Research Article
Risk Assessment among Pregnant Women in Nigeria: Requisite Step towards Reduced Maternal Morbidity and Mortality
- Adebukunola O. Afolabi 1*
- Ekpoanwan Esienumoh 2
- Kolade A. Afolabi 3
- Monisola Y. J. Omishakin 4
- Love B. Ayamolowo 1
1Department of Nursing Science, Obafemi Awolowo University, Ile-Ife, Nigeria.
2Department of Nursing Science, University of Calabar, Nigeria.
3Medical and Health Services, Obafemi Awolowo University, Ile-Ife, Nigeria.
4Department of Nursing Science, Redeemer’s University, Ede, Nigeria.
*Corresponding Author: Adebukunola O Afolabi, Department of Nursing Science, Obafemi Awolowo University, Ile-Ife, Nigeria.
Citation: : Adebukunola O. Afolabi, Esienumoh E, Kolade A. Afolabi, M.Y.J. Omishakin, Love B. Ayamolowo. (2023). Risk Assessment among Pregnant Women in Nigeria: Requisite Step towards Reduced Maternal Morbidity and Mortality, Journal of Women Health Care and Gynecology, BioRes Scientia Publishers. 2(3):1-14. DOI: 10.59657/2993-0871.brs.23.018
Copyright: © 2023 Adebukunola O Afolabi, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: September 15, 2023 | Accepted: October 03, 2023 | Published: October 10, 2023
Abstract
Background: Existing risk assessment tools in pregnancy are limited in their predictive capabilities, whereas effective risk assessment should incorporate non-medical variables such as cultural and religious contexts of women, typical of African settings.
Objective: This study explored perception about risk in pregnancy, assessed knowledge about risk in pregnancy, examined risk status and related factors among pregnant women in Ile-Ife, southwest Nigeria.
Methods: Study employed sequential explanatory mixed method design. Quantitative data was collected using modified Dutta & Das Prenatal Scoring System from 239 pregnant women selected through a two-stage sampling technique. Regression analysis examined relationship between dependent and independent variables. Level of significance was P<0.05. Focus Group Discussion explored participants’ perception about risk in pregnancy. Qualitative responses were analyzed thematically.
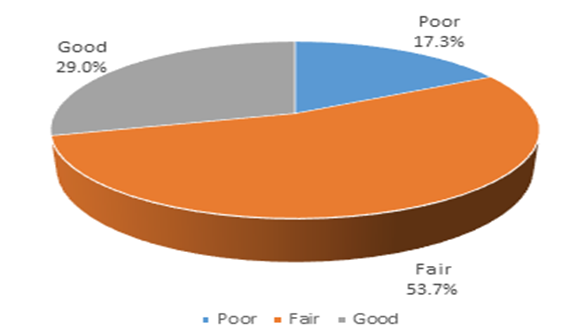
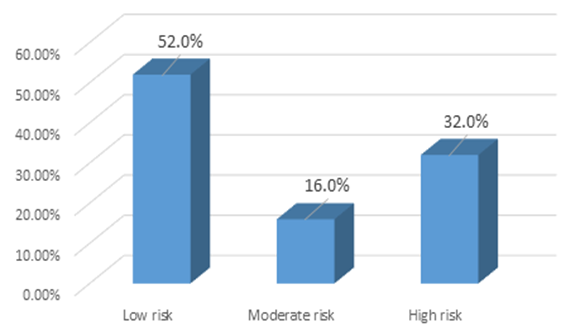
Results: Findings showed that 80.5% had positive perception about risk in pregnancy, 19.5% had negative perception, 29.0% had good knowledge about risk in pregnancy, 17.3% of the pregnant women had poor knowledge while 53.7% had fair knowledge. Study observed significant relationship between high risk in pregnancy and age group 15-24 years (p=0.01, RRR= 0.67, CI= 0.12-3.63), ethnicity (p=0.02, RRR=12.93, CI=1.42-117.76), poor knowledge about risk in pregnancy (p=0.03, RRR=4.08, CI=1.19-13.98), prim gravidity (p=0.001, RRR=0.01, CI=0.002-0.08), multigravidity (p=0.001, RRR=0.04, CI=0.02-0.29) and vaginal birth (p=0.001, RRR=0.21, CI= 0.08-0.54). Qualitative findings resulted in three themes namely; women’s perception about risk in pregnancy, perceived causes of risk in pregnancy, perceived risk preventive measures in pregnancy.
Conclusion: Study concluded that women’s age, ethnicity, knowledge about risk in pregnancy, gravidity and mode of birth were main predictors of risk in pregnancy. Intervention programs should take cognizance of these variables especially cultural contexts of women.
Keywords: pregnant women; risk in pregnancy; risk assessment in pregnancy; nigeria
Introduction
Pregnancy is a physiological state, a sensitive period associated with physical, biochemical and emotional changes in both mother and the growing fetus [1]. The World Health Organization, WHO [2] envisages a world where pregnant women receive quality care throughout pregnancy, birth and the postnatal period with priority focus on person-centered health and well-being. This phenomenon is geared towards reduction in maternal mortalities and morbidities: an essential component of Sustainable Development Goals (SDG) [3]. Worldwide, maternal mortality has been identified as a major public health challenge [4–6]. Global estimate shows that 810 women die daily as a result of pregnancy, childbirth and related complications with approximately 94% of these deaths occurs in developing countries with sub-Sahara Africa and southern Asia accounting for almost 86% of the total global maternal deaths while in Nigeria, the maternal mortality ratio as at 2017 was 917 per 100,000 live births translating into 23 Percentage deaths among women of reproductive age [7]. Many of these deaths are preventable especially with timely identification of risk factors and prompt interventions by experienced, skilled health care professionals especially midwives during the antenatal, perinatal and postnatal periods [7].
Similarly, several studies have shown that pregnancy, labour and puerperium are associated with varying degrees of risk and complications for the mother and or baby [1,8]. The above submission underscores the need for midwives, Obstetricians and other health care providers to be able to identify the category into which a pregnant woman belongs and subsequently institute appropriate intervention plan [9]. Consequently, antenatal care has been identified as the basis for improving maternal and neonatal wellbeing [10] with the aim of providing support for the pregnant woman, categorize pregnant women into risk status, identify associated risk factors and prioritize care in order to improve chances of successful pregnancy outcome and to ensure minimal adverse experience during pregnancy, labour and puerperium [1]. These are in addition to prompt identification and treatment of new medical or obstetric conditions during pregnan cy and where possible, prevent these from adversely affecting the health of the mother or baby, plan for labour and birth, care of the newborn and assist the woman to plan future reproductive health decisions [11].
