistreptococcus.
- Concept of passive smoking.
- Allergic terrain (clinical signs).
- Stay in crèches or daycare centers.
- History of repeated VAS infections.
- History of GERD.
- History of recurrent AOM.
Current weight: Obese or not (BMI).
Results
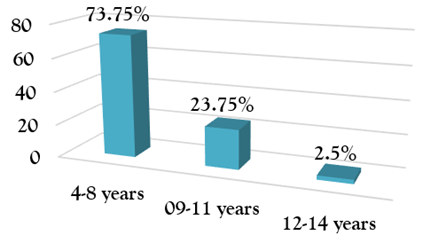
Factors seem to be related to the high prevalence of SMO, among them: young age, which represents a main risk factor, because it is a pediatric disease and as we grow up, there will be a decrease in the incidence of the disease. The distribution of patients according to age (Figure 1) finds a frequency peak at the age of four to eight years, with a percentage of 73.75percentage.
Figure 1: Distribution of patients according to age group on the date of the first consultation.
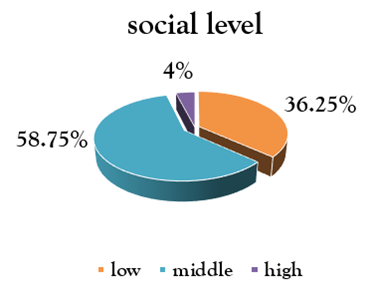
The criterion of promiscuity has been put forward by several authors, linking it to the social level of parents, being responsible for viral transmission during upper airways infections. In our study, 38.75percentage of families (n=31) live in F2s, with almost all (n=79) having more than 4 people per household and a high prevalence of the disease is found in families with a lower social level. low and medium (96percentage) (Figure 2).
Figure 2: distribution of patient families according to their social level.
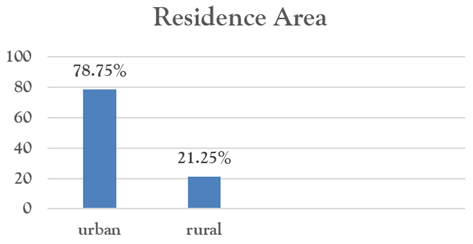
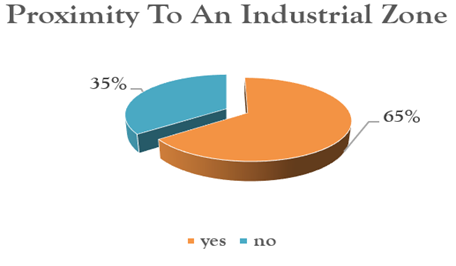
Most epidemiological studies found in the literature affirm the presence of an environmental pollution factor closely related to the high prevalence of SMO. Our results are in favor of these findings with a rate of 78.75% for urban housing (Figure 3), 65% for residence near an industrial zone (Figure 4).
Figure 3: distribution of patients according to their area of residence.
Figure 4: distribution of patients according to the proximity of the place of residence to an industrial zone.
According to several authors, the mother's education appears to be a determining factor in the prevalence of SMO. Our results are in favor of a high prevalence of the disease in the group of mothers whose level of education does not exceed secondary studies (n=73, 91.25%), and with the same 38.75% (n= 31) mothers with a low level of education, i.e., not exceeding the 6th year of primary school (Table 1).
Table 1: distribution of patients’ mothers according to their level of education.
| Mother's Education Level | Frequencies | % |
| Down | 31 | 38,75% |
| Middle | 42 | 52,50% |
| High | 7 | 8,75% |
| Total | 80 | 100,00% |
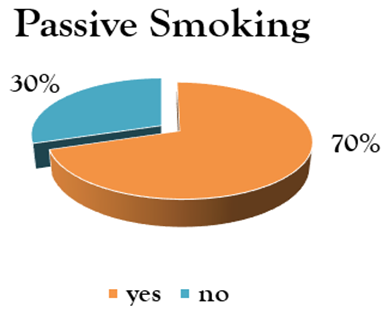
It is clear that there is compelling evidence of an association between exposure to tobacco smoke and otitis media in children. Our results are quite similar, because in our series the rate of passive smoking (especially the father, an uncle and sometimes even a grandfather living with the family) is high 70% (n= 56) (Figure 5).
Figure 5: distribution of patients according to the presence or absence of passive smoking.
