Research Article
Quality of Life in Patients with Stiff-Person Syndrome: Evaluation Congruent with Patient Values using the Schedule-Direct Weighting Method
1Graduate School of Health and Welfare Sciences, International University of Health and Welfare, Narita, Japan.
2Department of Physical Therapy, School of Health Sciences at Narita, International University of Health and Welfare, Narita, Japan.
*Corresponding Author: Chiemi Kobayashi, Graduate School of Health and Welfare Sciences, International University of Health and Welfare, Narita, Japan.
Citation: Kobayashi C., Makihara Y., Nishida Y. (2023). Quality of Life in Patients with Stiff-Person Syndrome: Evaluation Congruent with Patient Values Using the Schedule-Direct Weighting Method. Journal of BioMed Research and Reports, BRS Publishers. 2(4); DOI: 10.59657/2837-4681.brs.23.029
Copyright: © 2023 Chiemi Kobayashi, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: June 21, 2023 | Accepted: July 06, 2023 | Published: July 13, 2023
Abstract
Patients with chronic progressive disease have a low health-related quality of life (HRQoL); however, various compensation mechanisms can improve and restore quality of life (QoL) even in cases of severe physical disability. In this study, we evaluate QoL according to patient value by individual QoL evaluation and identify QoL determinants in patients with stiff-person syndrome (SPS) to consider appropriate support measures. By 13 December 2020, SPS patients completed semi-structured interviews. For patients, the positive factors were "family support" and "parental care", while the negative factors were "physical symptoms" and "relationship with doctors". Parental care" was identified as the most important area, but satisfaction was low. Therefore, in each case, support is needed to ensure that the patient is satisfactory. In addition, "physical symptoms" are the strongest negative areas and can be alleviated with appropriate medical assistance. In addition, rehabilitation should work on pain relief caused by muscle spasms and stiffness.
Keywords: compensation mechanisms; chronic progressive disease; determinants of quality of life; schedule for the evaluation of individual quality of life-direct weighting; stiff-person syndrome; health-related quality of life
Introduction
Stiff-person syndrome (SPS) is ‘a very rare autoimmune neuropathy characterised by painful muscle spasms and muscle rigidity’ [1, 2]. The disease comes in many forms [1], and due to the low level of awareness regarding the disease, it is commonly misdiagnosed as an orthopaedic disease or a mental illness [1, 3, 4].
Nakane et al. indicate that severe muscular rigidity leads to lumbar lordosis and impairs voluntary movements such as walking, and it is severe enough for a patient to be unable to move their body [1]. As a result, when patients experience convulsions or stiffness attacks, they are unable to move or perform their typical activities of daily living (ADLs). Crispo et al. report SPS inpatient care in the United States with the goal of describing inpatient treatment and characterising 30-day inpatient readings (n=703); ‘other hereditary and degenerative nervous system conditions’ was the most frequently recorded group of primary reasons for index SPS hospitalisation (29.5%), and other leading reasons for index hospitalisation included ‘diabetes complications’ (5.1%), ‘septicaemia’ (3.9%), ‘other nervous system disorders’ (3.7%), ‘spondylosis, intervertebral disc disorders, and other back problems’(2.4%), and ‘respiratory failure, insufficiency, and arrest’ (1.7%) [5]. Sudden death due to autonomic neuropathy has also been reported [5-7]. Previous studies have clinically evaluated patients’ health-related quality of life (HRQoL). For example, Ortiz et al. report on each treatment and show that they were effective in completing ADLs, reducing convulsion frequency, and weakening muscle tone according to the Ashworth Scale, even though evaluation methods differed for each treatment [2]. Marinos et al. assess the degree of stiffness, stiffness distribution, increased sensitivity (twitching and falling), and timed activity, and while there were individual differences/improvement in all categories indicating SPS, the symptoms eventually worsened [8]. Sarva et al. analyse the presence of clinical symptoms after identifying the disease type [9]. Abbatemarco et al. utilise the Numerical Assessment of Pain Scale, Spasm Frequency Scale, Lower Limb Modification Ashworth Scale, and Timed 25-foot Gait Scale to find that the intrathecal baclofen therapy was effective for medically refractory spasticity caused by SPS and helped reduce the dosage of oral medications [10]. Furthermore, the patients’ quality of life (QoL) improved, their gait was maintained, and patients noted a decrease in convulsive frequency [10].
