Research Article
Retention in Care and Treatment Adherence to Antiretroviral Therapy (Art), And Its Associated Factors Among Pregnant and Lactating HIV Positive Women in Hawassa Public Health Facilities, Sidama, Ethiopia: Retrospective Cross-Sectional Study
1Hawassa College of Health Science, Hawassa, Ethiopia.
2School of Public Health, College of Medicine and Health Science, Hawassa University Hawassa, Ethiopia.
*Corresponding Author: Dansamo Tediso, Hawassa College of Health Science, Hawassa, Ethiopia.
Citation: Tediso D, Tafesse T, Tafese F, Tegene L Dadi. (2023). Retention in Care and Treatment Adherence to Antiretroviral Therapy (Art), And Its Associated Factors Among Pregnant and Lactating HIV Positive Women in Hawassa Public Health Facilities, Sidama, Ethiopia: Retrospective Cross-Sectional Study, Journal of Women Health Care and Gynecology, BioRes Scientia Publishers. 2(4):1-15, DOI: 10.59657/2993-0871.brs.23.015
Copyright: © 2023 Dansamo Tediso, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: September 09, 2023 | Accepted: October 31, 2023 | Published: November 04, 2023
Abstract
Background: Retention in care and treatment adherence to antiretroviral therapy (ART) among people living with HIV (PLHIV) is essential for longer existence, good quality of life, and minimizing HIV transmission. Few studies in Ethiopia were focusing more on pregnant HIV patients but it is also important to include lactating HIV positive patients as they are at risk of transmitting HIV to their child. Therefore, this study aimed to determine the level of retention in care and treatment adherence to antiretroviral therapy (ART), and its associated factors among pregnant and lactating HIV-positive women in Hawassa public health facilities, Sidama, Ethiopia, 2021.
Methods: Institution-based retrospective cross-sectional study was conducted from January 1, 2016-December 31, 2020, on a total sample size of 223. Pregnant and lactating HIV-positive women registered on the PMTCT logbook were selected by using simple random sampling techniques. Data were collected by using a structured data abstraction form. The data were entered to EpiData V4.4.2.1 and analyzed using SPSS Version 25. Bivariate and multivariate logistic regressions were undertaken to see the association between variables. Adjusted odds ratio (AOR) with 95% confidence interval (95%CI) and p-value <0.05 was used to declare the significance.
Results: The overall levels of retention in care and treatment adherence to ART were 85.7% and 88.3% respectively. Secondary and above education level [AOR =3.67, 95%CI (1.18, 11.4)], functional working status [AOR = 4.5, 95% CI (1.9, 10.82)] and HIV status disclosure to partner [AOR = 5.7, 95% CI (2.25, 14.71)] were identified as associated factors with retention in care. Baseline WHO stages I/II [AOR = 2.5, 95% CI: (1.04, 5.99)] was identified as the associated factor with treatment adherence level to ART.
Conclusions: The levels of retention in care and treatment adherence to ART in the current study were suboptimal compared to the national target. Secondary and above education level, baseline working functional status, and HIV status disclosures were associated with retention in care, whereas baseline WHO stages I/II was associated with treatment adherence. All concerned body should develop strategies on tracking lost to follow-up clients and encouraging a woman for disclosing their HV status to their partners.
Keywords: retention; adherence; ART; Hawassa; ethiopia
Background
The WHO has defined retention in care as the continuous engagement in the care from diagnosis in a package of prevention, treatment, support and care services [1]. Treatment adherence had defined as “the extent to which a person’s behavior-taking medications, following a diet and/or executing lifestyle changes-corresponds with agreed recommendations from a health care provider” [2]. Retention in care and treatment adherence to antiretroviral therapy (ART) among people living with HIV (PLHIV) are essential for longer existence, good quality of life, and minimizing HIV transmission [3]. The risk of transmission from mother to child is 15% to 45%. However, Antiretroviral therapy (ART) and other effective interventions during pregnancy, childbirth, or breastfeeding can reduce the risk below 5% [4-6]. Globally by the end of 2019, 38 million people worldwide were infected with HIV. Sub-Saharan Africa contributes over two-thirds of the global burden, with the majority of 59
Methods
Study area
The study was conducted at Hawassa town. It is located 275 Km South of Addis Ababa, the capital city of Ethiopia. The Hawassa city administration is subdivided into 8 sub-cities and the estimated total population size in 2017 was 455,658 as projected from the 2007 Ethiopian national census [25]. There are three governmental hospitals, 4 private primary hospitals, 12 health centers, and many public and private clinics and pharmacies in Hawassa town. The five facilities provide HIV care and services. HIV care and services at those facilities are provided by ART and PMTCT trained BSc midwives, nurses, health officers, doctors, and pharmacy technicians.
Study design, period, and population
Institution-based retrospective cross-sectional study was conducted from January 1, 2016-December 31, 2020. Data were retrieved from May 15-June 10, 2021. The source populations were all pregnant and lactating HIV positive women who were ever enrolled in ART at Hawassa public health facilities. The study population was all selected pregnant and lactating HIV positive women on ART from selected public health facilities who have lived at least for 6 months. Pregnant and lactating HIV positive women cards with incomplete data (date of HIV diagnosis, date of ART initiation, and outcome not recorded), and those who were start ART recently were excluded from this study.
Sample size determination and sampling technique
The sample size was determined by using a single population proportion in consideration of the following assumption: 95% confidence level, 5% margin of error, and the estimated proportion of retention in care at East Wollega, Oromia region was 74.8% [16]. Thus, n1 = z2pq/d2. Then, n1= (1.96)2 (0.7485x0.252)/ (0.05)2 =290. Given the source population (N=675) was finite and small, then (n1f) =290/1+290/675=203. By adding 10% missed records; total sample sizes of 223 were included. In Hawassa town, there are three governmental hospitals and 12 health centers. One comprehensive specialized hospital, one general hospital, and two health centers were selected out of fifteen health facilities by simple random sampling technique (lottery method). The calculated sample size (223) was proportionally allocated to the selected health facilities. Study participants' unique ART number was retrieved from the registration book and the number was used to find the PMTCT logbook, ART intake form, and medical cards and hence was used as a sampling frame. Then, within each health facility by using a simple random sampling technique, records of study participants were selected randomly by lottery method. Finally, 223 study participants’ chart was reviewed and recorded on a tool.