Furthermore, the WHO recommends that the first visit by a pregnant woman to the antenatal clinic known as booking visit is expected between the 8th and 12th weeks gestation; this should aim to identify women who may need additional specialized care and to assist in planning the modality of management of pregnancy, labour, birth and puerperium. Specific information should be given to pregnant women concerning medications such as folic acid and other supplements, hygiene, lifestyle modification including smoking and alcohol cessation, antenatal screening and risks assessment [1,2]. Pregnancy is said to be at risk when the likelihood of an adverse outcome for the woman or the baby is greater than that of the normal population. The level of risk in pregnancy may be determined before pregnancy, during pregnancy or labour; the outcome of which can affect the woman or the baby or both [12]. The risk assessment and classification of pregnant women into high risk and low risk categories considers factors such as maternal characteristics such as age, number of children, time of previous deliveries, existing medical history and maternal education and other maternal variables which have been found to influence pregnancy outcomes. The prenatal period serves as distinctive window of opportunity to identify risks to both the pregnant woman, the growing fetus and through which several preventable adverse outcomes to mother and child could be identified and appropriate intervention put in place [11].
High risk pregnancies include those pregnancies associated with history of complications during previous pregnancies and or deliveries, pregnancies with metabolic diseases such as diabetes, hypertension, immunological disorders and pregnancies presenting with anomalies such as malnutrition, obesity, intrauterine growth retardation; such pregnancies require more intensive and focused monitoring and specialized care [11]. Risk assessment at the beginning of pregnancy remains valuable because the procedure enables women with observable risk factors to be identified early while prioritized attention is considered either for specialized care at the health facility or for appropriate referrals. In an attempt to promote a viable tool for assessing level of risk in pregnancy, Wilson [13] evaluated antenatal risk scoring for perinatal mortality, intrauterine growth restriction, preterm birth and low Apgar score at birth. Dutta & Das [14] similarly proposed a scoring system for identifying high risk mothers in pregnancy in India. These scoring systems and several other existing risk assessment scales are limited in their predictive capabilities because they focus mainly on medical, surgical and gynaecological factors [15] whereas effective risk assessment tools should incorporate non-medical variables such as demographic, cultural and religious contexts of women, typical of African settings [16]. It is therefore appropriate to undertake this study with the aim of exploring perception about risk in pregnancy, assessing level of knowledge about risk in pregnancy, assessing risk status and related factors among pregnant women attending antenatal clinic in Obafemi Awolowo University Teaching Hospitals, Ile-Ife, southwest Nigeria.
Methods
Study design
Study adopted sequential explanatory mixed method design using quantitative and qualitative data collection methods.
Study Setting
Study was conducted among pregnant women attending antenatal clinic in Ife Hospital Unit of the Obafemi Awolowo University Teaching Hospital, southwest Nigeria between between October and December, 2021. The Obafemi Awolowo University Teaching Hospitals is one of the first-generation tertiary health facilities established in 1967 by the Federal Government of Nigeria to provide qualitative health care services to the sub region. The hospital focuses on integrated healthcare birth system approach with emphasis on comprehensive healthcare service based on a pyramidal structure comprising primary care at the base, secondary and tertiary services at hospital settings, designed to secure improvement in the physical, mental and socio-economic wellbeing of Nigerians through preventive, promotive, diagnostic, restorative and rehabilitative services. The Obafemi Awolowo University Teaching Hospitals Complex has 5 main units for operational effectiveness namely: Ife hospital unit (IHU), Wesley guild hospital, Ilesa, urban comprehensive health centre, Eleyele, Ile-Ife, multipurpose health centre, Ilesa and rural community health centre, Imesi-Ile, all in southwestern region in Nigeria.
Inclusion and exclusion criteria
Pregnant women receiving antenatal care at the Ife hospital unit of the teaching hospital, Ile-Ife were included in the study, unbooked pregnant women were excluded from this study.
Sample size and sampling technique for quantitative data
The sample frame for the pregnant women over a period of 4 weeks was estimated to 480. The Taro Yamane method for sample size calculation was used to estimate sample size for the quantitative study: Given n= N / (1+N (e)2, where n = estimated sample size, N = sample frame (population under study), e = margin error (given as 0.05 in this study), n= 480 / (1+ 480 (0.05)2, n = 480 / (1 + 1.2) = 218, with 10% attrition rate, sample size was estimated to 239. Eligible women were selected through a two-stage sampling technique: Stage one involved purposive selection of Ife hospital unit (preliminary observation showed that then Ife unit has the highest number of women attending antenatal clinic compared to other units of the Obafemi Awolowo University Teaching Hospital. In the second stage, eligible women were selected by convenience sampling technique and selection continued daily at the antenatal clinic until the estimated sample size was attained.
Sample size and sampling technique for qualitative data
Four sessions of Focus Group Discussion (FGD) using FGD guide were conducted for the qualitative study with 10 discussants selected for each session giving total of 40 discussants. Discussants were purposively selected based on gravidity such that two sessions were conducted among primigravida and multigravida respectively. FGD explored participants’ perception about risk in pregnancy and related factors.
Research instrument for quantitative study
An interviewer-administered questionnaire was used for quantitative data collection. Section A of the questionnaire elicited information on socio-demographic and socio-economic characteristics of pregnant women, section B contains information on reproductive characteristics, section C contains items which assessed knowledge about risk in pregnancy while section D was adapted from Modified Prenatal Scoring System by Dutta & Das [14] . This section elicited information on past obstetric history, past medical and surgical history.
Research instrument for qualitative study
An FGD guide with 10 items was used to collect qualitative data. The FGD guide explored participants’ perception about risk in pregnancy and related factors.
Validity and reliability of instrument
Face and content validity of the research instrument was done by subjecting the instruments to review by experts in Nursing and Midwifery, Demography and Social Statistics, Obstetrics and Gynaecology. Each item of the instruments was reviewed to ensure their appropriateness and ability to meet the stated objective of the study. Necessary corrections were affected on the research instruments after review by experts. Reliability of the questionnaire was assessed through test-retest method to access stability of the research instruments while internal consistency of questionnaire was examined by calculating Cronbach’s alpha value for the questionnaire 0.76.