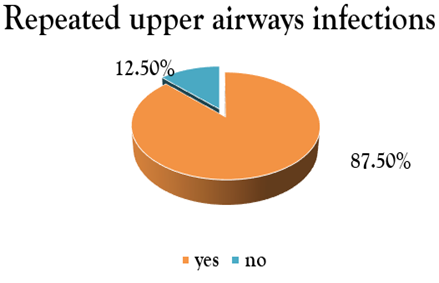
The presence and repetition of infectious episodes of the upper airways is responsible for the high prevalence of SMO, especially if these episodes exceed 4 per year. For our part, the frequency of recurrent UADT infections is high with a rate of 87.50% (n=70) (Figure 6), with, according to the majority of parents, more than 3 episodes per year.
Figure 6: distribution of patients according to the presence or absence of a notion of repeated VAS infections.
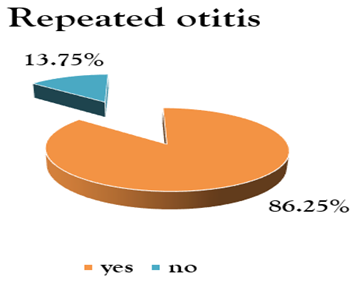
Also, the high percentage of otitis episodes in the past of the patients in the series was high 86.25% (n=69) (Figure 7).
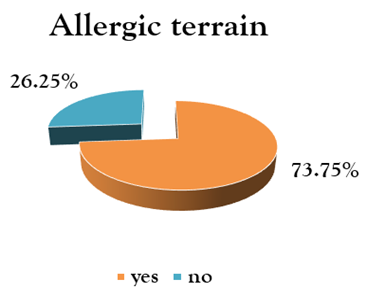
Respiratory allergy (associated or not with bronchial asthma) represents 73.75% (n=59) of cases (Figure 8).
Figure 8: distribution of patients according to the presence of allergic signs.
Diagnostic confirmation was based on skin reaction to allergens (Prick Test). In the 59 children suspected of having allergic rhinitis, the prick tests came back positive in 81.36% of cases (n= 48). The almost majority of patients were allergic to dust mites (DPT, DF and blomia), molds and 5-grasses. We also noted several cases of polysensitization (several allergens). Other factors appear to play a protective role on the development of SMO, such as breastfeeding, which may be protective in the first years of life, but its protective action may not cover older children. In our study we find a fairly significant figure of breastfeeding less than 06 months (n = 64, 80%), with especially 43.75% of children breastfed less than 03 months (Table 2).
Table 2: distribution of patients according to duration of breastfeeding.
| Breastfeeding | Frequencies | % |
| 0 | 10 | 12,50% |
| 0-3 months | 25 | 31,25% |
| 3-6 months | 29 | 36,25% |
| 6-12 months | 5 | 6,25% |
| > 12 months | 11 | 13,75% |
| Total | 80 | 100,00% |
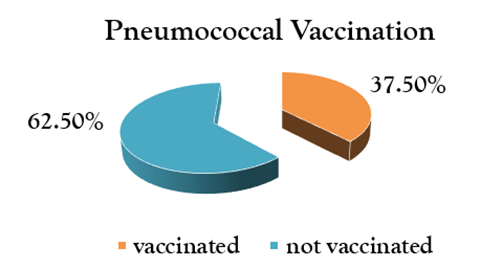
The positive effect of the pneumococcal vaccine is directly related to the reduction in nasopharyngeal carriage of pneumococcus (serotypes included in the PCV13 vaccine). In our series, SMO seems to be more frequent in children not vaccinated with PCV13 with a rate of 62.50% (n=50) (Figure 9).
Figure 9: distribution of patients according to pneumococcal vaccination (PCV13).
According to our results, other factors seem to have no relationship with the pathogenesis of this pathology. This is the case for cousin marriage, prematurity, stay in daycare, gastroesophageal reflux disease (GERD) and obesity.