Data collection method and tools
The data collection was administered by 3 Bsc midwife from a study setting who was not assigned at the ART clinic was recruited for data collection. One trained health officer and the principal investigator intensively supervised the data collection process. The data was collected by using a data abstraction form adapted from the federal ministry of health (FMoH), PMTCT logbook, ART intake forms, and medical cards. Treatment adherence to ART and retention in care was assessed in three health facilities using retrospective records review. One cohort who started ART in all the 3 health facilities were traced from the health facility by retrospective record review to find out the loss to follow up within 5 years during the study period.
Data quality control
The data abstraction form was prepared in the English language. Data collectors and supervisors were trained for two days on data collection, objectives, data collection tools, record techniques and significance of the study, and checking the already filled abstraction form by the principal investigator. Pre-testing was performed at study areas to check consistency and any ambiguity of the abstraction form a week back of actual data collection and some of the deviation identified during pre-test was checked again and incorporated into the data abstraction form. Data completeness was checked by the supervisor daily and weekly by the principal investigator for completeness and missing values.
Study variables
Outcome variables: Retention in care and treatment Adherence.
Independent variables included: Socio-demographic characteristics of pregnant and lactating HIV patients(Age at start, marital status, level of education, residence, occupation of patient), Patient-related characteristics (time of ART initiated, gestation at booking, place of delivery, outcome of delivery, status of pregnancy at enrollment, partner HIV status, disclosure status), Baseline clinical and health service-related characteristics(Baseline functional status, baseline WHO clinical stage, baseline CD4 count, baseline ART regimen).
Operational definitions
Retention in care: all patients who are not recorded as deceased or lost to follow-up (LTFU) for any reason [26].
HIV patient retained in care: attending every 3 months scheduled clinic visit at month 6, 12, and 24 prior to data extraction to the ART at least 1 year from January 1, 2016-December 31, 2020 from the date enrolled.
HIV patient not retained in care: that had missed attending two or more successive scheduled visits at month 6, 12, and 24 prior to data extraction to the ART clinic at least 1 year from the date enrolled.
Treatment adherence to ART: defined as “the extent to which a client follows a prescribed medication or treatment regimen” [10]. For this study treatment adherence was measured using recorded patient self-report (PSR) at 3, 6 or 12 months.
Good adherence: If a patient took ≥95% of the expected doses of their ART a week within 3 months.
Poor adherence: If a patient took less than 95 Percentage of the expected doses of their ART a week within 3 months.
Transfer out: Included HIV patients who had officially moved to another facility by the health provider.
Lost to follow up (LTFU): Patients who had been receiving ART and had missed scheduled clinic or pharmacy appointments more than 3 months and were not known to have transferred out or died.
Data processing and analysis
The collected data was entered to EpiData V4.4.2.1 and then exported to Statistical Package for Social Science (SPSS) Version 23 for analysis. Data was coded and cleaned in SPSS V23All required variables recording and computations were done before the main analysis. Descriptive analyses (mean, standard deviation, proportion) were conducted to obtain descriptive measures for the socio-demographic characteristics and other variables. Binary logistic regression was used to identify factors associated with retention in care and treatment adherence. The bi-variable logistic regression analysis started with unadjusted analysis in which each potential predictor was assessed separately for its association with stunting [27]. Variables with p-values less than 0.25 on the unadjusted analysis were entered into a multivariable logistic regression model to find out independent risk factors of stunting adjusting for other factors in the model.
Moreover, multicollinearity was checked by using the collinearity diagnostic test by checking the value of the Variance Inflation Factor (VIF) and tolerance test. Hosmer–Lemeshow goodness-of-fit was used to test for the model fitness, and the p-value for the Hosmer-Lemeshow test was 0.49 which indicates a good model. Odds ratio at 95% CI were used to measure the strength of association between outcome and predictor variables. P-value less than 0.05 was considered to declare statistical significance in multivariate logistic regression analysis. Finally, the results were presented in texts, graphs, and tables.
Results
Socio-demographic characteristics of the pregnant and lactating HIV positive women
Two hundred twenty-three pregnant and lactating HIV patients were included in this study. The mean (±SD) age at start of ART was 26.7 (± 4.21) years with a minimum and maximum age of 15 and 38, respectively. About 62 (27.8%) belong to the age group of 25–29 years at start of ART and more than half, 144 (64.4%) were urban resident. The majority, 173(77.6%) were married, and about 71 (31.8%) were unable to write and read. More than half, 115 (52.6%) were housewives (Table 1).
Table 1: Baseline socio-demographic characteristics of pregnant and lactating HIV positive women at public health facilities of Hawassa, Sidama, Ethiopia, January 1, 2016-December 31, 2020 (n=223).
| Variables | Categories | Number (%) |
| Time ART initiated at PMTCT | ||
| Before pregnancy | 135(60.5) | |
| During pregnancy | 47(21.1) | |
| During breast feeding | 41(18.4) | |
| Gestation at booking to PMTCT | ||
| First trimester | 77(34.5) | |
| Second trimester | 88(39.5) | |
| Third trimester | 58(26) | |
| Pregnancy status at enrollment | ||
| Pregnant | 116(52) | |
| Lactating | 107(48) | |
| Delivery outcome | ||
| Live birth | 211(94.6) | |
| Still birth | 12(5.4) | |
| Current status of the patient | ||
| Pregnant | 76(34.1) | |
| Lactating | 124(55.6) | |
| Not recorded | 23(10.3) | |
| Partner HIV status | ||
| Positive | 144(64.6) | |
| Negative | 35(15.7) | |
| Unknown | 44(19.7) | |
| HIV status disclosed to partner | ||
| Yes | 180(80.7) | |
| No | 43(19.3) | |
*: Daily laborer, Student
Patient related characteristics
One hundred thirty-five (60.5%) participants were initiated ART at PMTCT before pregnancy and about 78 (34.5%) had been linked to PMTCT at third trimester. At enrollment, more than half, 118(52.9%) were pregnant, and most of, 211(94.6%) the delivery was live birth. Currently, more than half, 124(55.6%) patients were lactating. Two third, 144 (64.6%) of participants’ partner HIV status were positive and majority, 180(80.7%) patients had disclosed HIV status to their partner (Table 2).