Procedure for data collection
The aim of study was explained to study participants and informed consent to participate was obtained. Women’s socio-demographic and socio-economic characteristics were elicited using relevant sections of research instruments while clinical and biophysical parameters were evaluated. Knowledge about risk among pregnant women was evaluated while risk status among pregnant women was assessed using the Modified Prenatal Scoring System by Dutta & Das [14] .
Data analysis and scoring
The outcome variables in this study were ‘risk status of pregnant women’. Independent variables included selected demographic, socio-economic and obstetric characteristics of women. These are characteristics that were observed in previous studies to influence the course of pregnancy. Data was processed and analyzed using IBM Statistical Product and Service Solutions (SPSS) software version 25. Analysis was done at univariate, bivariate and multivariate levels. P-value of less than 0.05 was considered significant. Knowledge about risk in pregnancy among the pregnant women were assessed using 7 items in section C of the questionnaire. Each correct option was scored “1” point while incorrect answer scored ‘zero’. Maximum score was 7 points; women with total score of 5-7 were categorized as having ‘good knowledge’ about risk in pregnancy, score of 2-4 was categorized as having ‘fair knowledge while score of 0-1 was categorized as ‘poor knowledge’.
Risk status among the pregnant women were assessed using 28 items in section D of the questionnaire. Maximum score obtainable was 56, while minimum score obtainable was ‘0’. Women with total score of 0-2 were categorized as having ‘Low risk’; scores of 3-4 was categorized as ‘Moderate risk’; while score of ≥5 was categorized as ‘High risk’.
Factors associated with risk in pregnancy was evaluated by examining the relationship between risk status of the pregnant women (outcome variable) and selected women’s demographic, socio-economic and obstetric characteristics of women (Independent variable). Chi-square statistic examined relationship between dependent variable and the independent variables at bivariate, multinomial logistic regression analysis assess the simultaneous effects of independent variables) on the dependent variable.
Results
Findings showed that 57.2% of the pregnant women were aged 25-34 years old, 22.5% were aged 35-44 years old while 20.3% were aged 15-24 years old. The mean age was 29 years ± 5 SD (Table1).
In addition, 52.4% of the pregnant women had their first marriage between ages 25-34 years old, 30.7%) had their first marriage at age 15-24 years old, 4.3% had their first marriage at age 35-44 years old while 12.6% were unmarried. The mean age at first marriage was 23 years ± 3 SD. 58.5% women were multigravida, 26.8% were primigravida while 14.7% were grand multigravida, 35.5% were nullipara, 31.6% were primipara while 32.9% were multipara (Table2).
Table 1: Socio-demographic and socio-economic characteristics of pregnant women N=231.
| Variables | Frequency | % |
| Age at last birthday (years)Mean = 29 ± 5 SD | ||
| 15-24 | 47 | 20.3 |
| 25-34 | 132 | 57.2 |
| 35-44 | 52 | 22.5 |
| Place of residence | ||
| Rural | 110 | 47.6 |
| Urban | 121 | 52.4 |
| Marital status | ||
| Married | 202 | 87.4 |
| Single | 29 | 12.6 |
| Family type | ||
| Monogamous | 144 | 62.3 |
| Polygamous | 58 | 25.1 |
| Single | 29 | 12.6 |
| Ethnicity | ||
| Yoruba | 153 | 66.2 |
| Hausa | 27 | 11.7 |
| Igbo | 34 | 14.7 |
| Others (Itsekiri/Urhobo) | 17 | 7.4 |
| Religion | ||
| Christianity | 149 | 64.5 |
| Islam | 82 | 35.5 |
| Highest level of education | ||
| No formal education | 17 | 7.4 |
| Primary | 37 | 16.0 |
| Secondary | 71 | 30.7 |
| Tertiary | 106 | 45.9 |
| Employment status | ||
| Not employed | 55 | 23.8 |
| Self employed | 102 | 44.2 |
| Employed by Government | 49 | 21.2 |
| Employed by private sector | 25 | 10.8 |
| *Average monthly income | ||
| < 30> | 95 | 41.1 |
| ≥ 30,000 naira | 136 | 58.9 |
| Socio-economic status | ||
| Low | 40 | 17.3 |
| Middle | 37 | 16.0 |
| High | 154 | 66.7 |
*30,000 naira was the minimum wage in Nigeria as at the time of this study.
Table 2: Reproductive characteristics of pregnant women N=231.
| Variables | Frequency | % |
| Age at first marriage (years) Mean=23 years ± 3 SD | ||
| 15-24 | 71 | 30.7 |
| 25-34 | 121 | 52.4 |
| 35-44 | 10 | 4.3 |
| Age at first pregnancy (years): Mean=25±5 SD | ||
| 15-24 | 113 | 48.9 |
| 25-34 | 106 | 45.9 |
| 35-44 | 12 | 5.2 |
| Estimated gestational age of index pregnancy at booking (weeks): Mean=17 ± 6 SD | ||
| First trimester | 48 | 20.8 |
| Second trimester | 164 | 71.0 |
| Third trimester | 19 | 8.2 |
| Estimated gestational age of index pregnancy at the time of data collection (weeks): Mean= 27± 7 SD | ||
| First trimester | 11 | 4.8 |
| Second trimester | 50 | 21.6 |
| Third trimester | 170 | 73.6 |
| Gravidity | ||
| Primigravida | 62 | 26.8 |
| Multigravida | 135 | 58.5 |
| Grand multigravida | 34 | 14.7 |
| Parity | ||
| Nullipara | 82 | 35.5 |
| Primipara | 73 | 31.6 |
| Multipara | 76 | 32.9 |
| Mode of last delivery | ||
| Nullipara | 82 | 35.5 |
| Vaginal delivery | 108 | 46.8 |
| Caesarian section | 41 | 17.7 |
Twenty nine percent of the pregnant women had good knowledge about risk in pregnancy, 17.3% had poor knowledge while 53.7% had fair knowledge (Figure 1). Fifty two percent of the pregnant women were at low risk in pregnancy, about one-third (32.0%) were at high risk while 16.0% were at moderate risk (Figure 2).
Figure 1: Knowledge about risk in Pregnancy.
Figure 2: Risk status of pregnant women.
Furthermore, analysis of factors that influence risk in pregnancy at the bivariate level revealed significant relationship between risk in pregnancy and women’s’ age at last birthday (p = 0.001), place of residence (p=0.03), religion (p=0.03), highest level of education (p=0.002), employment status (p=0.001), average monthly income (p=0.001) and socio-economic status (p=0.01). (Table3). Bivariate analysis also revealed significant relationship between risk in pregnancy and women’s gravidity (p=0.001), mode of last birth (p=0.01). (Table 4).