Table 3: Risk factors unrelated to OSM.
| Cousin Marriage | Frequencies | % |
| No | 69 | 86,25% |
| Yes | 11 | 13,75% |
| Total | 80 | 100,00% |
| Prematurity | Frequencies | % |
| No | 75 | 93,75% |
| Yes | 5 | 6,25% |
| Total | 80 | 100,00% |
| Stay In Nurseries | Frequencies | % |
| No | 36 | 45,00% |
| Yes | 44 | 55,00% |
| Total | 80 | 100,00% |
| GERD | Frequencies | % |
| No | 69 | 86,25% |
| Yes | 11 | 13,75% |
| Total | 80 | 100,00% |
| Obésity | Frequencies | % |
| Non | 75 | 93,75% |
| Oui | 5 | 6,25% |
| Total | 80 | 100,00% |
Comparison between group with AH versus group without AH
Depending on the presence or absence of adenoid hypertrophy (AH), the patients were divided into two groups: group A (n=68) with AH and group B (n=12) without AH. Despite the fairly small number of the two groups, especially group B, we can still try to compare the main risk factors between the two groups. We note that the factors which have a statistically significant relationship with the presence of hypertrophy of the adenoids associated with SMO are the proximity of an industrial zone (P= 0.035), passive smoking (P= 0.0341) and recurrent upper airway infections (P= 0.00002) (Table 4).
Table 4
| Groupe A, SMO With AH (N=68) | Groupe B, SMON Without AH (N=12) | ||||
| Proximity to an Industrial Zone | Frequencies | % | Frequencies | % | Khi2 = 4,4128, P = 0,035, Significant |
| No | 27 | 39,71% | 1 | 8,33% | |
| Yes | 41 | 60,29% | 11 | 91,67% | |
| Total | 68 | 100,00% | 12 | 100,00% | |
| Passive Smoking | Frequencies | % | Frequencies | % | Khi2 = 4,4865, P = 0,0341, Significant |
| No | 24 | 35,29% | 0 | 0% | |
| Yes | 44 | 64,71% | 12 | 100,00% | |
| Total | 68 | 100,00% | 12 | 100,00% | |
| Repeated UADT Infections | Frequencies | % | Frequencies | % | Khi2 = 18,1513, P = 0,00002, Very Significant |
| No | 4 | 5,88% | 6 | 50,00% | |
| Yes | 64 | 94,12% | 6 | 50,00% | |
| Total | 68 | 100,00% | 12 | 100,00% | |
Discussion
Sero-mucosal otitis (SMO) is an extremely common condition, which in the vast majority of cases affects children under the age of 10. Its frequency is difficult to assess and differently described in world literature. It is the most common cause of deafness in children [2]. Numerous studies have focused on the different factors cited above, with very variable, even contradictory, results. Hundreds of publications have focused on the analysis of several risk factors, some of which are even more difficult to interpret. Craniofacial malformations such as velar clefts, cleft palates, trisomy 21 and craniostenosis represent a very significant risk factor for SMO and several studies confirm this, such as the meta-analysis by Emmanuel Choffor-Nchinda and Col. 2020 [3], or the authors confirm that velar clefts represent the most significant risk factor for SMO. For our study, this factor was excluded to eliminate any risk of confusion. For the age factor, our results are in favor of a close relationship, because 90% of patients are under 10 years old, which is similar to the results of Al-Humaid I. Humaid and col, in Saudi Arabia 2014 [4], and the meta-analysis of Emmanuel Choffor-Nchinda and col, in Cameroon 2020, studying the overall prevalence of SMO in the African continent [3].
The promiscuity factor has been put forward by several authors [5-7], linking it to the social level of the parents. Our results are similar to those of Ibekwe Matilda Uju and col.2020 [8], where the authors describe a strong relationship of SMO with having more than 3 people per room. J. Umutoni and col, in Rwanda 2021 find a high prevalence of SMO in categories with low socio-economic status [9,10], which supports our results. Some studies [11,12] found in the international literature, affirm the presence of an environmental pollution factor closely related to the high prevalence of otitis media. Our results support these findings with a rate of 78.75% for urban housing and 65% for residence near an industrial zone. For the factor of maternal education level, our results are quite close to those of most studies, which find a strong relationship of low maternal education level with the prevalence of SMO, such as that of Erdogan. Gultekin and col [13] and that of Al-Humaid I. Humaid and col [4]. Various studies [18,19] support the protective role of breastfeeding on the development of SMO. Our results are not close to those of Y. Yazibane [14], who in his study found that breastfeeding was the most frequent (47%) and that artificial breastfeeding only represented 18% of cases. On the other hand, our results are similar to those of F. Martines and col [15] and Khaled Saad and col, in Egypt 2020 [16], who found a strong statistical relationship of the disease with the total absence of breastfeeding.