Table 2: Patient related characteristics of pregnant and lactating HIV positive women at public health facilities of Hawassa, Sidama, Ethiopia, January 1, 2016-December 31, 2020 (n=223).
| Variables | Categories | Number (%) |
| Time ART initiated at PMTCT | ||
| Before pregnancy | 135(60.5) | |
| During pregnancy | 47(21.1) | |
| During breast feeding | 41(18.4) | |
| Gestation at booking to PMTCT | ||
| First trimester | 77(34.5) | |
| Second trimester | 88(39.5) | |
| Third trimester | 58(26) | |
| Pregnancy status at enrollment | ||
| Pregnant | 116(52) | |
| Lactating | 107(48) | |
| Delivery outcome | ||
| Live birth | 211(94.6) | |
| Still birth | 12(5.4) | |
| Current status of the patient | ||
| Pregnant | 76(34.1) | |
| Lactating | 124(55.6) | |
| Not recorded | 23(10.3) | |
| Partner HIV status | ||
| Positive | 144(64.6) | |
| Negative | 35(15.7) | |
| Unknown | 44(19.7) | |
| HIV status disclosed to partner | ||
| Yes | 180(80.7) | |
| No | 43(19.3) | |
Baseline and current clinical and health service characteristics
At baseline, the majority, 150 (67.3%) of participants were in working functional status. One hundred forty-eight, 148 (66.4%) were in stage I or II WHO clinical stage category, and two third of patients, 135 (60.5%) had > 350 cells/mm3 CD4 count. More than half, 127 (57%) were on baseline triple ART regimen containing tenofovir, lamivudine, efavirenz (TDF/ 3TC/EFV). Currently, most of, 191 (85.5%) of participants were in working functional status. About 195 (87.4%) were in WHO stage I, and one hundred ninety-seven (88.3%) had > 350 cells/mm3 CD4 count. Two third, 146 (65.5%) were on triple ART regimen containing tenofovir, lamivudine, dolutegravir (TDF- 3TC-DTG) (Table 3).
Table 3: Baseline and current clinical and health service characteristics of pregnant and lactating HIV positive women at public health facilities of Hawassa, Sidama, Ethiopia, January 1, 2016-December 31, 2020 (n=223).
| Variables | Categories | Number (%) |
| Baseline functional status | ||
| Working | 150(67.3%) | |
| Ambulatory/bed ridden | 73(32.7) | |
| Baseline WHO Stage | ||
| Stage I/II | 148(66.4) | |
| Stage III/IV | 75(33.6) | |
| Baseline CD4 level (cells/mm3) | ||
| <=200 | 41(18.4) | |
| 200-350 | 47(21.1) | |
| >350 | 135(60.5) | |
| Baseline ART regimen | ||
| TDF-3TC-EFV | 127(57) | |
| AZT-3TC-NVP | 56(25.1) | |
| AZT-3TC-EFV | 40(17.9) | |
| Current functional status | ||
| Working | 191(85.7) | |
| Not recorded | 32(14.3) | |
| Current WHO Stage | ||
| Stage I | 195(87.4) | |
| Not recorded | 28(12.6) | |
| Current CD4 level (cells/mm3) | ||
| <=200 | 10(4.5) | |
| 200-350 | 12(5.4) | |
| >350 | 197(88.3) | |
| Not recorded | 4(1.8) | |
| Current ART regimen | ||
| TDF-3TC-DTG | 146(65.5) | |
| TDF-3TC-EFV | 42(18.8) | |
| AZT-3TC+EFV | 22(9.9) | |
| Not recorded | 13(5.8) | |
The level of retention in care among pregnant and lactating HIV patients
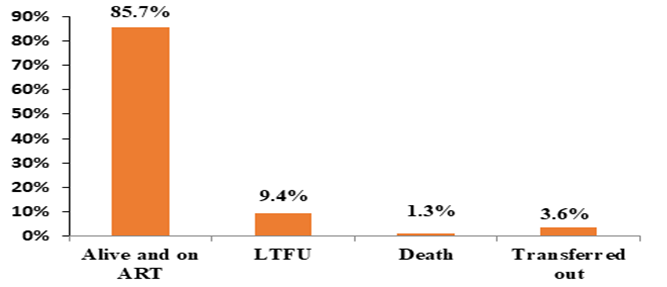
Of the 223 pregnant and lactating HIV patients had recorded, 3(1.3%) were died, 21(9.4%) were lost to follow up, 8(3.6%) were transferred to other health facility, and 191 (85.7%) (95% CI: 81%, 90%) were retained in the care during study period (Figure 1). The patient’s record was reviewed for 24 months of follow up with in study period. The HIV patients’ retention in care at 6, 12 and 24 months was 52 per 1000 person-months, 48 per 1000 person-months and 31 per 1000 person-months respectively. Of the 21 lost to follow up patients,4.1 per 1000 person-months ,5.5 per 1000 person-months and 4.8 per 1000 person-months were at 6,12 and 24 months respectively.
Figure 1: Maternal ART treatment outcome among pregnant and lactating HIV positive women at public health facilities of Hawassa, Sidama, Ethiopia, January 1, 2016-December 31, 2020.
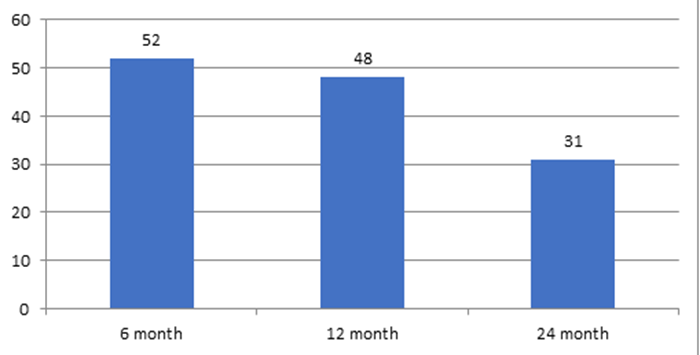
The patient’s record was reviewed for 24 months of follow up with in study period. The HIV patients’ retention in care at 6, 12 and 24 months was 52 per 1000 person-months,48 per 1000 person-months and 31 per 1000 person-months respectively (Figure 2). Of the 21 lost to follow up patients,4.1 per 1000 person-months ,5.5 per 1000 person-months and 4.8 per 1000 person-months were at 6,12 and 24 months respectively.
Figure 2: Trends of retention in care among pregnant and lactating HIV positive women.