In Japan, SPS diagnostic criteria were developed in 2018 and later improved to encompass disorders with confirmed diagnostic criteria; however, they are still in the epidemiological survey stage. Although SPS is verified as an intractable disease, it is not designated as such in Japan; as a result, it does not receive adequate social support, negatively impacting patients’ mental health, economic position, and physical symptoms. Furthermore, because SPS is not a classified intractable condition, the mechanism to compensate for the decline in QoL has not been thoroughly researched. The HRQoL of people with incurable disorders declines as the disease progresses. Until now, no research has found a link between patient needs and HRQoL [11]. HRQoL assesses medical aspects by focusing on a disease’s functional characteristics and symptoms. However, HRQoL decreases in patients with incurable diseases and those getting end-of-life care, and patients’ requirements and sense of well-being are difficult to identify [2]. As there is no disease-specific evaluation method for classified intractable disorders such as SPS, QoL must be assessed using patient values.
The Schedule for the Evaluation of Individual Quality of Life-Direct Weighting (SEIQoL-DW) is a World Health Organisation-recommended individual QoL assessment tool that directly weighs QoL dimensions in the QoL assessment of intractable diseases and palliative care [12]. We assessed patient QoL based on the results suggesting importance in patients’ lives and investigated the determinants of patient QoL based on the specific domains. In addition, we compared SPS to other diseases, extracted the determinants of QoL, and found the components that require assistance. This is the first SEIQoL-DW assessment of SPS. We hypothesise that if the requisite compensatory mechanism is ineffective, the SEIQoL-DW score will fall.
Methods
This is a cross-sectional observational study, in which participants were recruited through patient groups and Facebook and invited for interviews. The SEIQoL-DW was conducted in person from 28 May to 18 June 2021. This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the International University of Health and Welfare Ethical Review Board (10 Feb 2021/No. 20-Io-149). All individual participants in the study provided written informed consent. The SEIQoL-DW was completed online on the interview record form. It provided the interviewer an overall assessment of response time, understanding, fatigue/reduced motivation, and the adequacy of the data obtained. The SEIQoL-DW included of predetermined questions and explanations, with supplemental explanations offered based on each patient’s level of understanding.
First, the interviewer inquired, ‘What are the five most important areas of your life right now?’ The participants next identified five areas that they believed were currently making their everyday life enjoyable or sad, that is, the areas (cues) that determined their QoL. The patient’s interpretation of each cue is critical; that is, the underlying meanings of their answers were defined by asking them to talk about it. For example, going to Church (cue) is described differently in the grounded theory depending on whether it is for religious reasons or socialising with friends [12]. Second, the five cues were levelled using the Visual Analog Scale. Finally, the importance of each cue was displayed (through a pie chart). By multiplying the levels by the weights, the category weight (CW) was computed, and the SEIQoL-DW index was calculated as the sum of the five CWs. Furthermore, although being regarded as significant by individuals, cues with low CWs were the ones that required support, and those with high CWs were critical in determining QoL. The total index ranged from 0 to 100. The higher the index, the better the QoL of patient attributes (disability certificate, disability pension, and self-assessment Barthel Index [SB] [13], which were compared with the SEIQoL-DW index).
Methods
This is a cross-sectional observational study, in which participants were recruited through patient groups and Facebook and invited for interviews. The SEIQoL-DW was conducted in person from 28 May to 18 June 2021. This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the International University of Health and Welfare Ethical Review Board (10 Feb 2021/No. 20-Io-149). All individual participants in the study provided written informed consent. The SEIQoL-DW was completed online on the interview record form. It provided the interviewer an overall assessment of response time, understanding, fatigue/reduced motivation, and the adequacy of the data obtained. The SEIQoL-DW included of predetermined questions and explanations, with supplemental explanations offered based on each patient’s level of understanding.