The association between exposure to tobacco smoke and otitis media in children has been strongly proven by work based on measurements of salivary or urinary levels of cotinine [17,18], who were the most objective in affirming this relationship. Erdogan Gultekin and col [13] found a very significant association with the smoking of both parents and even more with that of the mother. This supports our results. Upper respiratory infections, as well as recurrent acute otitis media, appear to be determining factors in the pathogenesis of SMO. Our findings are in line with those of G AYDEMIR and col [6], by Nida Riaz and col [19] and other authors [9,10]. All of the studies found in the literature supported a strong correlation of allergic rhinitis with the high prevalence of SMO [10,16,19]. These findings support our results which would be favorable to the management of OSM associated with allergic rhinitis, possibly using specific immunotherapy. The effectiveness of PCV vaccines in reducing nasopharyngeal carriage of pneumococcus has been proven [20,21]. Mark Edmondson-Jones and col, in Sweden 2020, also observed a decrease in the incidence of OM after introduction of PCV13 [22]. Our results are supportive of these findings.
It must be emphasized that other risk factors, whose relationship with the disease is less obvious, or even absent, exist, namely consanguineous marriage, prematurity, GERD and obesity, as well as others, less frequently found in the literature, such as neonatal distress, cesarean delivery, low birth weight and many others.
Comparison between group with AH versus group without AH
In our series, children with AH represented 85% of cases (n=68, group A) and those without AH represented 15% (n=12, group B). By comparing the relationship of risk factors with the presence of AH in the two groups, we note that the factors which have a statistically significant relationship with the presence of hypertrophy of the adenoids associated with SMO are repeated infections. Of upper airways (p= 0.00002), passive smoking (p= 0.0341) and proximity to an industrial zone (p= 0.035) (Table 4). From these findings, we can consider AH as a disease associated with SMO and which presents risk factors intertwined with those of SMO, as we can consider it, as a risk factor for SMO.
Conclusion
SMO is the main cause of hearing loss in children and its pathogenesis remains controversial, with several risk factors having been incriminated. Studying these risk factors for SMO may be important for two reasons; firstly, we can have clues for a better understanding of the etiology of the disease and therefore be able to institute a prevention program. Second, knowledge of these risk factors can lead to a definition of high-risk groups, within the framework of a screening program. Our analysis in reality, even if it provides us with findings, has only an overall estimated value and only a multi-variate analysis by logistic regression, by associating a control group, will make it possible to statistically relate the risk factor to the disease. This can be envisaged in the perspectives of this work.
Conflicts of Interest
The authors declare that they have no conflict of interest regarding the publication of this article.
References
- Rosenfeld RM, Post JC. (1992). Meta-Analysis of Antibiotics for The Treatment of Otitis Media with Effusion. Otolaryngology-Head and Neck Surgery. 106(4):378-386.
Publisher | Google Scholor - Triglia JM, Roman S, Nicolas R. (2003). Otites Séromuqueuses. Encycl. Méd. Chir. (Editions Scientifiques Et Médicales), Elsevier SAS, Paris, Oto-Rhino-Laryngologie, 12.
Publisher | Google Scholor - Choffor‐Nchinda E, Bola Siafa A, Nansseu JR. (2020). Otitis Media with Effusion in Africa‐Prevalence and Associated Factors: A Systematic Review and Meta‐Analysis. Laryngoscope Investigative Otolaryngology. 5(6):1205-1216.
Publisher | Google Scholor - Al-Humaid HI, Abou-Halawa AS. (2014). Prevalence and Risk Factors of Otitis Media with Effusion in School Children in Qassim Region of Saudi Arabia. IJHS. 8(4):329-338.
Publisher | Google Scholor - Amusa YB, Ijadunola IKT, Onayade OO. (2005). Epidemiology Of Otitis Media in A Local Tropical African Population. West African Journal of Medicine. 24(3):227-230.
Publisher | Google Scholor - Aydemir G, Ozkurt F. (2011). Otitis Media with Effusion in Primary Schools in Princes’ Islands, Istanbul: Prevalence and Risk Factors. J Int Med Res. 39(3):866-872.
Publisher | Google Scholor - Songu M, Islek A, Imre A, Aslan H, Aladag I, et al. (2020). Risk Factors for Otitis Media with Effusion in Children with Adenoid Hypertrophy. Acta Otorhinolaryngol Ital. 40(2):133-137.
Publisher | Google Scholor - Uju IM, Ichendu PN. (2020). Otitis Media with Effusion Among Children in A Tertiary Hospital in Port Harcourt. 9:18.