Level of treatment adherence to ART
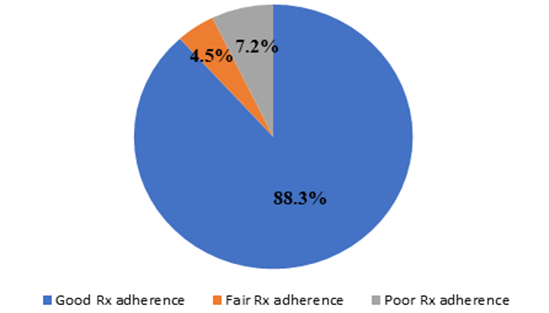
Treatment adherence to ART was measured by using records of patient self-report. Overall, of the 223 pregnant and lactating HIV patients, one hundred ninety-seven (88.3%) (95% CI: 84%, 91.2%) had good adherence, 10 (4.5 %) had fair adherence and 16(7.2%) had poor adherence (Figure 3).
Figure 3: Percentage of treatment adherence level to ART among pregnant and lactating HIV positive women at public health facilities of Hawassa, Sidama, Ethiopia, January 1, 2016-December 31, 2020.
Factors associated with retention in care to ART among pregnant and lactating HIV positive women
In the bivariate analysis, age at ART start, residence, educational status, time ART initiated at PMTCT, baseline functional status, baseline WHO stage, baseline CD4 level, partner HIV status, baseline and current ART regimen, and HIV status disclosed to their partner were important factors of retention in care to ART of pregnant and lactating HIV patients. The multivariable model revealed that educational status, baseline functional status and disclosure of HIV status had significant association with retention in care to ART among pregnant and lactating HIV patients. The pregnant and lactating HIV patients who had secondary and above educational levels were 3.67 times [AOR =3.67, 95%CI (1.18, 11.4)] more likely to retain in care of ART than mothers who were unable to write and read. This model also showed that those participants who had baseline working functional status were 4.5 times [AOR = 4.5, 95% CI (1.9, 10.82)] more likely to retain in care of ART than participants who had baseline ambulatory/bedridden functional status. Pregnant and lactating HIV patients who disclosed HIV status to their partner were 5.7 times [AOR = 5.7, 95% CI (2.25, 14.71)] more likely to retain in care to ART than those not disclosed (Table 4).
Table 4:Bivariable and Multivariable Logistic regression result on level and factors associated with retention in care among pregnant and lactating HIV positive women at public health facilities of Hawassa, Sidama, Ethiopia, January 1, 2016-December 31, 2020 (n=223).
| Retention | |||||
| Variables | Categories | Retained No (%) | Not retained No (%) | COR (95% CI) | AOR (95% CI) |
| Age at start | |||||
| 15-19 | 23(76.7) | 7(23.3) | 1 | 1 | |
| 20-24 | 47 (82.5) | 10(17.5) | 1.43(0.48-4.24) | 0.66(0.16 -2.73) | |
| 25-29 | 57(91.9) | 5(8.1) | 3.47(0.99-12.1) | 2.73(0.55 -13.45) | |
| 30-34 | 46(88.5) | 6(11.5) | 2.33(0.7-7.74) | 2.03(0.41 -10.16) | |
| >=35 | 18(81.8) | 4(18.2) | 1.37(.34-5.41) | 0.99(0.16 - 6.09) | |
| Residence | |||||
| Urban | 126(87.5) | 18(12.5) | 1.51(0.71-3.22) | 2(0.73 - 5.47) | |
| Rural | 65(82.3) | 14(17.7) | 1 | 1 | |
| Education | |||||
| Unable to read and write | 57(80.3) | 14(19.7) | 1 | 1 | |
| Grade 1-8 | 46(79.3) | 12(20.7) | 0.94(0.40-2.23) | 0.88(0.33-2.33) | |
| Grade 9-12 and above | 88(93.6) | 6(6.4) | 3.60(1.31-9.92) | 3.67(1.18- 11.4)* | |
| Time ART initiated at PMTCT | |||||
| Before pregnancy | 118(87.4) | 17(12.6) | 1.95(0.79-4.79) | 2.598(0.8- 8.35) | |
| During pregnancy | 41(87.2) | 6(12.8) | 1.92(0.62-5.96) | 3.018(0.7312.41) | |
| During breast feeding | 32(78) | 9(22) | 1 | 1 | |
| Baseline functional status | |||||
| Working | 139(92.7) | 11(7.3) | 5.10(2.3011.31) | 4.5(1.9- 10.82)* | |
| Ambulatory/bedridden | 52(71.2) | 21(28.8) | 1 | 1 | |
| Baseline WHO stage | |||||
| Stage I/II | 130(87.8) | 18(12.2) | 1.66(0.77-3.55) | 1.2(0.44- 3.24) | |
| Stage III/IV | 61(81.3) | 14(18.7) | 1 | 1 | |
| Baseline CD4 level(cells/mm3) | |||||
| <=200 | 30(73.2) | 11(26.8) | 0.42(0.18-0.98) | 0.56(0.21- 1.48) | |
| 201-350 | 44(93.6) | 3(6.4) | 2.26(0.63-8.04) | 3.49(0.83-14.71) | |
| >350 | 117(86.7) | 18(13.3) | 1 | 1 | |
| Partner HIV status | |||||
| Positive | 133(92.4) | 11(7.6) | .29(0.83- 6.31) | 2.38(0.76,7.48) | |
| Negative | 21(60) | 14(40) | 0.28(0.10-0.81) | 0.31(0.09,1.05) | |
| Unknown | 37(84.1) | 7(15.9) | 1 | 1 | |
| Baseline ART regimen | |||||
| TDF-3TC-EFV | 109(85.8) | 18(14.2) | 0.49(0.14-1.76) | 0.49(0.12- 2.05) | |
| AZT-3TC-NVP | 45(80.4) | 11(19.6) | 0.33(0.08-1.28) | 0.28(0.06- 1.23) | |
| AZT-3TC-EFV | 37(92.5) | 3(17.5) | 1 | 1 | |
| Current ART regimen | |||||
| TDF-3TC-DTG | 147(98) | 3(2) | 2.3(0.23-22.85) | 0.5(0.02-11.89) | |
| TDF-3TC-EFV | 24(61.5) | 15(38.5) | 0.9(0.1- 0.7) | 0.13(0.001-1.33) | |
| AZT-3TC-EFV | 20(95.2) | 1(4.8) | 1 | 1 | |
| HIV status disclosed to partner | |||||
| Yes | 163(90.6) | 17(9.4) | 5.14(2.3-11.45) | 5.7(2.25- 14.71) * | |
| No | 28(65.1) | 15(34.9) | 1 | 1 | |
*Indicates variables significant at P-value less than 0.05; 1: Indicates reference category
Factors associated with treatment adherence to ART among pregnant and lactating HIV positive women
In the bivariate analysis, showed that age at ART start, residence, educational status, time ART initiated at PMTCT, baseline WHO stage, baseline CD4 level, baseline and current ART regimen and HIV status disclosed to their partner were important factors of treatment adherence to ART of pregnant and lactating HIV patients. The multivariable model revealed thatbaseline WHO stage had significant association with treatment adherence to ART among pregnant and lactating HIV patients. Pregnant and lactating HIV patients who had baseline WHO stage I/II were 2.5 times [AOR = 2.5, 95% CI: (1.04, 5.99)] more likely adhere to ART treatment than those who had baseline WHO stage III/IV (Table 5).
