Research Article
Quality of Life of Patients with Stiff Person Syndrome
1Graduate School of Health and Welfare Sciences, Doctoral program, International University of Health and Welfare, Narita, Japan.
2Department of Physical Therapy, Graduate School of Health and Welfare Sciences, Doctoral program, International University of Health and Welfare, Narita, Japan.
*Corresponding Author: Chiemi Kobayashi, Graduate School of Health and Welfare Sciences, International University of Health and Welfare, Narita, Japan.
Citation: Kobayashi C., Makihara Y., Nishida Y. (2023). Quality of Life of Patients with Stiff Person Syndrome. Clinical Case Reports and Studies, BRS Publishers. 2(6); DOI: 10.59657/2837-2565.brs.23.048
Copyright: © 2023 Chiemi Kobayashi, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: June 21, 2023 | Accepted: July 10, 2023 | Published: July 18, 2023
Abstract
Aim: This study aimed to identify the factors that significantly affect the quality of life (QoL) of patients with Stiff-Person syndrome (SPS) by examining their physical, psychological, and social aspects using questionnaires.
Methods: This cross-sectional study included 23 patients with SPS. Data were collected using several questionnaires. Patient QoL was quantified using the EuroQoL-5-Dimention 5-Level; sociodemographic characteristics and other relevant variables were examined.
Results: QoL was poorer for patients with SPS than those with moderate to severe Alzheimer’s disease. Several important factors for patients’ QoL have been identified, including difficulty in breathing, pain, mobility issues leading to difficulty performing daily activities, depressive symptoms inherent to SPS, and insufficient social support.
Conclusion: Factors that significantly influenced the QoL of patients with SPS were related to multiple aspects of their lives. We evaluated all previously used methods. A disease-specific evaluation form is required to assess these patients thoroughly.
Keywords: EQ-5D-5L; health-related quality of life; sense of coherence; stiff -person syndrome; pain
Introduction
Stiff-Person syndrome (SPS) is an extremely rare disease characterized by systemic painful cramps and muscle stiffness triggered by various external stimuli, including sudden noise, light tactile stimuli, spontaneous movements, emotional changes, and cold environments. As various autoantibodies have been detected in patients with SPS, SPS has been reported to be an autoimmune neurological disease [1,2].
Paroxysmal reactions in the autonomic nervous system, such as temporary overheating, abnormal sweating, tachypnoea, and rapid blood pressure fluctuations, have also been observed. Sudden deaths due to autonomic neuropathy have been reported; therefore, caution is required [1]. The incidence of SPS is approximately 1 to 2 in 1 million people [2]. In Japan, it is subject to the intractable disease research project of the Ministry of Health, Labour and Welfare, and diagnostic criteria have been determined [3]. However, since SPS is relatively rare, it has rarely been investigated thoroughly, and the current challenges faced by patients are unclear. Research projects on designated intractable diseases await the results of epidemiological investigations. Patients with any intractable disease should not only be evaluated based on medical and physical aspects but also on psychological and social aspects. Thus, the QoL of the patients should be considered.
Disease-specific evaluation has been established for patients with several intractable diseases, such as amyotrophic lateral sclerosis and Parkinson's disease. Evaluating these diseases includes a QoL evaluation and an evaluation of physical symptoms, meaning that the patient can be assessed from various aspects, leading to the development of an effective intervention method. However, there is still no disease-specific evaluation of patients with SPS, particularly for those who undergo QoL evaluation. The lack of information on the QoL of patients with SPS is a critical issue, as it prohibits the establishment of treatment protocols for these patients. To our knowledge, this is the first report in Japan to quantify and extract the determinants of QoL in patients with SPS using questionnaires on the physical, psychological, and social aspects of their lives.
Materials and Methods
Patients
Twenty-three patients with a confirmed diagnosis of SPS were recruited. Written informed consent was obtained from all participants before the study began. Questionnaires were mailed to each patient to assess their QoL. They were asked to complete a questionnaire and return it to the research team within two weeks. This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the International University of Health and Welfare Ethical Review Board (10 Feb 2021/No. 20-Io-149).
