Case Report
Rare Presentation of Liver Hydatid Cyst in the Porta Hepatics: Report Five Cases and Review of Literature
- Manouchehr Aghajanzadeh 1*
- Afshin Shafaghi 2
- Omid Mosafaii Rad 3
- Mohaya Farzin 4
- Reza Shiezad 4
- Zahra Sadin 3
1Department of Thoracic and General Surgery, Aria Hospital, Guilan University of Medical Sciences, Rasht, Iran.
2Department of gasteroentrology, Guilan University of Medical Sciences, Rasht, Iran.
3Department of Internal Medicine, Inflammatory Lung Diseases Research Center, Razi Hospital, School of Medicine, Guilan University of Medical Sciences, Rasht, Iran.
4Department of physiology, Razi Clinical Research Development Center, Guilan University of Medical Sciences, Rasht, Iran.
*Corresponding Author: Manouchehr Aghajanzadeh, Department of Thoracic and General Surgery, Aria Hospital, Guilan University of Medical Sciences, Rasht, Iran.
Citation: Aghajanzadeh M, Shafaghi A, Rad O M, Farzin M, Shiezad R, et, al. (2024). Rare Presentation of Liver Hydatid Cyst in the Porta Hepatics: Report Five Cases and Review of Literature. Clinical Research and Reports, BioRes Scientia Publishers. 3(1):1-8. DOI: 10.59657/2995-6064.brs.24.042
Copyright: © 2024 Manouchehr Aghajanzadeh, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: September 20, 2024 | Accepted: October 15, 2024 | Published: October 31, 2024
Abstract
Echinococcosis remains a significant health hazard in endemic areas, including the Middle East, Mediterranean countries and Central Asia. The liver is the most common organ involved in the Hydatid Cyst (75%). Theoretically, any lobe could be involved. However, the right lobe is more common. The involvement liver dome or posterior segment (7th and 8th segment) s and potahepati has not been studied well. Humans are accidental infected and do not have any role in the life cycle of hydatid cysts .the parasite may infest any organ of the body, with the liver and lungs being the most involved organs. portahepatis involvement by hydatid cyst is extremely rare with only seven cases published in review of literatures, We present two man with 56 and 62-year-old Persian male and two old female with RUQ pain and ultrasonography (US), computed tomography (CT) and magnetic resonance imaging (MRI) findings show hydatid disease of the liver with compress of portal vein ,hepatic artery and CBD . Others organs were intact. there laboratory tests show milled elevation of ALT, AST (98,89 to 120 to 150 mg) and bilirubin(2.5to3.5mg), alkaline phosphatase was (482 to 650mg). Others lab date was in normal ranges. The patients is underwent surgery with laparotomy. After valling of the surgery site with sponge and hyper tonic salin, cysts were aspirated and evacuated and cavity filled with omentum(omentoplasty). Hydatid disease is imposing a significant burden on health care systems specifically in developing countries. Manifestations of the disease are often non-specific, while a subset of the infected population remains asymptomatic. Portohepatis obstruction and compressions a rare complication, and it is important to distinguish others cause of obstruction. the management of these entities requires different approaches. Our approach was surgery with albendasol postoperative.