Table 5: Bivariable and Multivariable Logistic regression result on level and factors associated with treatment adherence to ART among pregnant and lactating HIV positive women at public health facilities of Hawassa, Sidama, Ethiopia, January 1, 2016-December 31, 2020 (n=223).
| Variables | Rx adherence to ART | COR (95% CI) | AOR (95% CI) | |
| Good No (%) | PoorNo (%) | |||
| Age at start | ||||
| 15-19 | 24(80) | 6(20) | 1 | 1 |
| 20-24 | 51(89.5) | 6(10.5) | 2.12(0.62,7.28) | 1.5(0.35,6.07) |
| 25-29 | 58(93.5) | 4(6.5) | 3.62(0.94,14.01) | 3.72(0.73,18.85) |
| 30-34 | 44(84.6) | 8(15.4) | 1.37(0.43,4.43) | 1.12(0.26,4.75) |
| >=35 | 20(90.9) | 2(9.1) | 2.5(0.45,13.78) | 1.59(0.22,11.66) |
| Residence | ||||
| Urban | 132(91.7) | 12(8.3) | 2.37(1.04,5.41) | 2.19(0.92,5.22) |
| Rural | 65(82.3) | 14(17.7) | 1 | 1 |
| Education | ||||
| Unable to read and write | 62(87.3) | 9(12.7) | 1 | 1 |
| Grade 1-8 | 49(84.5) | 9(15.5) | 0.79(0.29,2.14) | 0.75(0.24,2.38) |
| Grade 9-12 and above | 86(91.5) | 8(8.5) | 1.56(0.57,4.27) | 1.42(0.44,4.56) |
| Time ART Initiated at PMTCT | ||||
| Before pregnancy | 123(91.1) | 12(8.9) | 1.42(0.47,4.31) | 1.4(0.4,4.95) |
| During pregnancy | 38(80.9) | 9(19.1) | 0.58(0.18,1.92) | 0.67(0.17,2.6) |
| During breast feeding | 36(87.8) | 5(12.2) | 1 | 1 |
| Baseline WHO Stage | ||||
| Stage I/II | 137(92.6) | 11(7.4) | 3.11(1.35,7.18) | 2.5(1.04,5.99) * |
| Stage III/IV | 60(80) | 15(20) | 1 | 1 |
| Baseline CD4 level(cells/mm3) | ||||
| <=200 | 36(87.8) | 5(12.2) | 0.7(0.23,2.13) | 0.83(0.24,2.9) |
| 201-350 | 38(80.9) | 9(19.1) | 0.41(0.16,1.05) | 0.35(0.12,1.03) |
| >350 | 123(91.1) | 12(8.9) | 1 | 1 |
| Baseline ART regimen | ||||
| TDF-3TC-EFV | 119(93.7) | 8(6.3) | 3.16(1.07,9.34) | 2.96(0.97,9.03) |
| AZT-3TC-NVP | 45(80.4) | 11(19.6) | 0.87(0.30,2.48) | 0.95(0.32,2.85) |
| AZT-3TC-EFV | 33(82.5) | 7(17.5) | 1 | 1 |
| Current ART regimen | ||||
| TDF-3TC-EFV | 134(91.8) | 12(8.2) | 3.28(1.03,10.6) | 4(0.98,17.14) |
| AZT-3TC-NVP | 36(85.7) | 6(14.3) | 1.76(0.47,6.6) | 2.6(0.48,14.2) |
| AZT-3TC-EFV | 17(77.3) | 5(22.7) | 1 | 1 |
| HIV status disclosed to partner | ||||
| Yes | 163(90.6) | 17(9.4) | 2.54(1.04,6.17) | 2.38(0.92,6.14) |
| No | 34(79.1) | 9(20.9) | 1 | 1 |
*: Indicates variables significant at P-value less than 0.05; 1: Indicates reference category.
Discussion
The overall level of retention in care to ART was 85.7%, (95% CI: 81%, 90%) in this study. This finding was consistent with other studies conducted in Gondar 88.2% and Uganda 87.9% [28,29]. However, the level of retention in care of this study was higher than the studies conducted in Ethiopia systemic review and meta-analysis (70.65%), Northern Ethiopia (70%), and Malawi (42%) [14, 16,30]. The reason for this difference might be study design, study setting, and study population. Study in Ethiopia systemic review and meta-analysis and Northern Ethiopia were among adults living with HIV/AIDS. This difference in Malawi might be due to the setting and time at which studies were conducted. In contrast, the level of retention in care of this finding was lower than the previous studies done in Cape Town South Africa 94% [31]. The reason for this difference might be countries have different socio-demographic characteristics, levels of infrastructure and HIV burden that could cause patients not to be retain in care and transfer out [32].
In this study, the educational status of women showed a statistically significant association with retention in care to ART. Pregnant and lactating HIV patients who had secondary and above education level were more likely to retain in care than mothers who were unable to write and read. This finding was consistent with previous studies conducted in East Wollega, a systematic review in low and middle-income countries, and Uganda [16,33,34]. This was explained as better access to information and self-decision making about care might be high for the women with a higher educational status that helps to retain in HIV care. According to the report of this study, baseline working functional status was significantly associated with factors of retention in care in the current study. Pregnant and lactating HIV patients who had baseline working functional status were more likely to retain in care than those who had baseline ambulatory/bedridden functional status. This finding was consistent with previous studies conducted in Ethiopia [35-38], and Zimbabwe [39]. The possible reason for this could be their ability to do their routine activity including their daily work and visit health facilities regularly [40, 41].
