Case Report
Rare Chronic Afferent Loop Syndrome Causing Partial Small Bowel Obstruction After Bill Roth II Gastro Jejunostomy: A Case Report
1Surgery Department, College of Medicine and Health Sciences, Hawassa University, Awasa, Ethiopia.
2Life Care Hospital, Kenya.
*Corresponding Author: Tigabu Daniel, Surgery Department, College of Medicine and Health Sciences, Hawassa University, Awasa, Ethiopia.
Citation: Daniel T., Woldegiorgis T. (2024). Rare Chronic Afferent Loop Syndrome Causing Partial Small Bowel Obstruction After Bill Roth ii Gastro Jejunostomy: A Case Report, Journal of BioMed Research and Reports, BioRes Scientia Publishers. 5(4):1-11. DOI: 10.59657/2837-4681.brs.24.112
Copyright: © 2024 Tigabu Daniel, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: September 13, 2024 | Accepted: October 05, 2024 | Published: October 15, 2024
Abstract
Introduction: Chronic afferent loop syndrome is one of rare complication after Bill Roth II gastrojejunostomy. Surgical correction is must to avoid complications that come after conservative management. Most common complications of chronic afferent loop syndrome are sepsis, pancreatitis, cholangitis and ischemia of the afferent loop.
Case Presentation: Here we are presenting 18 years old female patient presented with repeated episodes of bilious vomiting, nausea, epigastric discomfort and distension after her 90th post-truncal vagotomy and Bill Roth II gastrojejunostomy for gastric outlet obstruction secondary to peptic ulcer disease stricture. Braun’s corrective anastomosis done and the patient discharged with improvement. Now the patient was on follow up with no compliant.
Conclusion: Although rare to happen after Bill Roth II gastrojejunostomy reconstruction, it is better to consider chronic afferent loop syndrome irrespective of surgery done time for those who have bilious vomiting. Revision of the bypass surgery is must for chronic afferent loop syndrome to avoid serious complications.
Keywords: gastrojejunostomy; afferent loop syndrome; gastric out let obstruction
Introduction
Afferent loop syndrome is rare mechanical obstruction that occurs after Bill Roth II stomach or esophagus to jejunum anastomosis for malignant or non-malignant diseases [1]. It can be acute or chronic based on its duration of occurrence after the Bill Roth II reconstruction. Acute one will present with in early post-operative complete obstruction but chronic afferent loop syndrome can present with partially obstructed small bowel features for weeks, months and even years [2]. The causative agents are classified as intraluminal, intramural and extrinsic. Acute afferent loop syndrome classically presents with epigastric pain, abdominal distension, nausea, and projectile billows vomiting in early post-operative periods with complete obstruction features that need urgent exploration. In chronic afferent loop syndrome, the patient will have prolonged partial small intestine obstruction features. On long run, the obstruction will cause pancreatitis, cholangitis and overgrowth of microbes in afferent limb of the jejunum leading to sepsis [2-5]. To avoid such complication to happen, there should be surgical correction. Once happen, chronic afferent loop syndrome is managed only surgically [5-7]. Barium meal will show us the filling defect and give clue for obstruction but the best diagnostic modality is contrasting enhanced computed tomography (CT) [8]. The corrective surgical treatment options for Bill Roth II gastrojejunostomy maybe Roux-en-Y or Braun’s anastomosis but endoscopic by pass may be choice in debilitated end stage malignancy patients [9,10]. Here we are presenting rare chronic afferent loop syndrome case after Bill Roth II gastrojejunostomy and truncal vagotomy for patient presenting with gastric outlet obstruction secondary to peptic ulcer disease (PUD).