Table 3: Bivariate analysis of association between Socio-demographic characteristics and risk in pregnancy N=231.
| Risk status in pregnancy | |||||
| Variables | Low risk n (%) | Moderate risk n (%) | High risk n (%) | Total n (%) | Statistic χ2 df p |
| Age at last birthday (year) | 20.40 2 0.001 | ||||
| 15-24 | 33 (70.2) | 06 (12.8) | 08 (17.0) | 47 (100.0) | |
| 25-34 | 72 (54.5) | 22 (16.7) | 38 (28.8) | 132 (100.0) | |
| 35-44 | 15 (28.8) | 09 (17.3) | 28 (53.8) | 52 (100.0) | |
| Place of residence | 6.89 1 0.03 | ||||
| Rural | 65 (59.1) | 19 (17.3) | 26 (23.6) | 110 (100.0) | |
| Urban | 55 (45.5) | 18 (14.9) | 48 (39.7) | 121 (100.0) | |
| Marital status | 4.22 1 0.12 | ||||
| Married | 100 (49.5) | 35 (17.3) | 67 (33.2) | 202 (100.0) | |
| Single | 20 (69.0) | 02 (6.9) | 07 (24.1) | 29 (100.0) | |
| Ethnicity | 8.14 3 0.23 | ||||
| Yoruba | 83 (54.2) | 23 (15.0) | 47 (30.7) | 153 (100.0) | |
| Hausa | 13 (48.1) | 05 (18.5) | 09 (33.3) | 27 (100.0) | |
| Igbo | 12 (35.3) | 06 (17.6) | 16 (47.1) | 34 (100.0) | |
| Others (Itsekiri, Ijaw,) | 12 (70.6) | 03 (17.6) | 02 (11.8) | 17 (100.0) | |
| Religion | 6.87 1 0.03 | ||||
| Christianity | 68 (45.6) | 26 (17.4) | 55 (36.9) | 149 (100.0) | |
| Islam | 52 (63.4) | 11 (13.4) | 19 (23.2) | 82 (100.0) | |
| Highest level of education | 20.28 3 0.002 | ||||
| No formal education | 10 (58.8) | 03 (17.6) | 04 (23.5) | 17 (100.0) | |
| Primary | 31 (83.8) | 02 (5.4) | 04 (10.8) | 37 (100.0) | |
| Secondary | 31 (43.7) | 15 (21.1) | 25 35.2) | 71 (100.0) | |
| Tertiary | 48 (45.3) | 17 (16.0) | 41 (38.7) | 106 (100.0) | |
| Employment status | 21.61 3 0.001 | ||||
| Not employed | 40 (72.7) | 07 (12.7) | 08 (14.5) | 55 (100.0) | |
| Self employed | 46 (45.1) | 21(20.6) | 35 (34.3) | 102 (100.0 | |
| Employed by Government | 19 (38.8) | 05 (10.2) | 25 (51.0) | 49 (100.0) | |
| Employed by private sector | 15 (60.0) | 04 (16.0) | 06 (24.0) | 25 (100.0) | |
| Average monthly income | 14.14 1 0.001 | ||||
| < 30> | 62 (65.3) | 15 (15.8) | 18 (18.9) | 95 (100.0) | |
| ≥ 30,000 naira | 58 (42.6) | 22 (16.2) | 56 (41.2) | 136 (100.0) | |
| Socio-economic status | 13.36 2 0.01 | ||||
| Low | 29 (72.5) | 05 (12.5) | 06 (15.0) | 40 (100.0) | |
| Middle | 23 (62.2) | 06 (16.2) | 08 (21.6) | 37 (100.0) | |
| High | 68 (44.2) | 26 (16.9) | 60 (39.0) | 154 (100.0) | |
Table 4: Bivariate analysis of association between reproductive characteristics and risk in pregnancy N=231.
| Risk status in pregnancy | |||||
| Variables | Low risk n(%) | Moderate risk n(%) | High risk n(%) | Total n(%) | Statistic χ2 df p |
| Age at first marriage (years) | 9.48 3 0.15 | ||||
| 15-24 | 42 (59.2) | 11 (15.5) | 18 (25.4) | 71 (100.0) | |
| 25-34 | 55 (45.5) | 22 (18.2) | 44 (36.4) | 121 (100.0) | |
| 35-44 | 03 (30.0) | 02 (20.0) | 05 (50.0) | 10 (100.0) | |
| Age at first pregnancy (years) | 4.70 2 0.32 | ||||
| 15-24 | 65 (57.5) | 13 (11.5) | 35 (31.0) | 113 (100.0) | |
| 25-34 | 50 (47.2) | 22 (20.8) | 34 (32.1) | 106 (100.0) | |
| 35-44 | 05 (41.7) | 02 (16.7) | 05 (41.7) | 12 (100.0) | |
| Estimated gestational age at booking (weeks) |
| 7.38 2 0.12 | |||
| First trimester | 21 (43.8) | 13 (27.1) | 14 (29.2) | 48 (100.0) | |
| Second trimester | 88 (53.7) | 20 (12.2) | 56 (34.1) | 164 (100.0) | |
| Third trimester | 11 (57.9) | 04 (21.1) | 04 (21.1) | 19 (100.0) | |
| Estimated gestational age at the time of data collection (weeks) | 7.42 2 0.12 | ||||
| First trimester | 03 (27.3) | 04 (36.4) | 04 (36.4) | 11 (100.0) | |
| Second trimester | 31 (62.0) | 04 (8.0) | 15 (30.0) | 50 (100.0) | |
| Third trimester | 86 (50.6) | 29 (17.1) | 55 (32.4) | 170 (100.0) | |
| Gravidity | 42.86 2 0.001 | ||||
| Primigravida | 48 (77.4) | 02 (3.2) | 12 (19.4) | 62 (100.0) | |
| Multigravida | 67 (49.6) | 29 (21.5) | 39 (28.9) | 135 (100.0) | |
| Grand multigravida | 05 (14.7) | 06 (17.6) | 23 (67.6) | 34 (100.0) | |
| Parity | |||||
| Nullipara | 49 (59.8) | 11 (13.4) | 22 (26.8) | 82 (100.0) | |
| Primipara | 42 (57.5) | 10 (13.7) | 21 (28.8) | 73 (100.0) | |
| Multipara | 29 (38.2) | 16 (21.1) | 31 (40.8) | 76 (100.0) | |
| Mode of last delivery | 13.24 1 0.01 | ||||
| Vaginal delivery | 60 (55.6) | 17 (15.7) | 31 (28.7) | 108 (100.0) | |
| Caesarian section | 11 (26.8) | 09 (22.0) | 21 (51.2) | 41 (100.0) | |
| Nullipara | 49 (59.8) | 11 (13.4) | 22 (26.8) | 82 (100.0) | |
Further analysis at the multivariate level however showed significant relationship between high risk in pregnancy and age group 15-24 years (p=0.01, RRR= 0.67, CI= 0.12-3.63), age group 25-34 years (p=0.001, RRR=0.37, CI=0.12-1.15), hausa ethnicity (p=0.02, RRR=12.93, CI=1.42-117.76), Igbo ethnicity (p= 0.03, RRR=9.43, CI=1.27-70.03), poor knowledge about risk in pregnancy (p=0.03, RRR=4.08, CI=1.19-13.98) (Table5). The relative risk for women aged 15-24 years old (RRR= 0.67) having high risk in pregnancy was higher than the relative risk for women aged 25-34 years old (RRR=0.37) relative to low risk. Similarly, the relative risk in pregnancy for hausa women (RRR=12.93) having high risk in pregnancy was higher than the relative risk for Igbo women (RRR=9.43) relative to low-risk status in pregnancy. In addition, the relative risk of having high risk in pregnancy among women with poor knowledge (RRR=4.08) was higher than the relative risk for women with fair knowledge about risk in pregnancy (RRR=0.97) relative to low-risk status in pregnancy.