Keywords: echinococcosis granulosus; hydatid cyst; portahepates hydatid cyst; compression
Introduction
Hydatid disease is a serious health and infection problem in world especially in endemic countries [1,2,3]. There are reports from several countries, which this disease is endemic in the Mediterranean region, Far East, South America, and Middle East such as Iran [1, 2, 3, 4]. It is a parasitic infection caused by the Echinococcus granulosus [1, 2]. Humans are accidental infected and do not have any role in the life cycle of hydatid cysts [2, 3.4]. Humans are infected by eggs of this parasite from vegetable, soil or water which contaminated by the dogs feces [1, 2, 3, 4]. Hydatid cysts may involve all organ in the body but occur most frequently in the liver (50%–77%) and lungs (18%–35%), and occasionally in other organs [1, 2, 3, 4, 5, 6]. However, the right lobe is more common [2,3]. The involvement of liver dome or posterior segment (7th and 8th segment) and portahepatis has not been studied well [12]. Concomitant liver and pulmonary hydatid cysts occur in 4%%of patients [1, 4]. Hydatid cyst may present as a chronic disease and asymptomatic [2, 3, 5] or may be found during routine clinical examination and serologic, radiographic, or ultrasonography for others problem [ 2,3,5, 6, 7, 9]. The clinical signs and symptoms of hydatid cysts depend on locations in the organs (deep or superficial, right and left lobe or portahepatis), size, adjacent organs, and complications such as infection or cyst rupture in the pritional cavity, intrabiliary, in the pleural or lung parachimal and rarely intra pericardial cavity or compression of portahepatis and bacterial infection [1, 2, 4, 5,7, 8,10]. The presence of air forming an air fluid level inside the cyst on CT-scan, this finding indicate the infection of the cyst [11]. The clinical status of the patient imagines finding will contribute to the final diagnosis in cases of infection of the cyst which present as a hepatic abscess [10-11]. The compression and displacement of biliary ducts can frequently produce a spontaneous rupture in biliary ducts obstructive jaundice [7,11].
A cyst may rupture into the biliary systems, Into the hollow organ, through the diaphragm into the pleural cavity or pulmonary parenchyma, or directly in the peritoneal cavity [4, 5, 6, 8, 12]. Rupture of the cyst may occur after trauma or spontaneously due to suddenly increased intracystic pressure or during treatment whit Albedasol [4, 6, ,7,8,9]. A hydatid cyst rupturing into the peritoneal cavity or may cause some symptoms including abdominal pain, urticaria, anaphylaxis, and sudden death or shoulder pain due to irritation of diaphragm [7-8-9] ). Presentation is usually dramatic with acute abdominal signs, such as guarding, rebound, and tenderness [1, 3, 5, 7, 8, 9]. In this case series, we want to show clinical presentation, diagnosis, surgical approach, mortality, morbidity and recurrences of patient who had hydatid cyst in the potahepatis with complications.
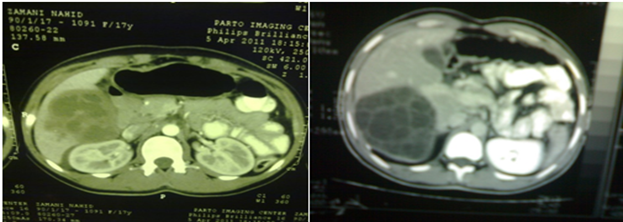
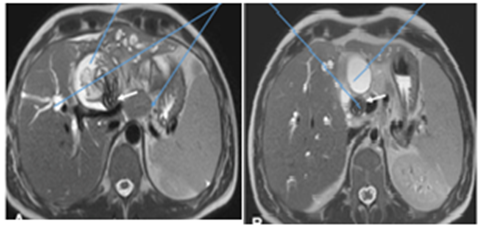
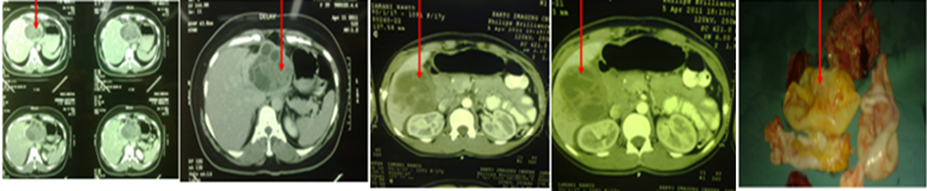
Case presentation 1
A 42-year-old femail was referred to our clinic with liver cyst which found during because of RUQ pain fever, jaundice, nausea and vomiting. There was no history of pain, Physical examination show RUQ tenderness. Routine blood vestigation, liver function (ALT and =98mg and AST=86 mg-L),total bilobren(3mg-l Direct=2mg-L and indirect 1 mg-L,AKP=342mg-L) ,WBC=12462 ,HB=12mg-L and renal function tests were normal. Past medical history was non-significant. ultrasonography (US) Computed tomography of the abdomen showed cystic lesion with separation on the portohepatis which this finding of imaging indicates a very rare location site in liver hydatid cyst (Figure. 1, Figure. 2–3). In MREP, porta hepatics as common bile duct was milled dilated. Intrahepatic bile ducts have a normal appearance. This case was brought up in a multidisciplinary committee and they decided one week Albendazole therapy followed by operative exploration with midline laparotomy for aspiration and evacuation of the cyst with omentoplasthy and intracavity drainage . However, the patient was discharged due to not having consent to undergo surgery and is being followed up for a 6-month-long period and Albendazole therapy in this period.