First, the interviewer inquired, ‘What are the five most important areas of your life right now?’ The participants next identified five areas that they believed were currently making their everyday life enjoyable or sad, that is, the areas (cues) that determined their QoL. The patient’s interpretation of each cue is critical; that is, the underlying meanings of their answers were defined by asking them to talk about it. For example, going to Church (cue) is described differently in the grounded theory depending on whether it is for religious reasons or socialising with friends [12]. Second, the five cues were levelled using the Visual Analog Scale. Finally, the importance of each cue was displayed (through a pie chart). By multiplying the levels by the weights, the category weight (CW) was computed, and the SEIQoL-DW index was calculated as the sum of the five CWs. Furthermore, although being regarded as significant by individuals, cues with low CWs were the ones that required support, and those with high CWs were critical in determining QoL. The total index ranged from 0 to 100. The higher the index, the better the QoL of patient attributes (disability certificate, disability pension, and self-assessment Barthel Index [SB] [13], which were compared with the SEIQoL-DW index).
Analysis
The mean values of levels, weights, and CWs were calculated using Microsoft Excel from the definitions of critical areas. The associations between diseases were compared using the Tukey–Kramer method. Finally, we analysed all cases and verified the relationship between the SB and SEIQoL-DW.
Results
Fifteen individuals volunteered to participate; however, one could not participate due to family obligations and another could not be reached. Thirteen patients were eligible to take part in the trial, but one was in complete remission and was thus excluded.
Table 1 shows the attributes of patients. All patients had a disability certificate, but only four had access to the community-based integrated care system.
Table 1: Demographic characteristics (N=12) of three male and nine female patients
| Characteristics | Grade | n |
| Disability certificate | 1 | 5 |
| 2 | 4 | |
| 3 | 3 | |
| Disability pension | 1 | 6 |
| 2 | 4 | |
| 3 | 1 | |
| none | 1 |
Efficacy of the SEIQoL-DW testing
The interview lasted 42.25±18.67 minutes on average (range: 20-85 minutes). Eight patients reported good comprehension, four had low/unknown comprehension, and four needed additional explanations. Furthermore, five patients reported no fatigue/decreased motivation, five reported minor fatigue/decreased motivation, and two indicated extremely significant fatigue/decreased motivation. None of the patients withdrew.
The interview time was relatively long because the examiner had breathing problems and had to read the explanations while experiencing breathing difficulties. Furthermore, the examiner had to listen carefully because the patients frequently exhibited dysarthria and dyspnoea. One of the five patients with ‘slight fatigue/decreased motivation’ could produce pie charts on their own, one felt fatigued from sitting, one was unwell, one stated the interview was simpler than housekeeping, and one complained about trouble hearing owing to audio problems. One of the two patients who answered ‘very high’ for fatigue and loss of motivation chuckled about his regular fatigue, and the other stated he felt sick not because of the examination, but because of his medical condition. Therefore, given that there was no loss of motivation or dropout, the validity of the evaluation was deemed sufficient.
Validation from the definitions
Table 2 shows the classification of definitions and the contents of the cues. Physical symptoms were indicated as the most common category, followed by ‘family support’, ‘anxiety’, and ‘hobby’. ‘Physical symptoms’ included difficulty in ‘shopping’ and ‘eating’. Patients frequently hesitated to go out because, while they wanted to see and walk more, they were worried that seizures would occur. Therefore, these difficulties were characterised as ‘physical symptoms. Furthermore, it was observed that one could not eat adequately at night without the assistance of helpers due to their ‘physical symptoms’.