Publisher | Google Scholor - Humaid AHI, Abou-Halawa SA, Masood KA, Nuha AHS, Al Duways Ali Saleh AM. (2014). Prevalence and Risk Factors of Otitis Media with Effusion in School Children in Qassim Region of Saudi Arabia. International Journal of Health Sciences. 8(4):325.
Publisher | Google Scholor - Bamaraki K, Namwagala J, Hidour R, Bambi EN. (2022). Otitis Media with Effusion in Children Aged 2-12 Years Attending the Paediatric Clinic at Mulago National Referral Hospital, A Ugandan Tertiary Hospital: A Cross-Sectional Study. 1-14.
Publisher | Google Scholor - Park M, Han J, Jang M Jin, Suh MW, Lee JH, et al. (2018). Air Pollution Influences the Incidence of Otitis Media in Children: A National Population-Based Study. Larcombe A, Éditeur. Plos ONE. 13(6):E0199296.
Publisher | Google Scholor - Bowatte G, Tham R, Perret J, Bloom M, Dong G, et al. (2018). Air Pollution and Otitis Media in Children: A Systematic Review of Literature. IJERPH. 15(2):257.
Publisher | Google Scholor - Gultekin E, Develioğlu ÖN, Yener M, Ozdemir I, Külekçi M. (2010). Prevalence and Risk Factors for Persistent Otitis Media with Effusion in Primary School Children in Istanbul, Turkey. Auris Nasus Larynx. 37(2):145-149.
Publisher | Google Scholor - Y. Yazibane. (2012). Les OSM Aspects Cliniques, Évolutifs et Prise En Charge. Thèse DESSM.
Publisher | Google Scholor - Martines F, Bentivegna D, Maira E, Sciacca V, Martines E. (2011). Risk Factors for Otitis Media with Effusion: Case–Control Study in Sicilian Schoolchildren. International Journal of Pediatric Otorhinolaryngology. 75(6):754-759.
Publisher | Google Scholor - Saad K, Abdelmoghny A, Abdel-Raheem YF, Gad EF, Elhoufey A. (2020). Prevalence and Associated Risk Factors of Recurrent Otitis Media with Effusion in Children in Upper Egypt. World Journal of Otorhinolaryngology-Head and Neck Surgery. S2095881120301219.
Publisher | Google Scholor - Strachan DP, Jarvis MJ, Feyerabend C. (1989). Passive Smoking, Salivary Cotinine Concentrations, And Middle Ear Effusion In 7-Year-Old Children. BMJ. 298(6687):1549-1552.
Publisher | Google Scholor - Ilicali ÖC, Keleş N, Dèger K, Sàgun ÖF, Güldíken Y. (2001). Evaluation of The Effect of Passive Smoking on Otitis Media in Children by An Objective Method: Urinary Cotinine Analysis. Laryngoscope. 111(1):163-167.
Publisher | Google Scholor - Riaz N, Ajmal M, Khan MS. (2021). Frequency of Otitis Media with Effusion Among Children Aged 1–5 Years Presenting to Immunization Center of Tertiary Care Hospitals, Rawalpindi. World Journal of Otorhinolaryngology-Head and Neck Surgery. S2095881121000378.
Publisher | Google Scholor - Prymula R, Peeters P, Chrobok V, Kriz P, Novakova E, et al. (2006). Pneumococcal Capsular Polysaccharides Conjugated to Protein D For Prevention of Acute Otitis Media Caused by Both Streptococcus Pneumoniae and Non-Typable Haemophilus Influenzae: A Randomized Double-Blind Efficacy Study. 367:9.
Publisher | Google Scholor - Van Den Bergh MR, Spijkerman J, Swinnen KM, Francois NA, Pascal TG, et al. (2013). Effects Of The 10-Valent Pneumococcal Nontypeable Haemophilus Influenzae Protein D-Conjugate Vaccine on Nasopharyngeal Bacterial Colonization in Young Children: A Randomized Controlled Trial. Clinical Infectious Diseases. 56(3):e30‑e39.
Publisher | Google Scholor - Edmondson-Jones M, Dibbern T, Hultberg M, Anell B, Medin E, et al. (2021). The Effect of Pneumococcal Conjugate Vaccines on Otitis Media From 2005 To 2013 In Children Aged ≤5 Years: A Retrospective Cohort Study in Two Swedish Regions. Human Vaccines and Immunotherapeutics. 17(2):517-526.
Publisher | Google Scholor