Figure 1
Figure 2
Figure 3
Case presentation 2
A 52-year-old mail was referred to our hospital with liver cyst porta hepatis which found during because of RUQ pain , nausea and vomiting. There was no history of abdominal pain, Physical examination show RUQ tenderness with deep compression. Routine blood examination, liver function (ALT and =48mg and AST=56 mg-L), total bilobren(2mg-l Direct=1.5mg-L and indirect .5 mg-L,AKP=142mg-L) ,WBC=8462 ,HB=12mg-L and renal function tests were normal. Past medical history was non-significant. ultrasonography (US) and Computed tomography of the abdomen showed cystic lesion with separation on the porta hepatis which this finding of imaging’s shows a very rare location of cysts in the liver (Figure. 1, Figure. 2–3). In MRCP, porta hepatics as common bile duct was normal and intrahepatic bile ducts have a normal appearance. After consultation others college and they decided one week prophylaxis with Albendazole therapy followed by with operative exploration with midline laparotomy for aspiration and evacuation of the cyst with omentoplasthy , capitonnage with carfully to prevention of porta hepatis elements and external intracavity drainage . However, the patient was discharged four days postoperative and is being good condition followed up for a 6-month-long period and Albendazole therapy in three cycles of 28 day with 14 day inter wall.
Figure 1
Figure 2
Figure 3
Case presentation 3
A 32-year-old female was referred to our thoracic surgery clinc with liver cyst because of RUQ pain, fever, jaundice, nausea and vomiting. There was no medical problem in the past history of patient, Physical examination show RUQ tenderness, fever =39 c and sclera was yellow .Routine blood examination show, liver function (ALT and =108mg and AST=122 mg-L),total bilobren(4mg-L, Direct=3mg-L and indirect 1 mg-L,AKP=422mg-L) ,WBC=462 ,HB=12mg-L,PT,PTT,INR and renal function tests were normal. Past medical history was non-significant. ultrasonography (US) Computed tomography of the abdomen showed cystic lesion with separation on the portohepatis which imaging finding show i a very rare location of hydatid cyst in the liver (Figure. 1, Figure. 2–3). In MREP, porta hepatics element as common bile duct and intrahepatic duct was dilated (Figxx). This case was consulted with gastroenterologist and infection department and they decided to surgery for decompression of the porta hepatic for evacuation of cyst. Midline laparotomy was performed and aspiration and evacuation of the cyst with omentoplasty and external drainage of intracavity was performed. However, the patient was discharged six days postoperative with 800 mg Albendasol daily for three cycles of 28 day with 14-day rest. Patient followed up for a 6-month the condition was good.