Table 2: Classification of definitions and the contents of cue.
| Definition area | Contents of the patient-mentioned cue | n |
| Physical symptoms | Living, I cannot read in my physical condition, body pain and tension, body tenseness, cramping, breathing, being able to walk freely, my health, I cannot do housework anymore, my health, one could not eat properly at night, shopping | 12 |
| Family support | Family (as indicated by two individuals); husband (as indicated by two individuals), husband, children and family, family health, family (wife) | 7 |
| Anxiety | Anxiety about not knowing what kind of illness I have, anxiety about illness, anxiety about the future, hoping to be positive, anxiety about medication, be positive, future facility admissions | 6 |
| Hobby | Hobbies (as indicated by two individuals), boats, piano, enjoying hobbies | 5 |
| Economic issues | Money (as indicated by two individuals), life after retirement, financial problems | 4 |
| Relationship with doctors | Hospital, relationship of trust with hospitals and doctors, relationship of trust with hospitals (doctors), lack of hospitals where you can be examined | 4 |
| Supporter | Care manager, environmental adjustment, living in elderly housing, getting help | 4 |
| Work | Job, working, helping farmers, job | 4 |
| Parental care | Caring for parents, parents, taking care of parents, wanting to spend time with parents | 4 |
| Emotional support | Snuggling, maintaining a lifestyle, Buddhism | 3 |
| Elimination of anxiety | I place anxiety-relieving objects such as photos and gifts from friends around myself, I do things that allow me to immerse myself in them because I get anxious if I am not doing anything. | 2 |
| Outing | I want to go out, go out on my own | 2 |
| Symptomatic stabilisation | Keep the wave of symptoms | 1 |
| Change of pace | Change my mood by going shopping | 1 |
| Hope | Challenge | 1 |
n: number
Regarding the patients’ relationships with their doctor, there were also opinions reflecting both extremes. One patient said they were treated as fraudulent but stated, ‘I think it was the limit for doctors at that time. However, now the doctors say they will do whatever they can; hence, I want to build a trusting relationship with them instead of being repulsed by them’. In contrast, another patient said, even after being diagnosed with SPS, I was forced to go back and forth between the psychiatry and neurology departments. Some doctors do not believe I have SPS because they do not have antibodies; even now, they do not recognise SPS. I was told that I would no longer be examined at my hospital, and I thought of dying by committing suicide. I obtained a second opinion, and I was treated after writing a stern letter declaring that I had SPS and not a mental illness. Opinions have diverged within the department, and I still feel that hospitalisation is difficult. Doctors say that SPS does not cause respiratory function symptoms; however, it can still cause difficulties in breathing. Hence, I feel that doctors do not have a sufficient understanding of SPS.
Determinants of QoL
Table 3 depicts the determinants of QoL with weights. A positive area had a large weight and high level, while a negative area had a large weight and low level.
Table 3: Comparison of definitions, levels, weights, and category weights.
| Definition area | n | Level mean ±SD | Weight % mean±SD | CW mean ±SD | |
| Negative factor | Physical symptoms | 12 | 30.83±29.99 | 25.08±21.01 | 6.76±9.1 |
| Anxiety | 6 | 25±32.71 | 10.5±12.06 | 1.78±1.78 | |
| Hobby | 5 | 43±33.84 | 10.5±5.7 | 4.95±4 | |
| Relationship with doctors | 4 | 63.75±27.54 | 17.75±9.8 | 8.44±6.74 | |
| Supporter | 4 | 30±21.6 | 13±6.78 | 7.28±4.38 | |
| Work | 4 | 13.75±24.28 | 10.75±8.1 | 2.69±4.89 | |
| Positive factor | Family support | 7 | 88.57±14.64 | 34.71±17.09 | 29.74±13.24 |
| Economic issues | 4 | 72.5±27.54 | 14.75±4.11 | 10.6±5.2 | |
| Parental care | 4 | 50±35.59 | 41.25±30.1 | 24.75±23.77 |
n: number, CW: category weight, SD: standard deviation
As with other disabilities, "family support" was the strongest area. Informal support was important and sufficient for the SPS. In addition, "physical symptoms and anxiety" were cited by many patients. Furthermore, ‘physical symptoms’ were the most significant negative area. As previously said, the ‘relationship with doctors’ was extreme due to the substantial level of ‘relationship with doctors’, but the CW was low. Prior to the publication of diagnostic criteria, patients with SPS had problems with awareness and understanding their medical professionals.