Measurements
QoL
The EuroQoL-5 Dimensions (EQ-5D) is a five-item questionnaire that assesses mobility, self-care, usual activities, pain or discomfort, anxiety, and depression. It was originally developed with three levels of evaluation for each item (EQ-5D-3L) and has been used in many countries. However, since several studies reported that the sensitivity of the EQ-5D-3L was insufficient and that the ceiling effect was considered a problem, the EuroQoL-5 Dimensions 5 level (EQ-5D-5L) index was developed. The questionnaire consisted of five subjective assessment levels for each item, with 1 point indicating no problems; 2 points, slight problems; 3 points, moderate problems; 4 points, serious problems; and 5 points, extreme problems [4]. In this study, we used the Japanese version [4] of the EQ-5D-5L index to quantify the QOL. The final index was calculated based on a conversion table for the Japanese population. Ikeda et al. analyzed patients' responses to questions about the parameters of "mobility, self-care, normal activity, pain/discomfort, and anxiety/depression" using the compositive time trade-off (cTTO) task from data from the general public and scored them from "11111" to "55555.” The correlation between the actual value measured by cTTO and the estimate by the model for the health condition of the 86 patients was also obtained with r = 0.9 (R2 =0.98). Ikeda et al. have stated that clarifying the relationship between disease-specific QoL measurements in various diseases and pathologies is also a challenge [4].
Related Variables
Dyspnea
Patients were asked if they had experienced difficulty breathing at rest and/or during exertion within the past 2 weeks. If the answer was yes, the patient was asked about the extent of Dyspnea using a numerical rating scale (NRS) ranging from 0 (no Dyspnea) to 10 (severe Dyspnea).
Social support
Social support was classified into two categories: informal support, which was provided by nearby people, including family members and friends, and formal or public support, which was usually provided in accordance with laws such as the Comprehensive Support Law for Persons with Disabilities in Japan. In the present study, the amount of informal social support received by each patient was quantified using the Japanese version of the Duke-UNC Functional Social Support Questionnaire -14 (DUFSS) [5]. To investigate formal support, we asked if each patient had utilized services from a community-based integrated care system and whether the patient possessed a disability certificate or had received a disability pension.
Pain
Participants were asked about their general physical pain in three different categories: current pain, the strongest pain in the past 4 weeks, and average pain over the past 4 weeks. The extent of pain was quantified using the NRS.
Sense of coherence
Sense of coherence (SOC) reflects a coping ability with stress and health maintenance, mostly formed at age 20 and increases gradually with age.6 SOC has both direct and palliative effects on mental health [7]. In this study, SOC was evaluated using the Japanese version of SOC-13 [6].
Self-rating Barthel Index (SB)
As a functional measure, the University of Occupational and Environmental Health version of the Barthel Index Self-Rating Scale 3.3, the reliability of which has been established, [8] was used in the present study. It has a score of 0–100 at three levels: independence, partial assistance, and total assistance, and it evaluates 13 items, namely, eating, grooming, washing or bathing, dressing the upper body, dressing the lower body, toileting, controlling urination, controlling bowel movements, getting in and out of a chair or bed, getting on and off the toilet, getting in and out of a bathtub or shower, walking 50 m on the level, and walking up/down a flight of stairs.
Sociodemographic Features
Regarding sociodemographic data, information on patient characteristics, including sex, current age, age at onset, duration of disease, and the duration from the first hospital visit until SPS diagnosis, was collected.
Statistical analysis
Responses to the EQ-5D-5L index questions on Dyspnea, possession of a disability certificate, disability pension, and use of services of the community integrated care system were compared. Spearman’s correlation coefficients were calculated for questions that quantified the extent of parameters. All statistical analyses were performed using SPSS Statistics software (version 23.0; IBM, Tokyo, Japan). The EQ-5D-5L indices of each disease were compared using the Tukey–Kramer method. Statistical significance was set at p less than 0.05. For multiple comparisons, the significance levels were determined using the Bonferroni correction.
Results
Twenty-one of the 23 patients completed and returned the questionnaires between 7 and 8 August 2021, with a response rate of 91%. Since three patients did not show any supportive findings for the diagnostic criteria, statistical analysis was performed using the data from the remaining 18 cases.