Figure 1
Figure 2
Figure 3
Case presentation 4
A 48-year-old male was referred to our thoracic surgery wared with hydatid cyst of liver because of epigastric pain, no appetite fever, nausea and vomiting . sclera icteric and urine was yellow.Past medical history and drug history was non-significant Past . Physical examination show RUQ and epigastric tenderness, fever =38 c and sclera was yellow .Routine blood tests show, liver function (ALT and =98mg and AST=72 mg-L),total bilobren(3mg-L, Direct=1.8mg-L and indirect 1.2 mg-L,AKP=522mg-L) ,WBC=11624 ,HB=12mg-L,PT,PTT,INR and renal function tests were normal and urinalysis was positive for bilirubin. ultrasonography (US) Computed tomography of the abdomen showed cystic lesion with sepatation on the porta hepatic. Imaging finding show a very rare site of hydatid cyst in the liver (Figure. 1, Figure. 2–3). In MRCP, show porta hepatics element as common bile duct and intrahepatic duct was dilated (Figxx). This case was consulted with gastroenterologist department and they recommended surgical approached for decompression of porta hepatic cyst by evacuation of cyst. Midline laparotomy was performed after vialling of the cyst with sponge wet with hypertonic saline, aspiration and evacuation of the cyst contains was performed and remnant cavity after evacuation was obliterated by omentoplasty and capitonage. patient was discharged on five days postoperative with 800 mg Albendasol daily for three cycles of 28 day with 14-day rest. Patient followed up for a 4 to 8-month the condition was good.
Figure 1
Figure 2
Figure 3
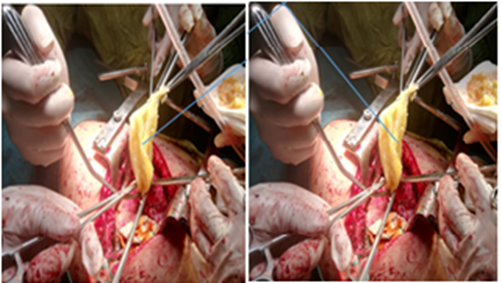
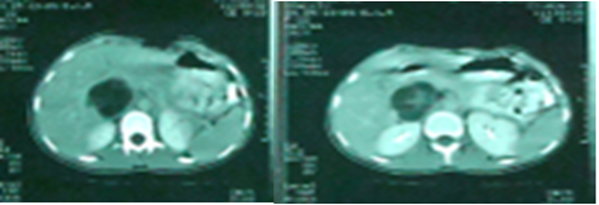
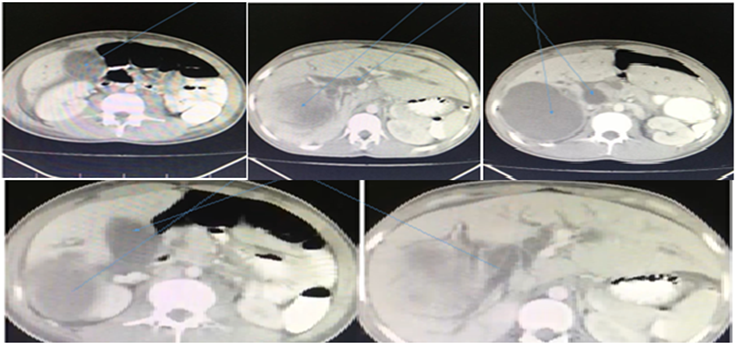
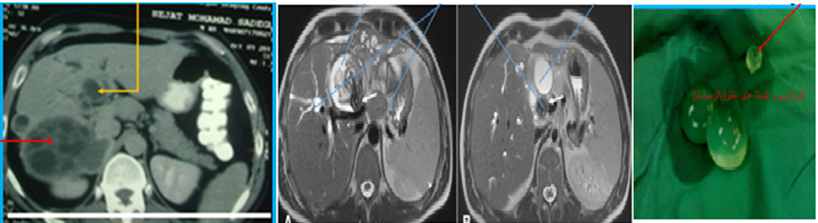
Case presentation 5
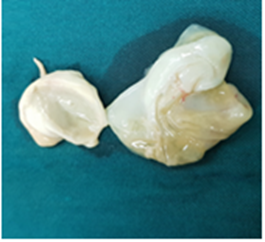
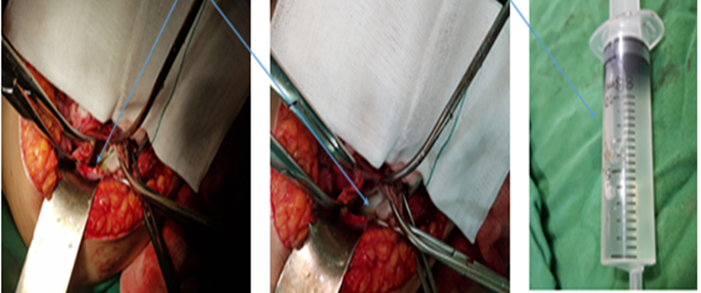
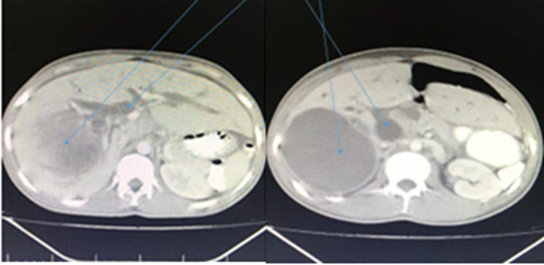
A 42-year-old male was referred to our clinic with liver cyst because of RUQ pain, fever, jaundice, nausea letargy,and vomiting. There was no medical problem in the past history , Physical examination show RUQ tenderness,fever =39 c and sclera and urin was yellow .Routine blood examination show, liver function (ALT and =148mg and AST=142 mg-L),total bilobren(5mg-L, Direct=4mg-L and indirect 1 mg-L,AKP=482mg-L) ,WBC=14620, HB=12mg-L,PT,PTT,INR and renal function tests were normal. Past medical history was non-significant. ultrasonography (US) Computed tomography of the abdomen showed cystic lesion with separation on the hill of liver which imaging finding show a very rare location of hydatid cyst in the liver (Figure. 