Findings also shows significant relationship between moderate risk in pregnancy and women with no formal education (p=0.001, RRR=1.91, CI=1.16-3.15), women with primary education (p=0.001, RRR=1.04, CI=0.61-1.79), women with low socio-economic status (p=0.001, RRR=2.10, CI=0.21-20.09). (Table 5). The relative risk of having moderate risk in pregnancy among women with no formal education (RRR=1.91) was higher than the relative risk for women with primary education (RRR=1.04) relative to low risk. Similarly, the relative risk of having moderate risk in pregnancy for women with low socio-economic status (RRR=2.10) was lower than the relative risk for women with middle socio-economic status (RRR=5.22) relative to low-risk status in pregnancy.
Multivariate analysis also revealed significant relationship between moderate risk in pregnancy and prim gravidity (p=0.001, RRR=0.01, CI=0.001-0.05) (Table 6).
Table 5: Multinomial regression analysis of association between risk in pregnancy and socio-demographic characteristics
| Moderate risk | High risk | |||||
| Socio-demographic variables | p-value | RRR | Confidence Interval (CI) | p-value | RRR | Confidence Interval (CI) |
| Age at last birthday (year) | ||||||
| 15-24 | 0.64 | 0.67 | 0.12-3.63 | 0.01 | 0.12 | 0.03-0.54 |
| 25-34 | 0.08 | 0.37 | 0.12-1.15 | 0.001 | 0.20 | 0.07-0.52 |
| 35-44 | RC | 1 | 1 | |||
| Place of residence | ||||||
| Rural | 0.83 | 0.90 | 0.35-2.32 | 0.62 | 0.82 | 0.37-1.82 |
| Urban | RC | 1 | 1 | |||
| Marital status | ||||||
| Married | 0.16 | 3.94 | 0.57-27.22 | 0.50 | 0.59 | 0.13-2.72 |
| Single | RC | 1 | 1 | |||
| Ethnicity | ||||||
| Yoruba | 0.65 | 1.43 | 0.30-6.90 | 0.06 | 5.39 | 0.92-31.59 |
| Hausa | 0.50 | 2.07 | 0.25-16.88 | 0.02 | 12.93 | 1.42-117.76 |
| Igbo | 0.42 | 2.15 | 0.33-13.91 | 0.03 | 9.43 | 1.27-70.03 |
| Others (Itsekiri, Urhobo) | RC | 1 | 1 | |||
| Religion | ||||||
| Christianity | 0.93 | 0.95 | 0.31-2.95 | 0.80 | 1.14 | 0.43-2.98 |
| Islam | RC | 1 | 1 | |||
| Highest level of education | ||||||
| No formal education | 0.001 | 1.91 | 1.16-3.15 | 0.64 | 0.43 | 0.01-14.26 |
| Primary | 0.001 | 1.04 | 0.61-1.79 | 0.15 | 0.15 | 0.01-1.97 |
| Secondary | 0.76 | 1.18 | 0.40-3.53 | 0.79 | 0.88 | 0.35-2.23 |
| Tertiary | RC | 1 | 1 | |||
| Employment status | ||||||
| Not employed | 0.50 | 0.44 | 0.04-4.75 | 0.31 | 0.31 | 0.03-2.97 |
| Self employed | 0.33 | 1.97 | 0.51-7.62 | 0.45 | 1.62 | 0.47-5.62 |
| Employed by Government | 0.74 | 0.74 | 0.13-4.13 | 0.15 | 2.81 | 0.69-11.45 |
| Employed by private sector | RC | 1 | 1 | |||
| Average monthly income | ||||||
| < 30> | 0.42 | 0.55 | 0.13-2.33 | 0.28 | 0.50 | 0.14-1.77 |
| ≥ 30,000 naira | RC | 1 | 1 | |||
| Socio-economic status | ||||||
| Low | 0.001 | 2.10 | 0.21-20.09 | 0.37 | 7.70 | 0.09-655.18 |
| Middle | 0.13 | 5.22 | 0.62-43.99 | 0.20 | 3.80 | 0.50-29.06 |
| High | RC | 1 | 1 | |||
| Knowledge about risk | ||||||
| Poor | 0.64 | 1.42 | 0.33-6.14 | 0.03 | 4.08 | 1.19-13.98 |
| Fair | 0.86 | 1.10 | 0.38-3.22 | 0.94 | 0.97 | 0.39-2.43 |
| Good | RC | 1 | RC | 1 | ||
| Model statistics: n=231, p = 0.001, R square = 0.30 | ||||||
| Note: Base outcome = Low risk RRR=Relative risk ratio CI = Confidence interval at 95% | ||||||
Table 6: Multinomial regression analysis of association between risk in pregnancy and reproductive characteristics.