Sociodemographic characteristics
All patients in this study were in the chronic stage (24–252 months after the onset of SPS). The duration required to obtain a definitive diagnosis of SPS is long (1–81 months after the first hospital visit). However, the confidence interval was 15–41 months, indicating that it took at least 1 year to be diagnosed in most cases (Table 1).
Table 1: Sociodemographic characteristics (n = 18, 4 men and 14 women).
| mean ± SD | min | max | 95% CI | |
| Current age (years) | 47.11 ± 13.02 | 23 | 70 | 40.64–53.5 |
| Age at onset (years) | 37.39 ± 11.6 | 16 | 60 | 31.62–43.16 |
| Disease duration (months) | 118.83 ± 52.68 | 24 | 252 | 92.64–145.03 |
| (years) | 9.9 ± 4.39 | 2 | 21 | 7.72–12.09 |
| Duration until diagnosed | 28 ± 26.8 | 1 | 81 | 14.67–41.33 |
| as SPS (months) (years) | 2.33 ± 2.23 | 0 | 6.75 | 1.22–3.44 |
n, sample size; SD, standard deviation; 95% CI, 95% confidence interval
EQ-5D-5L
The mean EQ-5D-5L index scores for the 18 patients with SPS was 0.484 ± 0.186. The EQ-5D-5L index was significantly higher in patients without difficulty breathing than in those with Dyspnea (Table 2A). Patients who received disability pensions had a lower EQ-5D-5L index than those who did not (Table 2A). We examined the correlation between the extent of Dyspnea and pain using the EQ-5D-5L index (Table 2B). The extent of Dyspnea at rest and on exertion showed a significant negative correlation with the EQ-5D-5L index, whereas the extent of pain did not. DUFSS and SOC scores were not significantly correlated with the EQ-5D-5L index. The SB showed a strong positive correlation with the EQ-5D-5L index (Table 2B).
Table 2: Comparison (A) and correlation (B) related to the EQ-5D-5L index for each question
| A | Mean ± SD | Yes | No |
| Do you have difficulty breathing ? | 0.36 ± 0.13; n = 9 | 0.61 ± 0.14**; n = 9 | |
| Do you have a disability certificate? | 0.45 ± 0.17; n = 16 | 0.77 ± 0.02; n = 2 | |
| you receive disability pension ? | 0.41 ± 0.16; n = 13 | 0.68 ± 0.09**; n = 5 | |
| Do you want to use the services of the community comprehensive care system? | 0.41 ± 0.15; n = 6 | 0.52 ± 0.2; n = 12 | |
| B | Degree of difficulty breathing | At rest | r=-0.68**; p=0.002 |
| During exertion | r=-0.67**; p=0.002 | ||
| degree of pain | Biggest pain in the past 4 weeks - | r=0.56; p=0.02 | |
| Average pain over the past 4 weeks | r=-0.49; p= 0.04 | ||
| SOC | r= 0.08 | ||
| DUFSS | r=0.27 | ||
| SB | r=0.83**; p=0.000 |
Table 2: Description.
A. The EQ-5D-5L Index was compared between participants who answered “Yes” and “No” to the questions listed. * p less than 0.05; **: p less than 0.01 by independent samples t-test.
B: Two-variate Spearman correlation coefficients of the EQ-5D-5L Index with listed items. * p less than 0.05, **: p less than 0.01 (Bonferroni corrected).
SD, standard deviation; 95% CI, 95% confidence interval; SOC, sense of coherence; DUFSS, Duke-UNC Social Functional Social Support Questionnaire-14; and SB, University of Occupational and Environmental Health version of the Barthel Index Self-Rating Scale 3.3.
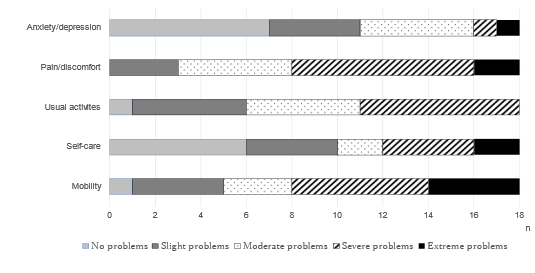
Figure 1 shows the distribution of levels in the five dimensions of the EQ-5D-5L index. Of the five levels of the EQ-5D-5L index, scored at level 2 or higher (i.e., slight problems), which was defined as “problematic.” Pain/discomfort was a problem in all patients; however, seven patients reported no problems, and 11 patients reported having anxiety/depression.