1,2,3,4). In MREP, porta hepatics element as common bile duct and intrahepatic duct was dilated. This case was consulted with gastroenterologist and infection department and they decided to surgery for decompression of the porta hepatic for evacuation of cyst. Midline laparotomy was performed and aspiration and evacuation of the cyst with omentoplasty and external drainage of intracavity was performed(Figure 5, 6). However, the patient was discharged six days postoperative with 800 mg Albendasol daily for three cycles of 28 day with 14-day rest. Patient followed up for a 6-month the condition was good.
Figure 1,2,3,4: CT-scan show cystic lesion of porto hepatis
Figure 5,6: show laminated membrane and doughter cysts
Discussion
Hydatid disease is a serious health and infection problem in endemic countries [1,2,3,4] Although reported from several countries, the disease is endemic in the Mediterranean region, Far East, South America, and Middle East such as Iran [1,2,3]. It is a parasitic infection caused by the larval stage of Echinococcus granulosus [1-3]. It is caused by the larval stage of Echinococcus granulosus [1-8]. Dogsarethe definitive hosts and human arinvolve incidentally and cannot transmit these disease [2-4]. Human become hosts accidentally by ingestion of contaminated foods, then ovules of E. granulosus are released within the duodenum and upper part of jejunum. Concomitant liver and pulmonary hydatid cysts occur in 4% to 25% of patients with hydatid disease [1,8]. Complications occur in 5% to 40% patients with liver hydatid cysts and include cyst rupture into the biliary tree, compression of biliary duct (porta hepatic element), cyst infection, allergy and anaphylactic reactions and intraperitoneal rupture, rupture in the pleural cavity and pulmonary parenchymal [1,4,12].in our for cases liver hydatid cysts location was in the porta hepatic and compress Subhepatic artery and portal vein, this complication is very rare in the literature review. The rupture of a liver hydatid cyst into the peritoneal cavity ranges from 1% to 16% [1,2,3,4,5,8,10]. Rupture may result from trauma or may occur spontaneously during treatment with albendasol [3-6,9]. The risk factors predisposing to rupture include young age, cyst diameter >10 cm, superficial cyst location, large cyst diameter, which increases the internal cyst pressure and superficial location of the cyst are prone to rupture, even with minor trauma [4-6,8,10]. This rarity in this location of cyst in porta hepatic can compress and elevation pressure within the porta hepatic system [13] The complication of this location of liver hydatid cyst is very uncommon, and to our knowledge, this specific involvement in review of literature was rare in Spanish literature, there was uncommon [16]. In our papers in journals this event is very rare [1,2,5,6,7,8]. Liver hydatid cyst can produce serious complications and include: cyst rupture in biliary system ,pleural space ,pulmonary