Case Presentation
18 years old female patient come to our hospital with compliant of bilious vomiting, nausea, abdominal distension and epigastric discomfort after her 90th post-operative day for whom truncal vagotomy and Bill Roth II gastrojejunostomy done for gastric out let obstruction (GOO) secondary to peptic ulcer stricture. For that compliant the patient was inserted nasogastric tube for decompression, resuscitated and managed conservatively by considering post-operative adhesion causing partial small bowel obstruction because she was passing. She was stayed in surgical ward for 72hours, improved and discharged. After five days of discharge, she came with the same compliant, admitted, management started, and thorough work up started. For the past 90 days she was doing well, taking meal comfortably, and gained 20kg weight but no compliant reported on her post-operative follow up. She was passing both flatus and feces but no jaundice, itching sensation or fever. On her general appearance she was better from previous condition but still wasted. Her pulse rate ranges 70-88beat per minute and also the other vital signs were in normal range. She has pink conjunctiva and no reportable findings on HEENT. No abnormality detected on respiratory and cardiac examination. Abdomen was scaphoid and there was healing supraumbilical mid vertical surgical wound otherwise no reportable finding. Normal other system examination except there was some palmar pallor. On complete blood count all parameters were in normal range. Serum electrolytes were also in normal range. Serum amylase and lipase were in normal range and also, liver function test was in normal range. Serum albumin was 3.1mg/dl which is normal. On ultrasound examination there was dilated afferent limb and stomach but collapsed distal bowel otherwise normal biliary ducts, gall bladder and pancreas. On contrast enhanced abdominopelvic computed tomography (CT) there was dilated afferent limb of jejunum, duodenum and stomach with collapsed distal bowel otherwise normal finding (Figure 1).
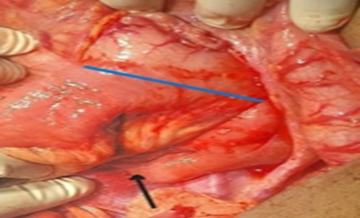
Figure 1: Showing Dilated Afferent Loop (Blue Arrow).
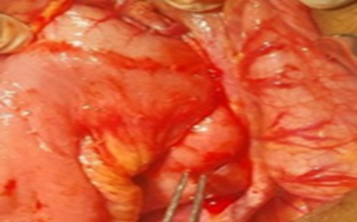
We requested for upper gastro intestinal endoscopy but the patient was not affording and left. By considering chronic afferent loop syndrome, naso gastric tube inserted and there was significant bilious output decompressed. The patient was resuscitated, informed consent taken and taken to operation room (OR). Supraumbilical mid vertical abdominal incision over previous scar was done. The intraoperative findings were-there was adhesion that is partially obstructing the afferent loop, dilated afferent loop, dilated duodenum and stomach, and collapsed efferent limb of jejunum and distal small bowel otherwise normal finding (Figure 2 & Figure 3).
Figure 2: Showing adhesion causing partial obstruction of afferent loop (black arrow) and intact gastrojejunostomy site with adequate patency (blue line).
Figure 3: Dilated Afferent Loop (Tip of the Forceps).
Patent gastrojejunostomy site with adequate size to allow passage of contents. For that Braun’s anastomosis was done, adhesion released and the abdomen closed in layers after the instrument count was correct. The patient was safely extubated with no incident and transferred to surgical ward with smooth post anesthesia condition. In the ward she was followed for seven days and discharged with improvement. She is on her 16th relaparotomy post-operative condition, gaining weight, ambulating, and no discomfort and vomiting.
Discussion
In chronic afferent loop syndrome, the patient will have prolonged partial small intestine obstruction features. In chronic afferent loop syndrome on long run, the obstruction will cause pancreatitis, cholangitis and overgrowth of microbes in afferent limb of the jejunum leading to sepsis [2-5]. Although patients with chronic afferent loop syndrome will have cholangitis, it is better to rule put other causes like stricture on hepaticojejunal anastomotic site. Like patient reported by Meghan R. Mansour et.al showed isolated cholangitis but not pancreatitis that is not clear whether the afferent loop syndrome or hepaticojejunal anastomotic site stricture caused cholangitis. The other issue regarding this case management is, it was managed conservatively which is against standard surgical correction of the afferent loop syndrome [1]. Unlike this case, our patient did not have cholangitis. Like report by Fernando Azevedo et.al, there was adhesion obstructing the afferent limb of the jejunum but there was no clear mention on the Y limb redundancy of the Roux-en-Y [2]. Another difference here is, in our case the initial surgery was Bill Roth II gastrojejunostomy with intact distal stomach and truncal vagotomy with only ten cm afferent loop length that goes with the standard. Another report by Brenton G. Davis et.al, showed stomach cancer advancing growth that causing obstruction which can be expected against our benign case [3]. K.D. Ballas et.al report is showing, acute presentation of afferent loop syndrome unlike ours that is chronic with prolonged duration and partial obstruction. Here also contrast enhanced CT of abdomen is choice of investigation [4]. Unlike our case, report by WARUN JOSE et.al was congenital cause [5]. Most common cause of the afferent loop syndrome was reported that it is progression of the initial malignancy condition unlike our case and common initial procedure done was distal gastrectomy with Bill Roth II gastrojejunostomy reconstruction that may make the afferent limb redundant but our initial procedure was Bill Roth II gastrojejunostomy with intact distal stomach and no redundant afferent limb of the jejunum [5,6,9]. Although rare to happen after intact distal gastrojejunostomy and non-redundant afferent loop of the jejunum still it is better to consider and reconstruct the Gastrojejunostomy once the patient had typical chronic type afferent loop syndrome clinical features.