Figure 1: Distribution of levels in each dimension of the EQ-5D-5L.
The number of patients who reported the level (severity) of each subfactor was determined using different patterns. n, sample size
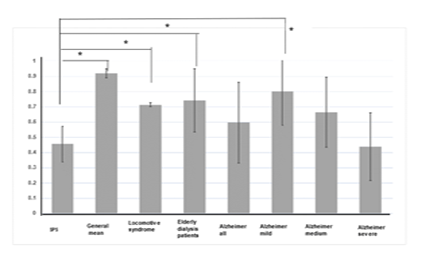
When comparing usual activities and motility, all but one patient was considered “problematic”; however, the extent of the problem differed between patients; four patients answered that they had “extreme problems” in mobility, yet no patients indicated this in usual activities. Regarding self-care, six patients reported no problems. In previous studies, the EQ-5D-5L index has been used in the general population [9] and in populations (Locomo syndrome [10], elderly patients undergoing dialysis, [11] and patients with Alzheimer’s disease12 to quantify QoL. The EQ-5D-5L index of patients with SPS in this study was 0.484±0.186, indicating a low QoL that is comparable to that of patients with moderate-to-severe Alzheimer's disease [12] (see Figure 2).
Figure 2: Comparison of the EQ-5D-5L index between the present study on Stiff-Person syndrome (SPS) and previous studies.
*P less than 0.05, 9General mean, 10locomotive syndrome, 11 elderly patients on dialysis, 12 patients with Alzheimer’s disease.
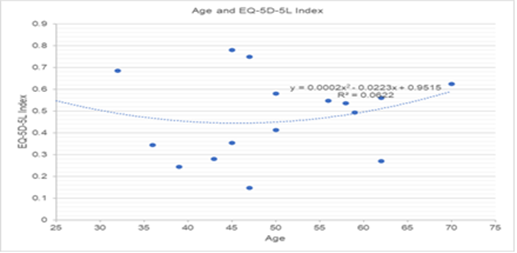
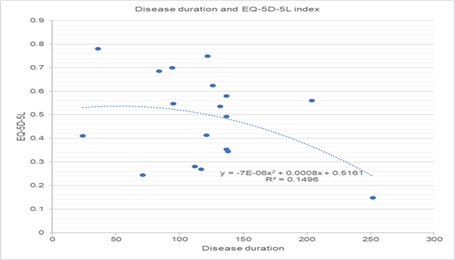
The degree of progression of SPS varied depending on the type of disease; in classical SPS, (n =11) EQ-5D-5L did not correlate with age (Figure 3) or disease duration (Figure 4). Figure 3. Relationship between the EQ-5D-5L index and age, However, no correlations were observed. The Health Visual Analog Scale had many missing values, and in some cases, it was difficult to identify the data. The data obtained were excluded from the analysis because they did not correlate with the EQ-5D-5L index.
Discussion
The present results show that Dyspnea is an important factor affecting the QoL of patients with SPS. Several studies have reported the severity of breathing problems in this population [13] Acute respiratory failure manifesting with apnoeic episodes is a life-threatening and unpredictable complication;[14] thus, Dyspnea significantly influences the QoL of patients with SPS. Furthermore, an association between Dyspnea and decreased mobility and activity in patients with SPS has also been reported.2 Moreover, mobility issues caused by Dyspnea may also be directly related to a significant association between SB scores and the EQ-5D-5L index.
Figure 3: Relationship between the EQ-5D-5L index and age.
However, no correlations were observed.
Figure 4: Relationship between the EQ-5D-5L index and disease duration.
However, no correlations were observed.