parenchymal and in the pritional cavity, widespread infections, [16,17]. We report all of above complications in the journals but we don’t report porta hepatic cases [1,3,4,8] Diagnosed tools are US, CT –scan and in rare case MRCP [1,2,3,4]. Treatment options for the of these cysts include surgical resection, medical treatment (Albendasol) [1,2,3,12,16 ,17,18], All of our four-case undergoing surgery with good results and complication. Our approaches were midline laparotomy, aspiration, evacuation and capitinnage and external drainage
Conclusion
compression of the porta hepatic by hydatid cysts is a rare complication. However, the diagnosis and management of this complications not defined. US, CT-scan, MRI and MRCP can help the diagnosis Managing of this complication is surgery necessitates and need best approach to prevent to damage porta hepatic element as portal vein, CBD and hepatic artery intraoperative during aspiration, evacuation and capitinnage.
Statement of ethical approval
The study was performed in accordance with the declaration of Helsinki and approved by the Ethics Committee of Local Ethical Committee of Arya private hospital. Iran, Rasht, Guilan.
References
- Manouchehr Aghajanzadeh, Mohammad Taghi Ashoobi, Hossein Hemmati, Pirooz Samidoust, Mohammad Sadegh Esmaeili Delshad and Yousha Pourahmadi. (2021). Intrabiliary and abdominal rupture of hepatic hydatid cyst leading to biliary obstruction, cholangitis, pancreatitis, peritonitis and septicemia: a case report. J Med Case Reports, 15:31.
Publisher | Google Scholor - Ouadii Mouaqit, Abdelaziz Hibatallah, Abdelmalek Ouss aden, Khalid Maazaz and Khalid Ait Taleb. (2013). Acute intraperitoneal rupture of hydatid cysts: a surgical experience with 14 cases, Ouadii Mouaqit1, 2, Abdelaziz Hibatallah, Abdelmalek Oussaden, Khalid Maazaz and Khalid Ait Taleb. World Journal of Emergency Surgery, 8:28.
Publisher | Google Scholor - Manouchehr Aghajanzadeh, Sayid Ali Glali1, Palizkar, Alireza Jafari, and Shima Ildari. (2018). Intraperitoneal Rupture of Liver Hydatid Cyst: Presented with Sever Right Shoulder and Mild Abdominal Pain. Ann Clin Cytol Pathol, 4(4):11091.
Publisher | Google Scholor - Aghajanzadeh M, Safarpoor F, Amani H, Alavi A. (2008). One-Stage Procedure for Lung and Liver Hydatid Cysts. Asian Cardiovasc Thorac Ann, 16:392-395.
Publisher | Google Scholor - N. Symeonidis, T. Pavlidis, M. Baltatzis, K. Ballas, K. Psarras, G. Marakis, and A. Sakantamis. (2013). Complicated Liver Echinococcosis: 30 Years of Experience from an Endemic Area. Scandinavian Journal of Surgery, 102(3):171-177.
Publisher | Google Scholor - Gulalp B, Koseoglu Z, Toprak N, Satar S, Sebe A, Gokel Y, et al. (2007). Ruptured hydatid cyst following minimal trauma and few signs on presentation. Neth J Med, 65:117-118 .