| Moderate risk | High risk | |||||
| Reproductive characteristics | p-value | RRR | Confidence Interval (CI) | p-value | RRR | Confidence Interval (CI) |
| Age at first marriage (years) | ||||||
| 15-24 | 0.67 | 2.05 | 0.08-54.83 | 0.61 | 0.52 | 0.04-6.61 |
| 25-34 | 0.70 | 1.89 | 0.08-45.26 | 0.57 | 0.49 | 0.04-5.59 |
| 35-44 | RC | 1 | RC | 1 | ||
| Age at first pregnancy (years) | ||||||
| 15-24 | 0.17 | 0.12 | 0.01-2.46 | 0.46 | 0.45 | 0.06-3.66 |
| 25-34 | 0.52 | 0.38 | 0.02-7.32 | 0.24 | 0.31 | 0.04-2.17 |
| 35-44 | RC | 1 | RC | 1 | ||
| Estimated gestation age at booking (weeks) | ||||||
| First trimester | 0.23 | 2.86 | 0.51-16.08 | 0.32 | 2.33 | 0.45-12.09 |
| Second trimester | 0.88 | 0.90 | 0.21-3.89 | 0.38 | 1.91 | 0.45-8.06 |
| Third trimester | RC | 1 | RC | 1 | ||
| Estimated gestation age as at time of data collection (weeks) | ||||||
| First trimester | 0.19 | 4.08 | 0.50-33.46 | 0.19 | 3.61 | 0.53-24.54 |
| Second trimester | 0.24 | 0.40 | 0.09-1.85 | 0.99 | 1.01 | 0.38-2.65 |
| Third trimester | RC | 1 | RC | 1 | ||
| Gravidity | ||||||
| Primigravida | 0.001 | 0.01 | 0.001-0.05 | 0.001 | 0.01 | 0.002-0.08 |
| Multigravida | 0.07 | 0.26 | 0.06-1.12 | 0.001 | 0.04 | 0.02-0.29 |
| Grandmultigravida | RC | 1 | RC | 1 | ||
| Parity | ||||||
| Nullipara | 0.69 | 1.46 | 0.24-9.00 | 0.74 | 0.75 | 0.14-3.97 |
| Primipara | 0.09 | 0.37 | 0.12-1.16 | 0.43 | 0.67 | 0.25-1.79 |
| Multipara | RC | 1 | RC | 1 | ||
| Mode of last delivery | ||||||
| Vaginal delivery | 0.09 | 0.37 | 0.12-1.17 | 0.001 | 0.21 | 0.08-0.54 |
| Caesarian section | RC | 1 | RC | 1 | ||
| Model statistics: n=231, p = 0.001, R square = 0.34 | ||||||
| Note: Base outcome = Low risk RRR=Relative risk ratio CI = Confidence interval at 95% | ||||||
Similarly, there was significant relationship between high risk in pregnancy and primigravidity (p=0.001, RRR=0.01, CI=0.002-0.08), multigravidity (p=0.001, RRR=0.04, CI=0.02-0.29) and vaginal birth (p=0.001, RRR=0.21, CI= 0.08-0.54) (Table6). The relative risk for moderate risk status in pregnancy among primigravida (RRR=0.01) was lesser than the relative risk among multigravida (RRR=0.26) relative to low-risk status in pregnancy. In addition, the relative risk for high-risk status in pregnancy for primigravid women (RRR=0.01) was lesser than the relative risk among multigravida (RRR=0.04) relative to low-risk status in pregnancy while the relative risk for high-risk status in pregnancy among women whose last child birth were through vaginal birth (RRR=0.21) was lesser than the relative risk among women who delivered through Caesarian section.
Qualitative findings
Qualitative findings identified three themes namely: women’s perception about risk in pregnancy, perceived causes of risk in pregnancy, perceived preventive measures. Women’s perception about risk in pregnancy: Risk in pregnancy was generally perceived as situations that pose threats or potential negative outcomes to pregnant women and or the fetus. FGD discussants generally opined that all pregnancies are associated with a measure of risk with varying degree of severity depending on the orientation of the woman to recognize danger signs and decision-making capability to seek skilled interventions. In support of this submission, a 34-year-old discussant retorted that: ‘…a pregnant woman is at risk when underlying medical conditions like infections, weight lost high blood pressure are left untreated. These conditions can lead to hazardous outcomes for the woman or her baby’. This submission was further supported by another discussant who opined that:’ …a pregnancy could be said to be at risk when the baby is not growing properly as expected. The woman may ne pale, poor feeding, get tired easily. These conditions require attention by doctors, nurses or other health workers’ (a 41-year-old discussant).
Perceived causes of risk in pregnancy: Responses from the FGD regarding causes of risk in pregnancy revealed that discussants identified underlying medical conditions like high blood pressure, level of education, employment status, previous unpalatable experiences in pregnancy, advance maternal age, number of previous pregnancies, some cultural taboos such as food restrictions, as probable causes of risk in pregnancy. A section of FGD discussants however opined those problems in pregnancy could result from cultural taboos or spells and witchcrafts activities, hence the need to be consult spiritual experts or traditionalist during pregnancy. Participants however opined that some of these conditions are preventable if identified early and managed. Below are excerpts to further buttress the above submission:
‘…Women with younger age will experience lower risk in pregnancy than older women, likewise women who gainfully employed may afford cost of quality medical treatment than unemployed women’. (a 28-year-old discussant).
‘Women who are educated may be more knowledgeable about danger signs of pregnancy. Such women will be able to take decision to visit the hospital promptly. The situation will be different for illiterate women’. (a 23-year-old discussant).
Perceived preventive measures: FGD discussants opined that some conditions that pose as threat during pregnancy could be prevented while some may not be preventable. It was generally opined that early booking and recognition danger signs of pregnancy with prompt visit to the hospital could reduce fatal outcomes. Below are excerpts to support the submission above:
‘…Dangers in pregnancy could be prevented if a pregnant woman registers her pregnancy in the hospital as early as possible. Early registration (booking) will enable nurses and doctors to monitor her properly and treat any dangerous conditions promptly’. (a 25-year-old discussants).
‘… a pregnant woman can prevent fatal outcomes if she reports any discomforts in pregnancy promptly. A pregnant woman should also comply with routine drug intake and advice given by the doctors and nurses. These will help prevent any unpalatable occurrences’; (a 43-year-old discussant).