‘Supporters (formal)’ had a CW mean of 7.28 because it had a low level and low weight. Although the community-based integrated care system had few users, there was a latent need for such a system. Further, ‘work’ was separated from ‘economic issues’ to include the social role. Patients who wished to work were compelled to work full-time. Those who were unable to work long hours felt that their physical condition was unacceptable. They stated that the work environment was not adequately prepared due to a lack of awareness of people with chronic diseases in the workplace. It also had the lowest level, while the CW average was the second lowest of all areas, at 2.69. ‘Hobby’ seemed to be a buffering element for anxiety, with a level of 43 and a CW mean of 4.95. Finally, ‘anxiety’ had the second lowest level, at 25, and the lowest CW, at 1.78.
Comparison of SPS with other diseases
In this study, the mean SEIQoL-DW index for SPS patients was 52.55±24.44 (range: 6.75–90) with a 95% confidence interval of 52.55±15.53. The areas (cues) identified as important for patient QoL were ‘physical symptoms’, ‘family support’, and ‘anxiety’. Table 4 compares SPS in this study to previously reported diseases.
'Family support’ was the most important factor for palliative care outpatients, including 35 patients in the anti-cancer treatment group and 33 patients in the palliative care group, and the SEIQoL-DW index was notably high in the palliative care group [14]. In the anti-cancer treatment group, ‘cancer treatment’ was the second most extracted region, and patients who prioritised cancer treatment had lower SEIQoL-DW values than those who prioritised other areas [14].
Table 4: Comparison of Stiff-Person syndrome with other diseases.
| Disease | n | Mean ± SD (Min-Max) | Cue mentioned | Author |
| SPS | 12 | 52.55±24.44 (6.75-90 | Physical symptoms, family support, anxiety | Current study |
| Anti-cancer treatment group | 35 | 61.5±21.0 | In both cases, the first is family, but in the anti-cancer treatment group, cancer treatment is second. | Sakashita et al. [15] |
| Palliative treatment group | 33 | 74.4±14.9 | ||
| Advanced cancer | 62 | 59.17±8(6-95) | Family, health, social activities, religion, friendship, contentment/happiness | Dympa et al. [14] |
| PD | 15 | 74.6±18.1 | Family, friends, hobbies, health, and economic activities | Takahashi et al. [16] |
| ALS | 80 | 73.3±22.8(1-98) | Social support, depression, religiosity, related to economic status | Chio et al [17] |
SPS: Stiff-Person syndrome, PD: Parkinson’s disease, ALS: amyotrophic lateral sclerosis, n: number.
Another study found that the most extracted areas among 62 patients with advanced cancer were ‘family support’, ‘health’, ‘social activity’, ‘religion’, ‘friendship’, and ‘contentment/well-being’ [15]. Furthermore, the most frequently extracted areas among 15 individuals with Parkinson’s disease (PD) were ‘family support’, ‘friends’, ‘hobby’, ‘health’, and ‘economic status’, which were significantly correlated with ‘communication ‘in the Parkinson’s Disease Questionnaire-39. It is critical to strengthen social networks and foster communication to improve the QoL of PD patients [16]. Another study found that 80 patients with amyotrophic lateral sclerosis had ‘social support’, ‘depression’, ‘religiosity’, and ‘economic status’ [17].
SPS was compared with other diseases using the Tukey–Kramer method. Although the lowest mean index was obtained, a significant difference (p less than 0.05) was found between advanced cancer and PD alone. The SEIQoL-DW indices of these diseases did not differ significantly from the SPS index.
