Case Report
Pulmonary Endarterectomy in a Patient with Heparin-Induced Thrombocytopenia using Pre-Cardiopulmonary Bypass Plasmapheresis and Immunoglobulin Infusion
- Pasquale Totaro MD PhD 1*
- Marta Sannito MD 2
- Mara De Amici MD 2,3
- Cesare Giuseppe Perotti MD 4
- Fabio M Pulcinelli MD 5
- Andrea Maria D’armini MD 1,2
1 Cardiac Surgery, Foundation IRCCS Policlinico San Matteo, Pavia, Italy.
2 University School of Medicine, University of Pavia, Pavia, Italy.
3 Laboratory of Immuno-Allergology of Clinical Chemistry and Pediatric Clinic, Foundation IRCCS Policlinico San Matteo, Pavia, Italy.
4 Immunohematology and Transfusion Medicine, Foundation IRCCS Policlinico San Matteo, Pavia, Italy.
5 Department of Experimental Medicine, Sapienza University School of Medicine, Rome, Italy.
*Corresponding Author: Pasquale Totaro, Cardiac Surgery, Foundation IRCCS Policlinico San Matteo, Pavia, Italy.
Citation: P Totaro, M Sannito, Mara D Amici, Cesare G Perotti, Fabio M Pulcinelli, et al. (2022). Pulmonary Endarterectomy in a Patient with Heparin-Induced Thrombocytopenia using Pre-Cardiopulmonary Bypass Plasmapheresis and Immunoglobulin Infusion. Journal of Clinical Surgery and Surgical Research, BRS Publishers. 1(1); DOI: 10.59657/2993-1126.brs.22.002
Copyright: © 2022 Pasquale Totaro, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: November 25, 2022 | Accepted: December 20, 2022 | Published: December 27, 2022
Abstract
We report a peculiar case of a 77 years woman affected by chronic thromboembolic pulmonary hypertension (CTEPH) with surgical indication to pulmonary endarterectomy (PEA) but with the concomitant presence of anti-PF4-heparin autoantibodies. Coagulation disorders are frequently associated in patients with CTEPH and therefore full thrombophilic pattern evaluation is completed as standard preoperative protocol in all our patients. In this case, history of chronic thrombocytopenia induced us to extend preoperative evaluation to the presence of anti-PF4-heparin autoantibodies. Once heparin-induced thrombocytopenia was documented, an alternative approach rather than standard cardiopulmonary bypass with systemic heparinization was mandatory. Due to the characteristics of surgical procedure (i.e., prolonged CPB time, possible risk of intraoperative and postoperative bleeding), we decided to adopt plasmapheresis and immunoglobulin infusion before surgery, thus allowing the standard use of heparin in CPB. The patient underwent a successful PEA without complications. Hemodynamic and clinical results are satisfactory after 3 years of follow-up.
Keywords: cardiopulmonary bypass; heparin-induced thrombocytopenia; pulmonary hyperthension; pulmonary endoarterectomy; plasmapheresis
Introduction
Pulmonary endarterectomy (PEA) is the gold standard for treatment of chronic thromboembolic pulmonary hypertension (CTEPH) [1,2]. Nowadays, however, only few centers worldwide carry extended PEA program with satisfactory short and long-term results. PEA is usually performed using hypothermic cardiopulmonary bypass plus a variable period of circulatory arrest to ensure a bloodless field. We report a peculiar case of a patient with surgical indication for CTEPH complicated by chronic thrombocytopenia and the presence of anti-PF4-heparin autoantibodies. After a multidisciplinary team discussion, we decided for plasmapheresis and immunoglobulin infusion in order to perform the intervention with standard CPB in heparin [3]. Our decision was mainly due to the peculiar aspects of PEA procedure (length of CPB, intraoperative and perioperative bleeding) which were not in favor of alternative anticoagulation protocol for CPB (such as Bivalirudin).
Case report
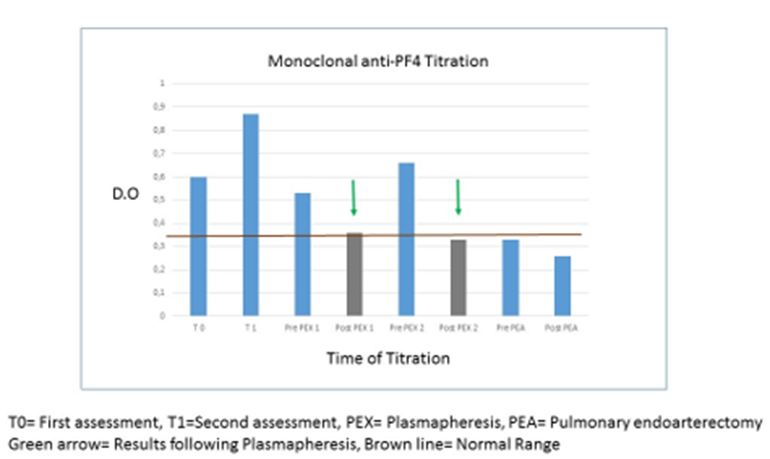
A 77-years-old woman, with medical history of COPD and chronic thrombocytopenia, was admitted in Hospital complaining dyspnea (in WHO class II) and hemoptysis. Following diagnosis of acute pulmonary embolism, she was discharged home with subcutaneous anticoagulation therapy. At 6 months follow-up, however, trans-thoracic echocardiography revealed residual pulmonary artery hypertension (sPAP= 50 mmHg). Subcutaneous therapy was then switched to oral anticoagulant therapy. Two years later, clinical conditions deteriorated with increasing dyspnea (WHO III). Angio CT scan and ventilatory/perfusion (V/Q) scan revealed significant alterations in the pulmonary arteries perfusion. Elevated pulmonary resistances (PVR = 718 dyne*sec*cm-5) was also confirmed at right heart catheterization. Due to the suspicion of CTEPH the patient was referred to our Center. As standardized assessment protocol, to identify potential comorbidities, full thrombophilic pattern was evaluated including, in this case, anti-PF4-heparin antibodies research (both polyclonal and monoclonal as described in appendix 1). Our evaluation confirmed the surgical indication for PEA but antibodies research showed both polyclonal and monoclonal anti-PF4-heparin antibodies. Due to the high risk of heparin-induced thrombocytopenia, PEA was, therefore, delayed. Serotonin release assay (SRA) [4] confirmed functionality of the anti-PF4 antibodies (see appendix 2), and the contraindication