Discussion of findings
Study found that about a third (29.0%) of the pregnant women had good knowledge about risk in pregnancy, 17.3% had poor knowledge while 53.7% had fair knowledge. This finding is comparable with result of a longitudinal study involving 157 pregnant women conducted by Theobald & Napendaeli [17] in Morogoro municipality, Tanzania to investigate level of maternal knowledge and attitudes towards risk in pregnancy which revealed that majority (70%) of the pregnant women were aware that risk factors could adversely affect pregnancy outcomes. The study by Theobald & Napendaeli concluded that although most women were aware of the pregnancy risk factors, the women lacked appropriate knowledge on how these factors could be prevented [17].
Findings from our study also showed that about half (52.0%) of the pregnant women were at low risk in pregnancy, one-third (32.0%) were at high risk in pregnancy while 16.0% were at moderate risk. This finding is consistent with result of a retrospective cohort study in a tertiary care center in Saudi Arabia which investigate the association between a validated antenatal risk scoring scale and involving 533 pregnant women undertaken by [18] where it was observed that 55.9% of the women had low antenatal risk scores, 34.7% had moderate risk scores while 9.4% had high risk scores. Al-Hindi et al concluded that antenatal risk scores remain a feasible tool in identifying risk status of pregnant women [18]. Findings above are consistent with the submission of Tulchinsky and Varavikova [19] who asserted that predictors of high risk pregnancies include maternal age, parity women and previous obstetric complications. To further corroborate this assertion, a study which compared the risk factors for adverse perinatal outcomes in adolescent age pregnancies and advanced age pregnancies among 187 pregnant women by Kuyumcuoglu et al [20] observed that women with advanced age were more prone to risk in pregnancy than younger women. Similarly, a multi-country study by the WHO [21] compared adolescents age (10-19 years) to women aged 20-24 years old. Study revealed that, adolescents aged 10-19 years were at higher risk of adverse pregnancy outcomes than older women. Similarly, Khalil et al [22] also evaluated the relationship between maternal age and adverse pregnancy outcomes. The study by Khalil et al observed that advanced maternal age (≥40 years old) was associated with higher risks of diabetes mellitus, miscarriage and pre-eclampsia [22]. A study conducted in the United States to ascertain if maternal race or ethnicity contributes to poor pregnancy outcomes showed that infants from Black, Hispanic, and Asian women suffered higher risk for adverse pregnancy outcomes when compared to infants from white women [23]. A retrospective study by Khalil et al [22] further observed significant association between racial background and a wide range of adverse pregnancy outcomes. In addition, studies in Iraq found association between adverse newborn outcomes such as preterm birth, stillbirth, post-datism, low birth weight, congenital anomalies and low level of education [24,25]. In their study to determine the risk of miscarriage among white and black women, Mukherjee et al observed that Black women were at higher risk of miscarriage when compared to white women [26]. Similarly, Ajiboye & Adebayo [27] observed a statistically significant association between socio-cultural factors and adverse pregnancy outcomes among Ugu community of Nigeria. A deep understanding of the influence of culture on health seeking behaviors is necessary in order to further strengthen and enhance the uptake and utilization of healthcare delivery services [28].
In addition, a study conducted in the United Kingdom to determine maternity care outcomes, utilization, and experience revealed that pregnant women of low socioeconomic status are 25% less likely to have received antenatal care, 15% less likely to have received routine postnatal check-up, 4% more likely to received antenatal hospital admission [29]. In addition, our study also revealed significant relationship between risk in pregnancy, gravidity, and previous mode of birth. To corroborate the influence of obstetric characteristics on risk status of a pregnant woman, findings from a study to evaluate the prevalence of anemia and the risk of haemo concentration during the three trimesters of pregnancy among women in a Mediterranean area in the south of Europe undertaken by Ribot et al [30] observed that the prevalence of anemia increased from 3.8% in the first trimester to 21.5% in the 3rd trimester. To further support the interplay between woman’s reproductive characteristics and risk in pregnancy, a study conducted among pregnant women in Norway by Wilcox et al [31] observed that the risk of miscarriage increases if the previous birth ended in a preterm birth. The study by Wilcox et al concluded that the risk of miscarriage varies greatly with maternal age [31]. Regarding perception about causes of risk in pregnancy and perceived preventive measures, a section of FGD discussants opined those problems in pregnancy could result from cultural taboos or spells and witchcrafts activities, hence the need to adhere to some cultural norms such as food cultural of family taboos such as food taboos, ancestral restrictions and consultations to spiritual experts or traditionalist during pregnancy. Such misconception contributes to delay in seeking skilled medical interventions. Women's perception about risk in pregnancy and psychological orientation of women are important factors to be considered with respect to prompt decision making capabilities of women and for intervention to be successful [32].
Conclusion
Study concluded that women’s age, ethnicity, knowledge about risk in pregnancy, gravidity and mode of birth were main predictors of risk in pregnancy. Intervention programs should take cognizance of these variables especially ethnic/cultural contexts of women. Midwives, health professionals and experts in women’s health should focus on improving women’s knowledge about risk in pregnancy and implications of gravidity of higher order.
Declarations
Implication of findings for Public Health, Nursing and Midwifery practices
Effective midwifery practices should priotize identification of existing or emerging risks variables in pregnancy towards optimal maternal and child health in addition to inclusion of non-medical components such as cultural and religious variables to routine maternal and child health services.
Nurses and midwives, should continue to create awareness about implications of gravidity and parity of higher order, promote timely uptake and utilization of maternal health services.
Strength and limitation of study
This study involves pregnant women attending a tertiary health facility in southwest Nigeria. The study sample could however be considered reasonably representative comprising of different categories of pregnant women with respect to educational background, marriage types, parity and employment status. The statistical tool employed and findings obtained in this study could be comparable with those obtainable from previous studies.
Ethics considerations
Ethical permission for this study was obtained from the Ethics and Research Committee of the Obafemi Awolowo University Teaching Hospitals Complex, Ile-Ife (Ethical approval number ERC/2021/12/01). Informed consent was obtained from selected pregnant women prior data collection.
Conflict of Interest
Authors declare no completing interest during the conduct and publication of this manuscript.
Funding
Authors of this manuscript did not receive funding or any form of financial assistance from any
government or organization during conduct and publishing this study.
References
- Anumba D, Jivraj S. (2018). Antenatal disorders for the MRCOG and Beyond. Cambridge University Press, 1-11.