Discussion
QoL determinants in patients with SPS from defined regions
The positive QoL determinants from definitions were ‘parental care’, ‘family support’, and ‘economic issues’, and the negative determinants were ‘physical symptoms’, ‘relationship with doctors’, ‘hobby’, ‘supporter’, ‘anxiety’, and ‘work’. The study indicated ‘family support’ as the strongest area. Furthermore, informal support was found to be important and adequately provided for SPS, as indicated when compared to other diseases. As the level of ‘parental care’ is lower than ‘family support’, the former requires some type of support, for example, one patient expressed a desire to take care of her parents herself. The ethos of familism in Japan (which affirms caring for parents within the home rather than outsourcing this care) [18] and the average age of patients made ‘parental care’, which was not heard of in other diseases, an unavoidable dilemma.
Instead of simply recommending the introduction of a third party, we believe it is necessary to secure individual means of transportation and adjust the living environment so that it is more accessible and user-friendly for patients (e.g., mobility adjustments and arrangements to ease housework at the parents’ home, such as lightweight vacuum cleaners, handrails, trolley attachments, and height-adjustable chairs in the kitchen). If environmental considerations can solve an issue, we should offer assistance in the form of proposals. As a result, healthcare workers must assess all aspects of patient activities, not only their home environment. Finally, the findings indicate that ‘economic difficulties’ are unimportant, and that ‘living with family’ and ‘receiving a disability pension’ have little effect on QoL.
‘Physical symptoms’ was the strongest negative area, of which medical assistance was an important part. In rehabilitation, only case reports are available. Furthermore, there are only a few cases where confounding areas can be ruled out; hence, researchers should consider this area for future studies. ‘Relationship with doctors’ was a high-level area; however, its CW was low because it was associated with negative experiences in some patients. This indicates the necessity of increasing the awareness of SPS. Unless it becomes a designated intractable disease, it cannot be accessed at the Intractable Disease Consultation Center. Hence, a definitive diagnosis is expected to take some time. ‘Anxiety’ had the lowest weight, despite being mentioned by half of the patients. In addition, ‘anxiety’ had the lowest level and CW. Patient statements revealed that anxiety develops with the progression of symptoms. Although ‘anxiety’ had a low weight, patients require psychological support during symptom progression.
A ‘job’ is a small pension for young patients with SPS. The financial burden posed by the child until they become independent is high. Most of the SEIQoL-DW participants are on grade 2 or higher disability pension. However, those with a grade 3 pension may find it tough to survive without earning some income. Such individuals have fluctuating physical conditions that are easily exacerbated by external and emotional stimuli. Voluntary movements induce muscle rigidity and muscle spasms, making it difficult for grade 3 pensioners to continue with their occupations. Many patients expressed wanting self-actualisation, and most of them were working. However, gaining what was lost in a new form is a major hurdle under the current system. Although some IT business sites give individuals with SPS preferential treatment, these individuals may find it challenging to retain physical strength throughout office hours. Furthermore, even if integration into the workplace or environment is possible, it is difficult to recognise that such workers require preferential treatment unless there is a vocational training facility nearby to obtain the necessary qualifications (commuting is required under the national system in principle). Although correspondence courses have previously been adopted in some prefectures, due to the limited number of courses available and their short duration, they have not assisted professional growth much. Practical professional advancement necessitates an ever-increasing level of assistance. Moreover, patients with intractable diseases must cope with changes in their illness, which act as a barrier to career advancement.
Comparison of SPS with other diseases
Although patients with SPS had lower SEIQoL-DW indices in this study (52.55±24.44 [range 6.75–90]) than other diseases, the SPS index did not differ significantly from the indices of other diseases such as cancer, PD, and amyotrophic lateral sclerosis (ALS). Interestingly, the ‘anxiety’ section stated in SPS is not found in other diseases. Furthermore, the study discovered that SPS patients seek supporters in the same way as ALS patients do, indicating that there are significant impediments to using formal support. Researchers should define the barriers and investigate why they were not overcome in the future. The main limitation of this study is the small sample size due to SPS being a rare and intractable disease; therefore, the results cannot be generalised. As some patients have raised issues in the past, it is necessary to investigate the problems faced by them before obtaining a disability certificate. New institutional support measures, such as a community-based comprehensive care system for intractable diseases that are not classified as such, are required, and we hope that this study will contribute in this regard.