Conclusion
Although rare to happen after Bill Roth II gastrojejunostomy reconstruction, it is better to consider chronic afferent loop syndrome irrespective of surgery done time for those who have bilious vomiting. Revision of the bypass surgery is must for chronic afferent loop syndrome to avoid serious complications.
Declarations
Ethical Approval and Consent for Participation
Written informed consent for participation was obtained from the patient herself and according to the Hawassa University IRB guideline, an IRB approval letter is not needed for publication of case reports.
Consent for Publication
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Availability of Supporting Data
The data in this case report will be accessed through the Corresponding author.
Competing Interests
The authors report no conflicts of interest in this work.
Funding
There is no financial support.
Authors’ Contributions
Both authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Acknowledgments
My deepest gratitude goes to the patient and family.
References
- Mansour MR, Meram TD, Kessler SA, Khreisat A, Wernette A, et al. (2023). A Rare Afferent Loop Syndrome Case in Adulthood Following Liver Transplantation in Neonatal Hemochromatosis. Gastro Hep Adv. 3(2):212-213.
Publisher | Google Scholor - Azevedo F, Canhoto C, Tralhão JG, Carvalho H. (2020). Management of Afferent Loop Syndrome After Roux-en-Y Subtotal Gastrectomy and Choledocholithiasis with Recurrent Cholangitis. BMJ Case Rep. 13(1):e232498.
Publisher | Google Scholor - Davis BG, Bayudan AM, Kouanda AM. (2023). Afferent Loop Syndrome as Second Presentation of Gastric Outlet Obstruction in Patient with Billroth II Anatomy. ACG Case Rep J. 10(5):e01043.
Publisher | Google Scholor - Ballas KD, Rafailidis SE, Konstantinidis HD, Pavlidis TE, Marakis GN, et al. (2009). Acute Afferent Loop Syndrome: A True Emergency. A Case Reports. Acta Chir Belg. 109(1):101-103.
Publisher | Google Scholor - Jose W, Saxena D, Hoisala R. (2016). Afferent Loop Syndrome in A Patient Having Incomplete Annular Pancreas. BJR Case Rep. 3(1):20160015.
Publisher | Google Scholor - Aoyama S, Motoori M, Miyazaki Y, Sugimoto T, Nishizawa Y, et al. (2021). Successful Treatment of Remnant Gastric Cancer with Afferent Loop Syndrome Managed by Percutaneous Transhepatic Cholangial Drainage Followed by Elective Gastrectomy: A Case Report. Surg Case Rep. 7(1):219.
Publisher | Google Scholor - Barajas-Fregoso, Elpidio Manuel; Romero-Hernández, Teodoro; Macías-Amezcua, Michel Dassaejv. (2013). Pancreatitis Aguda y Síndrome de Asa Aferente. Reporte de Caso, Cirugía y Cirujanos, 81(5):441-444.
Publisher | Google Scholor - Syndrome N obstructive AL, Afferent R Engastric B, Ii B. Brief Reports. (4):318-321.
Publisher | Google Scholor - Alves AR, Almeida N, Ferreira M, Tomé L. (2017). Endoscopic Management of Afferent Loop Syndrome Caused by Enteroliths and Anastomotic Stricture. A Case Reports. Rev Esp Enferm Dig. 109(6):457.
Publisher | Google Scholor - Katagiri H, Tahara K, Yoshikawa K, Lefor AK, Kubota T, et al. (2016). Afferent Loop Syndrome after Roux-en-Y Total Gastrectomy Caused by Volvulus of the Roux-Limb. Case Rep Surg. 4930354.
Publisher | Google Scholor