Publisher | Google Scholor - World Health Organization W. (2016). Standards for improving quality of maternal and newborn care in health facilities.
Publisher | Google Scholor - United Nations. (2015). The 2030 agenda for sustainable development (SDG).
Publisher | Google Scholor - Prata N, Passano P, Sreenivas A, Gerdts CE. (2010). Maternal mortality in developing countries: challenges in scaling-up priority interventions. Womens Heal, 6:311-327.
Publisher | Google Scholor - Asamoah B, Moussa K, Stafström M, Musinguzi G. (2011). Distribution of causes of maternal mortality among different socio- demographic groups in Ghana; a descriptive study. BMC Public Health, 11.
Publisher | Google Scholor - Geller S, Koch A, Garland C, Macdonald EJ, Storey F, Lawton B. (2018). A global view of severe maternal morbidity: moving beyond maternal mortality. Reprod Health, 15(S1):98.
Publisher | Google Scholor - World Health Organization. (2019). Maternal mortality in 2000-2017 in Nigeria.
Publisher | Google Scholor - Cavazos-rehg PA, Krauss MJ, Spitznagel EL, Bommarito K, Madden T, Olsen MA, et al. (2015). Maternal age and risk of labor and delivery complications Patricia. Matern Child Heal J, 19(6):1202-1211.
Publisher | Google Scholor - Scrimshaw S, Backes E. (2020). Birth settings in America: Outcomes, quality, access, and choice. A Consensus Study Report of National Academies of Science, Engineering, Medicine. Washington DC: The national Academic press.
Publisher | Google Scholor - Ngxongo T. (2018). Basic Antenatal Care Approach to Antenatal Care Service Provision. Intech Open.
Publisher | Google Scholor - Haruna U, Dandeebo G, Galaa S. (2019). Improving access and utilization of maternal healthcare services through focused antenatal care in rural Ghana: A qualitative study. Adv public Heal.
Publisher | Google Scholor - National Institute for Health and Care Excellence (NICE). (2020). Intrapartum care for women with existing medical conditions or obstetric complications and their babies.
Publisher | Google Scholor - Wilson J. (1996). Antenatal risk assessment. In: Midwifery Practice: Core Topics 1. Palgrave, London, 34-57.
Publisher | Google Scholor - Dutta S, Das X. (1990). Identification of high risk mothers by a scoring system and it’s correlation with perinatal outcome. J Obs Gynaecol India, 40:181-190.
Publisher | Google Scholor - Salem A, Lacour O, Scaringella S, Herinianasolo J, Benski A, Stancanelli G, et al. (2018). Cross-sectional survey of knowledge of obstetric danger signs among women in rural Madagascar. BMC Pregnancy Childbirth, 18(46):1-9.
Publisher | Google Scholor - Elkayam U. (2018). How to Predict Pregnancy Risk in an Individual Woman with Heart Disease&lowest. J Am Coll Cardiol, 71(21):2431-2433.
Publisher | Google Scholor - Theobald C, Napendaeli P. (2020). Factors influencing pregnancy outcomes in morogoro Municipality, Tanzania. Tanzan J Health Res, 12(4):249-260.
Publisher | Google Scholor - Al-hindi M, Al Sayari T, Al Solami R, Al Baiti A, Alnemri J, Mirza I, et al. (2020). Association of Antenatal Risk Score with Maternal and Neonatal Mortality and Morbidity. Cureus, 12(12).
Publisher | Google Scholor - Tulchinsky T, Varavikova E. (2014). The new public health. Vol. 74, Public Health. Elsevier science and technology books, 329-332.
Publisher | Google Scholor - Kuyumcuoglu U, Guzel A, Celik Y. (2012). Comparison of the risk factors for adverse perinatal outcomes in adolescent age pregnancies and advanced age pregnancies. Ginekol Pol. 83:2012-2014.
Publisher | Google Scholor - World Health Organization (WHO). (2014). WHO multi-country study on women’s health and domestic violence against women: Initial results on prevalence, health outcomes and women’s responses.
Publisher | Google Scholor - Khalil A, Syngelaki A, Maiz N, Zinevich Y, Nicolaides KH. (2013). Maternal age and adverse pregnancy outcome: a cohort study. Ultrasound Obs Gynecol, 42(6):76-78.
Publisher | Google Scholor - Health AJP, Borrell LN, Rodriguez-alvarez E, Savitz DA, Baquero MC. (2016). Parental Race Ethnicity and Adverse Birth Outcomes in New York City. 106(8).
Publisher | Google Scholor - Azooz R, Al-youzbaki D. (2012). Socio-demographic background of pregnant women with newborns’ adverse pregnancy outcomes: case control study. Iraqi J Comm Med, 2012(1):9-14.
Publisher | Google Scholor - Kaplan R, Fang Z, Kirby J. (2017). Educational Attainment and Health Outcomes: Data from the Medical Expenditures Panel Survey. Heal Psychol, 4272828.
Publisher | Google Scholor - Mukherjee S, Edwards DRV, Baird DD, Savitz DA, Katherine E. (2013). Risk of miscarriage among black women and white women in a US Prospective Cohort Study. 177(11):2013-2015.
Publisher | Google Scholor - Ajiboye O, Adebayo K. (2012). Socio-Cultural Factors Affecting Pregnancy Outcome among the Ogu Speaking People of Badagry Area of Lagos State, Nigeria. Int J Humanit Soc Sci, 2:133.
Publisher | Google Scholor - Esienumoh E, Akpabio I, Etowa J, Waterman H. (2015). Cultural Diversity in Childbirth Practices in a Rural Community in Southern Nigeria. In: • Sigma Theta Tau International (Sigma) repository.
Publisher | Google Scholor - Lindquist A, Kurinczuk J, Redshaw M, Knight M. (2015). Experiences, utilisation and outcomes of maternity care in England among women from different socio-economic groups: findings from the 2010 National Maternity Survey. BJOG, 122(12):1610-1617.
Publisher | Google Scholor - Ribot B, Isern R, Canals J, Arija V. (2014). Effects of tobacco habit, second- hand smoking and smoking cessation during pregnancy on newborn’ s health. Nutr Hosp, 143(2).
Publisher | Google Scholor - Wilcox AJ, Morken N, Clarice R. (2019). Role of maternal age and pregnancy history in risk of miscarriage: prospective register based study.
Publisher | Google Scholor - Lennon SL. (2016). Risk perception in pregnancy : a concept analysis. 1-14.
Publisher | Google Scholor