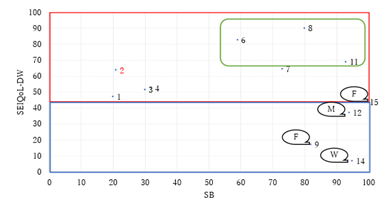
The relationship between the SB and SEIQoL-DW indices was confirmed in areas where psychological adaptation was achieved (more than 45 points) (Figure 1); well-being was observed in patients with more than 60 points, and the high SB group was polarised. The red area represents psychological adaptation; blue area, lack of psychological adaptation; green area, the SB height and SEIQoL-DW values, which are high; and the callouts, the reason the SEIQoL-DW is low despite the SB score being high. Four patients did not reach psychological adjustment, three reached psychological adjustment, and five were happy. Case 2 indicated a state of well-being paradox with all positive cues.
Figure 1: Relationship between SEIQoL-DW and SB.
Note: Speech bubbles are a necessary support and psychological state. S: Formal support. W: Wishing for a full recovery, M: Medical support, SEIQoL-DW, The Schedule for the Evaluation of Individual Quality of Life-Direct Weighting; SB, Self-rating Barthel Index.
Conclusion
This study demonstrated that an important area of SEIQoL-DW for patients was physical symptoms due to pain, such as cramps and stiffness. The results clarified patient needs and examined possible countermeasures. From the rehabilitation perspective, it is necessary to adjust the environment to alleviate patients’ pain, enhance their social activities, and build support that enables young patients who wish to engage in economic activities to receive necessary vocational training. Institutional reform of social support is also required. Remuneration for care for the physically disabled was revised in the fiscal year of 2021; however, few business sites comply with it. As a result, patients with incurable diseases requiring more frequent involvement are not adequately covered by the current care plan regime [19]. Hence, it is necessary to separate intractable diseases from the Welfare Act for Persons with Disabilities. In addition, it is difficult to respond appropriately to intractable diseases that are not fully understood. Therefore, municipalities need to secure not only a small number of business establishments but also a wide variety of business sites regarding quality and quantity and strengthen the information provision of intractable disease consultation centres to enhance the understanding of intractable diseases.
Due to the relationship between SEIQoL-DW and SB, an SEIQoL-DW score of 60 points or more could be used to indicate well-being. Psychological adaptation was defined as a higher positive CW total score than the negative CW total score. Three criteria were used to indicate a failure to accomplish psychological adaptation: a total negative CW total score that is more than the total positive CW total score; a substantial positive CW total score and a significant number of negative cues; and a low level of the most important cue. The third critical factor, the low level of the cue, clearly indicates the need for patients to be more supportive. Although it is crucial to use the SEIQoL-DW to precisely recognise psychological states, the number of samples in this study is small; therefore, more samples are needed to increase accuracy in the future. In addition, longitudinal evaluation should be conducted to confirm changes in support content.
Declarations
Acknowledgements
We express our sincere gratitude to all the patients who participated in the interview. We would like to thank Editage (www.editage.com) for English language editing.
Author contributions
All authors have participated in conception and design, or analysis and interpretation of the data; drafting the article or revising it critically for important intellectual content; and approval of the final version of manuscript.
Conflicts of Interest
The authors have no relevant financial or non-financial interests to disclose.
Consent for publication
The authors affirm that human research participants provided informed consent for the publication of their data in academic papers.
Availability of data and materials
The data generated or analysed during the current study are partially available upon request from the corresponding author. These data may include age and gender and no other personal information, up to 31 March 2024. The research plan, which is in Japanese, is also available.
References
- Nakane, T., Matuo, H. (2013). Stiff-person syndrome in Handbook of neurological disorders (ed. Kusunoki, S.), 298-305.
Publisher | Google Scholor - Ortiz, J. F. et al. (2020). Stiff-person syndrome: A treatment update and new directions. Cureus. 12, e11995.