Publisher | Google Scholor - Kurt N, Oncel M, Gulmez S, et al. (2003). Spontaneous and traumatic intraperitoneal perforations of hepatic hydatid cysts: a case series. J Gastrointest Surg, 7:635-641.
Publisher | Google Scholor - Manouchehr Aghajanzadeh, Mohammad Rasoul Herfatkar, Farzad Ghotbi, Gohar shrieha, Bahareh Mohtasham, and Omid Mosafaiee. (2018). Ruptured Hydatid Cyst of Liver and Huge Pulmonary Hydatid cyst: Presented as Acute Abdomen with Severe Anaphylaxis Shock: A Rare Presentation. Ann Clin Pathol, 6(1):1131.
Publisher | Google Scholor - Di Cataldo A, Lanteri R, Caniglia S, et al. (2005). A rare complication of the hepatic hydatid cyst: intraperitoneal perforation without anaphylaxis. Int Surg, 90:42-44.
Publisher | Google Scholor - Akcan A, Sozuer E, Akyildiz H, et al. (2010). Predisposing factors and surgical outcome of complicated liver hydatid cysts. World J Gastroenterol, 16:3040-3048.
Publisher | Google Scholor - Chautems R, Buhler LH, Gold B, et al. (2005). Surgical management and long-term outcome of complicated liver hydatid cysts caused by Echinococcus granulosus. Surgery, 137:312-316.
Publisher | Google Scholor - Manouchehr Aghajanzadeh Mohammad reza Asgary Ali Alavi Foumani. (2014). Surgical Sara Massahnia Management of pleural Complications of Lung and Liver Hydatid Cysts in 34 Patients. International Journal of Life Sciences, 8(4).
Publisher | Google Scholor - G Ertan, S Ulus, R Kilicarslan, M Yilmaz, Y Paksoy, C. Erol. (2019). Hydatid disease of the liver with portal vein invasion mimicking portal vein. Arab J Gastroenterol, 20(1):50-52.
Publisher | Google Scholor - Mohammad Abdollahi, Neda Karkeabadi, Mahdipursafar, Yousha Pourahmadi, Vahab Rezaee, Manoucher Aghajanzadeh. (2019). Liver Dome Hydatid Cyst Management: Laparotomy or Thoracotomy. P J M H S, 13(1).
Publisher | Google Scholor - E Spanou, K Tzanetou, A Foutris, G Panetsos, S Giannou, A. (2006). Archimandritis Hydatid disease of the liver causing cavernous transformation of portal vein and portal hypertension, Acta Microbiologica Hellenica, 51(4):17.
Publisher | Google Scholor - M Yuksel, G Demirpolat, A Sever, S Bakaris, E Bulbuloglu, N. Elmas. (2007). Hydatid disease involving some rare locations in the body: a pictorial essay. Korean J Radiol, 8(6):531-540.
Publisher | Google Scholor - L Zubiaurre Lizarralde, I Oyarzabal Pérez, I Ruiz Montesinos, E Guisasola Gorrotxategi. (2006). Invasion of the portal vein by a hydatid cyst. Review of the literature, Gastroenterol Hepatol, 29 (7):405-408.
Publisher | Google Scholor - EP Gonzalez, L Gil-Grande, LR del Arbol, D del Pozo, J Miquel, M Vazquez, et al. (2002). Presinusoidal portal hypertension secondary to portal invasive echinococcosis. J Clin Gastroenterol, 34(1):103-104.
Publisher | Google Scholor - S Sachar, S Goyal, S Goyal, S. Sangwan. (2014). Uncommon locations and presentations of hydatid cyst. Ann Med Health Sci Res, 4 (3):447-452.
Publisher | Google Scholor - Yagmur, S. Akbulut. (2012). Unusual location of hydatid cysts: a case report and literature review. Int Surg, 97 (1):23-26.
Publisher | Google Scholor