All participants considered “pain or discomfort” as problematic. Many previous studies have reported the severity of pain in patients with SPS, which originates from muscle spasm and rigidity [2]. The progression of spasm and rigidity eventually causes difficulties in mobility.2 Thus, pain and mobility issues are mutually related and underlie the deterioration of QoL in patients with SPS. However, pain was not correlated with the EQ-5D-5L index; in contrast, Dyspnea was significantly correlated with the EQ-5D-5L index (Table 2B). The weight of mobility, anxiety, and depression is greater when calculating the EQ-5D-5L score, and that of SPS pain can be underestimated. As some patients require emergency transport and intravenous diazepam infusion [15], the distribution of levels in each dimension of the EQ-5D-5L index should be evaluated, as shown in Figure 2. Eleven patients reported anxiety or depression on the EQ-5D-5L scale. Since patients with SPS are known to have psychological symptoms such as agoraphobia, anxiety induced by external stimuli, and emotional upset as inherent characteristics [2], anxiety or depression in the EQ-5D-5L index reflects this feature. We also measured SOC as a measure of coping ability, which declines with an increase in depressive symptoms [16], SOC scores were not associated with the EQ-5D-5L index; thus, the extent of coping ability and depressive symptoms did not have a strong impact on QoL in patients with SPS. However, the results of the SOC in the present study showed that 10 patients scored less than 59 points, which is considered a cutoff point for a high risk of depression [17], We suggest that the SOC score results also reflect the psychological features of patients with SPS. An association between depression and QoL in patients with SPS has also been previously reported [18].
We investigated the effects of formal social support (disability certificates and pensions) on QoL. Only patients with severe disabilities were authorized to receive social benefits. Our results showed that patients receiving a disability pension had lower EQ-5D-5L index scores than those not receiving it, indicating that the extent of disability had a greater impact on QoL than formal social support. The disability pension is currently just over 700,000 Japanese yen (5,136.48 US dollars as of 9 July 2022) per year. Based on the present results, this amount was insufficient to demonstrate a positive influence on QoL. Furthermore, our results showed that only six of 16 patients with disability certificates were regular users of the community comprehensive care system. Various social services are offered in the system based on the social and physical conditions of each user, which means that users are required to provide personal information and communicate closely with the system staff. We suggest that the inherent psychological features of the SPS, particularly emotional distress and stress induced when patients feel that they are not fully understood, would be a major obstacle to the regular use of this system. This may represent another aspect of the QoL deterioration caused by psychological symptoms. The DUFSS results, as a measure of informal support, showed no correlation with the EQ-5D-5L index. However, the actual score of patients with SPS was 57.5 ± 14.6, which was higher than that of patients with advanced cancer or acquired immunodeficiency syndrome (42.9 ± 13.9) [19].
Conclusion
In conclusion, we suggest that the amount of informal support in patients with SPS is not low and that investigating its association with QoL may require different forms of QoL evaluation. Because SPS progression varies by disease type and there was no correlation between the EQ-5D-5L scores of patients with classical SPS and age and disease duration, the weight of EQ-5D-5L scores may not match that of SPS. It was also unclear whether differences in individual progression were related to treatment. Therefore, it is desirable to develop SPS-specific evaluation methods.
Abbreviations
DUFSS: Duke-UNC Functional Social Support Questionnaire -14
EQ-5D-5L:EuroQoL-5-Dimension 5-level.
QoL: Quality of Life
S.B: Barthel Index Self-Rating Scale 3.3
SOC: sense of coherence
SPS: Stiff-Person syndrome
Declarations
Acknowledgements
We would like to thank the patients who participated in this research. We would like to thank Editage (www.editage.com) for English language editing.
Author contributions
All authors have participated in conception and design, or analysis and interpretation of the data; drafting the article or revising it critically for important intellectual content; and approval of the final version of manuscript.
Competing interests
The use of the Japanese version of the EQ-5D-5L in this study was approved by the Euro QoL group (ID: 39794).
Conflicts of Interest
The research was conducted only by the International University of Health and Welfare research funds (stamps, envelopes, and translation support funds only). The author has no other relevant financial or non-pecuniary interest to disclose from other companies.
References
- Mutou T. (2019). Stiff-person syndrome and progressive encephalomyelitis with rigidity and myoclonus. In: Tuji S, editor. Actual Approach to Neurological Practice. Tokyo Nakayama Syoten.