for prolonged CPB. Patient continue to deteriorate and a multidisciplinary team, involving surgeons, immunologists, rheumatologists and anesthetists was planned. Plasmapheresis with immunoglobulin infusion before CPB and heparin administration was proposed as an alternative strategy, and patient was admitted to our Center for the scheduled treatment (see appendix). Following written informed consent, she underwent 2 plasmaphereses in 3 days, followed by a human immunoglobulin infusion (0.4 gr/ Kg), obtaining a normalization of Anti- PF4 titer (Figure 1). The day after, once more following specific written informed consent, PEA with standard heparin-based CPB was carried out. Surgical procedure was satisfactory with abundant removal of both fresh and chronic material (Figure 2). In postoperative day 4th patient experienced sudden platelets drop (13.000 plt/mm3) which was treated with corticosteroids. Patients was discharged to rehabilitation clinic in 13rd postoperative day, in stable condition, with a further reduction of Anti- PF4 titer (Figure 1).
Figure 1: The graphic shows the reduction of anti PF4 antibodies following PEX treatment and following PEA
Figure 2: Postoperative picture representing the material removed during PEA. In the right pulmonary artery and its branches (left side), the presence of recent thrombotic material in combination to chronic lesions is notable. Chronic thromboembolic material is, on the other hand, predominant in the left pulmonary artery (right side).
Discussion
PEA is the gold standard for the treatment of CTEPH but is still a surgical procedure limited to few specialized high-volume centers. Accurate preoperative and intraoperative planning is mandatory to achieve satisfactory results currently reported by leading centers (survival >90% at 1 year and >70% at 10 years). Our case was peculiar as we had to face a complex situation. Continuous clinical deterioration indicated a poor prognosis while the risk of heparin induced thrombocytopenia indicated a contraindication for standard CPB protocol. Presence of anti-PF4 heparin autoantibodies represent a well-known contraindication to cardiac surgery. Clinical guidelines recommend to delay non-urgent surgery until anti-heparin antibodies are no more present. In case of urgent surgery and/or persistence of antibodies, alternatives to heparin in CPB have to be evaluated. Bivalirudin, a recombinant direct thrombin inhibitor, has been frequently reported in such respect. It has a short 25 minutes half-life in patients with normal renal function. Monitoring of anticoagulation with Bivalirudin, however, is more challenging [3]. In this case, considering that bleeding is one of the most frequent and potential complication during and after a PEA procedure, other alternatives were examined. Plasmapheresis to remove anti-PF4 antibodies has also been previously reported, in patients with weakly positive ELISA results requiring urgent cardiac procedures, to stabilize platelets count and normalize platelets aggregation, since it can reduce levels of circulating antibodies [5,6]. In this case, despite surgery was not urgent, the prognosis was poor (knowing the survival rate and quality of life of CTEPH patients) and we decided for this option. As far our knowledge this is the first case which report plasmaphereses and immunoglobulin infusion to prevent heparin induced thrombocytopenia during CPB for PEA [7].
Conflict of Interests
The authors have no conflict of interests or financial support related to this manuscript to disclose.
Acknowledgments
We would like to thank the precious support of Maria Luisa Guarino from the Department of Experimental Medicine, Sapienza University of Rome, Angela Rozzi from Cardiac Surgery of Foundation IRCCS Policlinico San Matteo.
References
- Delcroix M, Kerr K, Fedullo P. (2016). Chronic thromboembolic pulmonary hypertension. Epidemiology and risk factors. Ann Am Thorac Soc, 13(S3):201-206.
Publisher | Google Scholor - Shore-Lesserson L, Baker RA, Ferraris V, Greilich PE, Fitzgerald D, Roman P, Hammon J. (2018). STS/SCA/AmSECT Clinical Practice Guidelines: Anticoagulation during Cardiopulmonary Bypass. J Extra Corpor Technol. 50(1):5-18.
Publisher | Google Scholor - Guarino ML, Massimi I, Mardente S, Lappa A, Donfrancesco S, Visentin GP, Pulcinelli FM. (2017). New platelet functional method for identification of pathogenic antibodies in HIT patients. Platelets. 28(7):728-730.
Publisher | Google Scholor - Welsby IJ, Um J, Milano CA, Ortel TL, Arepally G. (2010). Plasmapheresis and heparin reexposure as a management strategy for cardiac surgical patients with heparin-induced thrombocytopenia. Anesth Analg, 110(1):30-35.
Publisher | Google Scholor - Voeller RK, Melby SJ, Grizzell BE, Moazami N. (2010). Novel use of plasmapheresis in a patient with heparin-induced thrombocytopenia requiring urgent insertion of a left ventricular assist device under cardiopulmonary bypass. J Thorac Cardiovasc Surg. 140(3):56-58.
Publisher | Google Scholor - Selleng S., Selleng K. (2016). Heparin-induced thrombocytopenia in cardiac surgery and critically ill patients. Thromb Haemost, 116:843-851.
Publisher | Google Scholor