This study also showed that disclosure of the HIV status to their partner was significantly associated with retention in care to ART in this study. Pregnant and lactating HIV patients who disclosed their HIV status were more likely to retain in care than those who did not disclose their HIV status to their partner. This finding was consistent with previous studies conducted in East Wollega[16], Sub-Saharan Africa[33], Malawi [30], and Uganda [34]. This is due to disclosure of HIV status might help to predict and prevent inconsistent care and to have family support. Existed evidence reported as non-disclosure was associated with poor retention in care [42]. The overall level of treatment adherence to ART among pregnant and lactating HIV positive women was 88.3%, (95% CI: 84%, 91.2%) according to this study. This finding was in line with other studies conducted in Tigray Region of North Ethiopia 87.1% [18], Yirgalem Hospital, South Ethiopia 88.7% [43], South wollo Zone 87.9% [17], Kisumu Kenya 84% [44], Nigeria 89.2% [45], and Malawi 91% [46]. However, the treatment adherence level of this study was higher than the studies conducted in Southern Ethiopia 81.4% [47], Hadya Zone 83.7% [19], East Shewa Zone 82.6% [48], and Sobi Specialist Hospital, Nigeria 73.3% [39]. The reason for this discrepancy might be the study population. The studies conducted in Sobi Specialist Hospital, Ilorin, Nigeria was among the general population. Other studies conducted in Hadya Zone, East Shewa Zone, and Southern Ethiopia were only among pregnant women. Pregnant and lactating women want to have HIV-free children and have challenges like caring for their families and children than general people living with HIV/AIDS (PLHIV).
In contrast to this finding, the level of adherence was lower than a study done in Ayder referral hospital, Northern Ethiopia (95.1%) among HIV-positive pregnant women [50]. The reason for this difference might be the discrepancy in sample size and the setting in which the research was done. The sample size study at Ayder referral hospital was among forty-one HIV-positive pregnant women and it was only in one public health facility. In this study, the WHO stage of HIV/AIDS at ART initiation was a significantly associated factor with treatment adherence to ART. Pregnant and lactating HIV patients who had started the ART treatment when their WHO clinical stage I/II were more likely had a good adherence than those who had started the ART treatment when their stage III/IVs. This finding was consistent with previous studies conducted in different countries [16, 51]. The potential reason for this is, patients with advanced WHO stage could have an increased pill burden during treatment of opportunistic infections, significant weakness in attending clinic appointments, and that may create more challenges to memorize recommended ART treatment.
Limitation of the study
The strength of the study, the study tried to assess retention in care and treatment adherence to ART for pregnant and lactating HIV-positive women together and provide important insight on prevalence and associated factors. Regardless of its strengths, our study had some basic limitations that might be considered while interpreting the results. First, since the data was based on recorded patients’ chart, this was difficult to know the status of self-referred and transferred out pregnant and lactating HIV positive women. This may lead to over or underestimation of outcome interest. Second, this study only analyses maternal outcomes and we did not review data on baby outcomes, and therefore we do not have information about the mother-baby. Third, the generalizability of this study finding may be limited to the public health facilities of Hawassa. Moreover, due to a cross-sectional study, it was difficult to identify the causal-effect relationships.
Conclusions
The level of retention in care in the current study was suboptimal compared to the national target. Secondary and above education level, baseline working functional status, and HIV status disclosures were important associated factors with retention in care. In addition to this, the level of retention in care in the current study was suboptimal compared to the national target Baseline WHO stage was an important associated factor with treatment adherence.
Therefore, Hawassa comprehensive specialized hospital and city administration health department should enhance retention in care for HIV patients who were unable to read and write. Facility management should try to develop strategies on having better access to information and encouraging self-decision making. In addition, existing Information, Education and Communication (IEC) interventions on HIV/AIDS should be strengthened in order to improve HIV disclosure. Health professionals shall counsel and encourage HIV patients to disclose their HIV status to partners. Moreover, pregnant and lactating HIV patient should be advised on the importance of retention in care and adherence to antiretroviral therapy.
Abbreviations
AIDS: Acquired Human Immune Disease Syndrome; ARV: Antiretroviral; AZT: Zidovudin; EFV: Efarenz; NVP: Nevarapin; PLHIV: People Living with Human Immune- deficiency Virus; SPSS: Statistical Package for Social Science; TDF: Tenofovir; UNAIDS: United Nation Acquired Human Immune Disease Syndrome.
Declarations
Ethics approval and consent to participate
Ethical clearance was obtained from the Institutional Review Board (IRB) at the College of Medicine and Health Sciences of Hawassa University before commencing data collection (Ref. No: IRB/145/13). An official letter of permission was obtained from the Department of Public Health to the respective district health office. Informed written permission was also obtained from the district health office. All methods were carried out in accordance with relevant guidelines and regulations.
Consent for publication
Not applicable.
Competing interests
All authors declare that they have no conflicts of interest.
Availability of data and materials
The datasets used and/or analyzed during the current study available from the corresponding author on reasonable request.
Funding
The financial aid of this thesis was obtained from Hawassa College health science with specific grant numbers HSC/10123/13. Dansamo Tediso is author who received award. The funded agency did not take part in the thesis design, data collection, and manuscript preparation process.
Authors’ contributions
TD- Involved in initiation of the research question, prepared the research proposal, carried out the research, did the data entry and analysis, and wrote the manuscript. TL- conducted edition, advising, cooperatively prepared research tools with PI, and revised the manuscript. FT- conducted edition, advising, and reviewed the manuscript. TT- Did the data entry, analysis, prepared and reviewed the manuscript. All authors have read and approved the final manuscript.
Acknowledgments
Authors would like to thank the Hawassa University, School of Public Health for approval of ethical clearance. The authors are also very grateful for data collectors.
References
- (2012). Retention in HIV programmes: defining the challenges and identifying solutions: meeting report, 13-15 September 2011. Geneva: World Health Organization.
Publisher | Google Scholor - (2003). Adherence to long-term therapies: evidence for action. WHO.
Publisher | Google Scholor - Umeokonkwo CD, Onoka CA, Agu PA, Ossai EN, Balogun MS, Ogbonnaya LU. (2019). Retention in care and adherence to HIV and AIDS treatment in Anambra State Nigeria. BMC infectious diseases,19(1):654.