Publisher | Google Scholor - Scoot DN. (2022). NORD Stiff-person syndrome.
Publisher | Google Scholor - Matsui N, Tanaka K, Kajia R. (2018). Stiff-Person Syndrome and Related Autoantibodies. Brain Nerve, 70(4):357-362.
Publisher | Google Scholor - Ikeda S, Shiroiwa T, Igarashi A. (2015). Developing a Japanese version of the EQ-5D-5L value set. J Natl Inst Public Health, 64:47-55.
Publisher | Google Scholor - Iwase N, Ikeda T. (2008). Development of Japanease Version of Japanease Version of Duke Social Index (DSSI-J). Bull Aich PrefColl Nurs Health, 14:19-27.
Publisher | Google Scholor - Togari T, Yamazaki Y, Nakayama K, Yokoyama Y, Yonekura Y. et al. (2015). Nationally represcntative score of Japanese Langage version of the 13-item 7-point sense of coherence scale. Japan Public Health Magazine. 62:232-237.
Publisher | Google Scholor - Antonovsky A. (1987). Unraveling the Mystery of Health: How People Manege Stress and Stay Well. Tokyo: Yushindo Koubunsha.
Publisher | Google Scholor - Hachisuka. K, Okazaki T, Ogata H. (1997). Self-rating Barthel lndex Compatible with the Original Barthel Index and the Functiomal Independence Measure Motor Score. J UOEH, 19:107-121.
Publisher | Google Scholor - Shiroiwa T, Fukuda T, Ikeda S, et al. (2016). Japanese population norms for preference-based measures: EQ-5D-3L, EQ-5D-5L, and SF-6D. Qual Life Res., 25:707-719.
Publisher | Google Scholor - Tanaka S, Ando K, Kobayashi K, Seki T, et al. (2020). Association between locomotive syndrome and the Japanese version of the EQ-5D-5L in middle-aged and elderly people in Japan. Nagoya J Med Sci., 82:5-14.
Publisher | Google Scholor - Shimizu U, Aoki H, Sakagami M, Akazawa K. (2018). Walking ability, anxiety and depression, significantly decrease EuroQol 5-Dimension 5-Level scores in older hemodialysis patients in Japan. Arch Gerontol Geriatr, 78:96-100.
Publisher | Google Scholor - Ashizawa T, Igarashi A, Sakata Y, et al. (2021). Impact of the Severity of Alzheimer's Disease on the Quality of Life, Activities of Daily Living, and Caregiving Costs for Institutionalized Patients on Anti-Alzheimer Medications in Japan. J Alzheimers Dis., 81:367-374.
Publisher | Google Scholor - Sexauer W, Woodford M, Pack K, Allen A, Crawford A, Rakocevic G. (2019). Dyspnea in Patients with Stiff-Person Syndrome. Am J Med Sci. 358:268-272.
Publisher | Google Scholor - Vincent J, Laurent L, Thierry G, Henry C, Daniel DS. Et al. (2016). Acute Respiratory Failure in a Patient with Stiff-Person Syndrome. Neurocnt Care. 25:455-457.
Publisher | Google Scholor - Crispo JAG, Thibault DP, Fortin Y, Willis AW. (2018). Inpatient care for stiff person syndrome in the United States: a nationwide readmission study. J Clin Mov Disord., 5:1-8.
Publisher | Google Scholor - Takayama T, Asano Y, Yamazaki K, et al. (1999). Sence of coherence stressful life events and psycological health. Japan Public Health Magazine, 46:965-976.
Publisher | Google Scholor - Kobayashi T. (2017). Effects of sense of coherence on depressive synptoms after employment in the Japan Selfe-Defence Force among male young adalts. Japanese Society of Public Health. 64:150-155.
Publisher | Google Scholor - Gerschlager W, Schrag A, Brown P. (2002). Quality of life in stiff-person syndrome. Mov Disord., 17:1064-1067.
Publisher | Google Scholor - Saracino R, Kolva E, Rosenfeld B, Breitbart W. (2015). Measuring social support in patients with advanced medical illnesses: An analysis of the Duke-UNC Functional Social Support Questionnaire. Palliat Support Care, 13:1153-1163.
Publisher | Google Scholor