Publisher | Google Scholor - Caffrey, D., Finn, C. T., Song, S. M., Burton, F. Ⅲ., Arsan, C. (2021). Stiff-person syndrome and psychiatric comorbidities: A systematic review. J. Acad. Consult. Liaison Psychiatry. 162:3-13.
Publisher | Google Scholor - Razmeh, S., Habibi, A. H., Sina, F., Alizadeh, E., Eslami, M. (2017). Stiff person case misdiagnosed as conversion disorder: A case report. Caspian J. Intern. Med. 8:329-331.
Publisher | Google Scholor - Crispo, J. A. G., Thibault, D. P., Fortin, Y., Willis, A. W. Inpatient care for stiff person syndrome in the United States: A nationwide readmission study. J. Mov. Disord. 5:1-8.
Publisher | Google Scholor - Mutou, T. (2019). Stiff-person syndrome and progressive encephalomyelitis with rigidity and myoclonus in Actual approach to neurological practice (ed. Tuji, S.) 2nd edition, 28590 (Routledge, 2019).
Publisher | Google Scholor - Scoot, D. N. (2019). NORD stiff-person syndrome. NORD Rare Disease Database.
Publisher | Google Scholor - Dalakas, M. C. et al. (2001). High-dose intravenous immune globulin for stiff-person syndrome. N. Engl. J. Med., 345:1870-1876.
Publisher | Google Scholor - Sarva, H., Deik, A., Ullah, A., Severt, W. L. (2016). Clinical spectrum of stiff person syndrome: A review of recent reports. Tremor Other Hyperkinet. Mov. 6,1-23.
Publisher | Google Scholor - Abbatemarco, J. R. et al. (2021). Case series: Intrathecal baclofen therapy in stiff-person syndrome. Neuromodulation. 21:655-659.
Publisher | Google Scholor - Kuzma-Kozakiewicz, M. et al. (2019). An observational study on quality of life and preferences to sustain life in locked-in state. Neurology. 93:e938-945.
Publisher | Google Scholor - O’Boyle, C. A., Browne, J., Hickey, A., McGee, H. M., Joyce, C. R. B. (2005). SEIQoL-DW administration manual (1st ed., Japanese version).
Publisher | Google Scholor - Hachisuka, K., Okazaki, T., Ogata, H. (1997). Self-rating Barthel index compatible with the original Barthel index and the Functional Independence Measure motor score. J UOEH. 19:107-121.
Publisher | Google Scholor - Waldron, D., O’Boyle, C. A., Kearmey, M., Moriarty, M., Carney, D. (1999). Quality-of-life measurement in advanced cancer: Assessing the individual. Clin. Oncol. 17:3603-611.
Publisher | Google Scholor - Sakashita, Y., Fujikawa, A., Akizuki, S., Fujisato, M. (2016). Areas considered important by patients undergoing anti-cancer therapy and the subjective QoL: The SEIQoL-DW of outpatients under palliative care. Palliat. Care. 11, 182-188.
Publisher | Google Scholor - Takahashi, K., Kamide, N., Suzuki, M., Fukuda, M. (2016). Quality of life in people with Parkinson’s disease: The relevance of social relationships and communication. J. Phys. Ther. Sci. 28, 541-546.
Publisher | Google Scholor - Chiò, A. et al. (2014). A cross sectional study on determinants of quality of life in ALS. J. Neurol. Neurosur.g Psychiatry. 75:1597-601.
Publisher | Google Scholor - Kato, Y., Tozato, F., Lee, B., Wang, W. C., Shirakura, K. (2009). Factors related to participation of patients with chronic neurological disease in the community: Utilizing the Japanese version of the Craig Handicap Assessment and Reporting Technique (CHART-J). Jpn. Assoc. Occup. Ther. 28:410-419.
Publisher | Google Scholor - (2021). Major revisions in the Ministry of Health, Labour, and Welfare. FY Reiwa 3 revision of remuneration for welfare services for persons with disabilities.
Publisher | Google Scholor