Publisher | Google Scholor - (2018). Federal ministry of health(FMoH), Federal HIV/AIDS Prevention and Control Office(FHAPCO),United nation population fund agency(UNFPA),Joint United nations on HIV/AIDS(UNAIDS). Ethiopian National consolidated guidelines for comprehensive HIV prevention, care and treatment.
Publisher | Google Scholor - Abtew S, Awoke W, Asrat A. (2016). Knowledge of pregnant women on mother-to-child transmission of HIV, its prevention, and associated factors in Assosa town, Northwest Ethiopia. Hiv/Aids, 8:101-107.
Publisher | Google Scholor - World Health Organization (WHO). (2017). 'Mother-to-child transmission of HIV'.
Publisher | Google Scholor - Global HIV statistics.
Publisher | Google Scholor - World Health Organization. (2017). Global Guidance on Criteria and Processes for Validation: Elimination of Mother-To-Child Transmission of HIV and Syphilis.
Publisher | Google Scholor - Luzuriaga K, Mofenson LM, Campion EW. (2016). Challenges in the elimination of pediatric HIV-1 infection. N Engl J Med, 374 (8):761-770.
Publisher | Google Scholor - Central Statistical Agency (CSA) [Ethiopia] and ICF. 2016.Ethiopia Demographic and Health Survey 2016: Key Indicators Report. Addis Ababa, Ethiopia, and Rockville, Maryland, USA. CSA and ICF.
Publisher | Google Scholor - Holtzman CW, Shea JA, Glanz K, Jacobs LM, Gross R, Hines J, et al. (2015). Mapping patient-identified barriers and facilitators to retention in HIV care and antiretroviral therapy adherence to Andersen's Behavioral Model. AIDS care, 27(7):817-828.
Publisher | Google Scholor - World helath organization(WHO) Africa. (2016). Prevention of mother-to-child transmission - Technical update.
Publisher | Google Scholor - Lisa L JM, Christian Mpody, Marcel Yotebieng, Pamela M, Kate Clouse, Lindah Otieno,, wools-Kaloustian CRaK. (2018). Achieving UNAIDS 90-90-90 targets for pregnant and postpartum women in sub-Saharan Africa: progress, gaps and research needs. Journal of virus eradication, 2(4):33-39.
Publisher | Google Scholor - Tsegaye R, Etafa W, Wakuma B, Mosisa G, Mulisa D, Tolossa T. (2020). The magnitude of adherence to option B plus program and associated factors among women in eastern African countries: a systematic review and meta-analysis. BMC public health, 20(1):1812.
Publisher | Google Scholor - Assefa Y, Kiflie A, Tesfaye D, Haile Mariam D, Kloos H, Wouters E, et al. (2011). Outcomes of antiretroviral treatment program in Ethiopia: Retention of patients in care is a major challenge and varies across health facilities. BMC health services research, 11:81.
Publisher | Google Scholor - Tolossa T, Mulisa D, Fetensa G, Fekadu G. (2020). Magnitude and factors associated with lost to follow-up among women under option B+ PMTCT program at East Wollega public health facilities, western Ethiopia. International Journal of Africa Nursing Sciences,13:100212.
Publisher | Google Scholor - Tsegaye D DL, Wodajo S. (2016).Level of Adherence and Associated Factors to Option B+ PMTCT among Pregnant and Lactating Mothers in Selected Government Health Facilities of South Wollo Zone, Amhara Region, North East Ethiopia2016 Epidemiol Health. 38.
Publisher | Google Scholor - Ebuy H, Yebyo H, Alemayehu M. (2015). Level of adherence and predictors of adherence to the Option B+ PMTCT program in Tigray, northern Ethiopia. International Journal of Infectious Diseases, 33:123-129.
Publisher | Google Scholor - Lodebo TM, Suloro JA. (2017). Level of Adherence and Associated Factors to Option B+ PMTCT among HIV Positive Pregnant Women in Hadiya Zone, Southern Ethiopia. Global Journal of Health Sciences, 2(1):39-58.
Publisher | Google Scholor - Joint United Nations Programme on HIV/AIDS (UNAIDS). .2025 AIDS Targets, Ending the AIDS Epidemic by 2030,
Publisher | Google Scholor - (2015). Joint United Nations Programme on HIV/AIDS. UNAIDS 2016–2021 strategy: on the fast-track to end AIDS. UNAIDS Geneva.
Publisher | Google Scholor - Chaka TE, Abebe TW, Kassa RT. (2019). Option B+ prevention of mother-to-child transmission of HIV/AIDS service intervention outcomes in selected health facilities, Adama town, Ethiopia. HIV/AIDS (Auckland, NZ), 11:77-82.
Publisher | Google Scholor - (2021). Health Sector Transformation Plan II 2020/21-2024/25.
Publisher | Google Scholor - Abdisa S, Tenaw Z. (2021). Level of adherence to option B plus PMTCT and associated factors among HIV positive pregnant and lactating women in public health facilities of Hawassa city, Southern Ethiopia. PLoS ONE, 16(8): 0255808.
Publisher | Google Scholor - (2013). Central Statistical Agency of Ethiopia. Population Projection for all regions at wereda level from 2014–2017, Addis Ababa, Ethiopia: Central Statistical Agency.
Publisher | Google Scholor - Assefa Y, Worku A, Wouters E, Koole O, Haile Mariam D, Van Damme W. (2012). Simplified tools for measuring retention in care in antiretroviral treatment program in Ethiopia: cohort and current retention in care. PloS one, 7(6):38555.
Publisher | Google Scholor - Zoran B, Heath G, David KW, David WH. (2008). Purposeful selection of variables in logistic regression. Source Code for Bio Med, 3:17.
Publisher | Google Scholor - Masereka E.M NTD, Osingada C. P,Wiltshire C.S, A.N CBK. (2019). Increasing retention of HIV positive pregnant and breastfeeding mothers on option-B plus by upgrading and providing full time HIV services at a lower health facility in rural Uganda. BMC public health, 19.
Publisher | Google Scholor - Wubshet M, Berhane Y, Worku A, Kebede Y, Diro E. (2012). High loss to followup and early mortality create substantial reduction in patient retention at antiretroviral treatment program in north-west ethiopia. Isrn Aids, 721720.
Publisher | Google Scholor - Bigirimana F, Owiredu MN, Nuwagira I. (2016). Prevention of mother-to-child transmission technical update: implementing the ‘treat all’approach among pregnant and breastfeeding women living with HIV in the WHO African region. Victoria: Bigirimana.
Publisher | Google Scholor - Toit E, van Schalkwyk C, Dunbar R, Jennings K, Yang B, Coetzee D, et al. (2014). Missed Opportunities for Retention in Pre-ART Care in Cape Town, South Africa. PloS one, 9:96867.
Publisher | Google Scholor - Gesesew HA, Tesfay Gebremedhin A, Demissie TD, Kerie MW, Sudhakar M, Mwanri L. (2017). Significant association between perceived HIV related stigma and late presentation for HIV/AIDS care in low and middle-income countries: A systematic review and meta-analysis. PloS one, 12(3):0173928.
Publisher | Google Scholor - Hodgson I, Plummer ML, Konopka SN, Colvin CJ, Jonas E, Albertini J, et al. (2014). A systematic review of individual and contextual factors affecting ART initiation, adherence, and retention for HIV-infected pregnant and postpartum women. PloS one, 9(11):111421.
Publisher | Google Scholor - Kiwanuka G, Kiwanuka N, Muneza F, Nabirye J, Oporia F, Odikro MA, et al. Retention of HIV infected pregnant and breastfeeding women on option B+ in Gomba District, Uganda: a retrospective cohort study. BMC infectious diseases, 18(1):533.
Publisher | Google Scholor - Abebe Moges N, Olubukola A, Micheal O, Berhane Y. (2020). HIV patients retention and attrition in care and their determinants in Ethiopia: a systematic review and meta-analysis. BMC infectious diseases,1(20):439.
Publisher | Google Scholor - Wubshet M, Berhane Y, Worku A, Kebede Y, Diro E. (2012). High loss to followup and early mortality create substantial reduction in patient retention at antiretroviral treatment program in north-west ethiopia. Isrn Aids, 721720.
Publisher | Google Scholor - Tiruneh Y, Galárraga O, Genberg B, Wilson I. (2016). Retention in Care among HIV-Infected Adults in Ethiopia, 2005– 2011: A Mixed-Methods Study. PloS one,11:0156619.
Publisher | Google Scholor - 38.Mekuria LA, Prins JM, Yalew AW, Sprangers MA, Nieuwkerk PT. (2015). Retention in HIV Care and Predictors of Attrition from Care among HIV-Infected Adults Receiving Combination Anti-Retroviral Therapy in Addis Ababa. PloS one, 10(6):0130649.
Publisher | Google Scholor - Makurumidze R, Mutasa-Apollo T, Decroo T, Choto RC, Takarinda KC, Dzangare J, et al. (2019). Retention and predictors of attrition among patients who started antiretroviral therapy in Zimbabwe’s National Antiretroviral Therapy Programme between 2012 and 2015. bioRxiv, 750232.
Publisher | Google Scholor - Makurumidze R, Mutasa-Apollo T, Decroo T, Choto RC, Takarinda KC, Dzangare J, et al. (2019). Retention and predictors of attrition among patients who started antiretroviral therapy in Zimbabwe’s National Antiretroviral Therapy Programme between 2012 and 2015. bioRxiv, 750232.
Publisher | Google Scholor - Rosita Dewi A, Hartati Eko W, Tika Dwi T. (2021). Functional Status and Incidence of Loss to Follow-up after Antiretroviral Therapy Initiation. KnE Life Sciences, 6(2).
Publisher | Google Scholor - Elopre L, Hook EW, Westfall AO, Zinski A, Mugavero MJ, Turan J, et al. (2015). The Role of Early HIV Status Disclosure in Retention in HIV Care. AIDS patient care and STDs. 29(12):646-650.
Publisher | Google Scholor - Markos E, Worku A, Davey G. (2016). Adherence to ART in PLWHA at Yirgalem Hospital, South Ethiopia. The Ethiopian Journal of Health Development, 22(2).
Publisher | Google Scholor - Okonji JA, Zeh C, Weidle PJ, Williamson J, Akoth B, Masaba RO, et al. (2012). CD4, viral load response, and adherence among antiretroviral-naive breast-feeding women receiving triple antiretroviral prophylaxis for prevention of mother-to-child transmission of HIV in Kisumu, Kenya. Journal of acquired immune deficiency syndromes, 61(2):249-257.
Publisher | Google Scholor - Joseph A, Ogah O, Robinson O, Matthew N, chukwuemeka U, Ikeola A. (2018). Determinants of Adherence to Antiretroviral Therapy among HIV-Positive Women Accessing Prevention of Mother to Child Transmission Services in Ebonyi State, Nigeria. Annals of Medical and Health Sciences Research, 8.
Publisher | Google Scholor - Ng’ambi W, Tweya H, Speight C, Man-Bourdon C, Hosseinpour M, Phiri S, (2013). editors. Determinants of antiretroviral treatment adherence among women accessing PMTCT “Option B+”: a retrospective study at Bwaila Hospital, Malawi. IAS Conference on HIV Pathogenesis, treatment and prevention.
Publisher | Google Scholor - Tesfaye DJ, Hibistu DT, Abebo TA, Asfaw FT, Lukas K, Laelago T, et al. (2019). Option B plus antiretroviral therapy adherence and associated factors among HIV positive pregnant women in Southern Ethiopia. BMC Pregnancy and Childbirth, 19(1):82.
Publisher | Google Scholor - Tarekegn M, Baru A, Seme A. (2019). Levels of option B+ ART drugs adherence and associated factors among pregnant women following ART services at public health facilities of East Shawa Zone, Oromia, Ethiopia. Sexual & reproductive healthcare : official journal of the Swedish Association of Midwives. 22:100459.
Publisher | Google Scholor - Bello SI. (2011). HIV/AIDS Patients' Adherence to Antiretroviral Therapy in Sobi Specialist Hospital, Ilorin, Nigeria. The Journal of medical research, 11.
Publisher | Google Scholor - Shibabaw A, shibabaw w, Melkam W. (2018). Adherence to Anti-retroviral Therapy among HIV Positive Pregnant Women in Ayder Refferal Hospital, Northern Ethiopia. Journal of Antivirals & Antiretrovirals, 10.
Publisher | Google Scholor - World health organization(WHO). (2017). Guidelines Approved by the Guidelines Review Committee. Guidelines for Managing Advanced HIV Disease and Rapid Initiation of Antiretroviral Therapy. Geneva: World Health Organization
Publisher | Google Scholor