Case Report
Prone Position Spinal Anaesthesia: Enhancing Comfort and Efficiency
1*DM Cardiac Anesthesia, Department of Anaesthesiology, AIIMS Raipur, India.
2Senior Resident, Department of Anaesthesia, AIIMS Raipur.
3,4Junior Resident, Department of Anaesthesia, AIIMS Raipur.
*Corresponding Author: Gade Sandeep,DM Cardiac Anesthesia, Department of Anaesthesiology, AIIMS Raipur, India.
Citation: S. Gade, V. Swati, N. R. Sathya, C. P. Girish (2024). Prone Position Spinal An aesthesia: Enhancing Comfort and Efficiency, International Journal of Medical Case Reports and Reviews, BioRes Scientia Publishers. 3(5):1-4. DOI: 10.59657/2837-8172.brs.24.060
Copyright: © 2024 Dr Gade Sandeep, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: May 03, 2024 | Accepted: May 18, 2024 | Published: May 29, 2024
Abstract
Prone spinal anaesthesia has emerged as a versatile and effective technique in modern anaesthesia practice, offering unique advantages for various surgical procedures. For many different types of surgery, operative access necessitates the prone positioning of patients under anaesthesia. In certain conditions the patient is unable to lie supine or on the lateral side, or the surgery is to be performed in the prone position. In such cases spinal anaesthesia can be administered in the same position providing patient comfort and avoiding the complications of changing the position of the patient after the administration of spinal anaesthesia. Here we describe 2 cases in which spinal anaesthesia was administered in the prone position which was beneficial to the patient, surgeon and the anaesthesiologist.
Keywords: anaesthesia; spinal; patients; surgery
Introduction
Prone positioning during surgery is used for access to the posterior head, neck and spine during spinal surgery, access to the retroperitoneum and drainage of gluteal abscesses. [1] Patients with abscesses commonly present to the emergency department for incision and drainage. An abscess is an acute painful condition and positioning in such a case is a challenge. Spinal anaesthesia in the prone position has been performed in various orthopaedic, anorectal and lower limb plastic surgeries [2,3]. Here we describe 2 cases in which spinal anaesthesia was administered in the prone position to facilitate patient comfort and surgical ease.
Case 1
A 27-year-old female presented with complaints of pain and swelling in the right gluteal region and was diagnosed with a gluteal abscess. She was planned for incision and drainage of the abscess in the emergency OR (operation room). During the pre-anaesthetic evaluation, the patient was found to be apprehensive, irritable and unable to sit due to the pain. The patient was comfortable in the prone position.
Her vitals at the time of examination were as follows
Pulse rate: 120 beats per minute
Blood pressure: 100/64 mmHg
Respiratory rate: 20 per minute
O2 saturation: 99% on room air
Temperature: 98.4 F, afebrile.
Cardiovascular and Respiratory system examination revealed normal findings.
Preoperative investigations showed
Haemoglobin: 12.5 g/dL.
WBC: 18200 cells/cu mm.
Platelets: 1.58 Lakh.
The patient was cleared for the proposed procedure under the American Society of Anaesthesiologists Physical Status 1(E). In the OR, the patient refused to assume a supine or sitting position due to the pain. A decision was then made to perform a subarachnoid block with the patient in the prone position. The patient and her attendees were explained about the choice of anaesthesia and the position of the patient for this particular technique and consent was obtained. Hence the patient was maintained in a prone position and monitors as per standard ASA criteria were attached. The patient’s back was painted with povidone-iodine solution and draped with a sterile cloth. The operation table was broken at the hips to bring about the Jack Knife position which helped in opening up the lumbar vertebral spaces. Skin infiltration with 1.5 mL of 2% Lignocaine was done to anaesthetise the skin and subcutaneous tissue. Using a 23G Quincke’s needle, a lumbar puncture was performed. A 2 mL syringe was used to confirm the backflow of CSF. Once the backflow of CSF was confirmed, 2.4 mL of 0.5% Bupivacaine Heavy was administered in the subarachnoid space. To prevent the rapid ascent of the drug in the prone position, the head end of the OR table was made flat while the foot end was lowered further. The onset of action of the sensory blockade as assessed using the pinprick method was about 1.2 minutes. The onset of complete motor blockade as assessed by the Modified Bromage scale was about 3 mins 30 seconds. The maximum level of sensory blockade was up to T10. The patient’s hemodynamic were continually monitored throughout the surgery via ECG, pulse oximetry and NIBP. The surgery lasted for 50 minutes, and the course was uneventful. Post procedure the patient’s sensory and motor level was rechecked. The sensory was at level T10 while the Modified Bromage grading was 3. The patient was shifted to the post anaesthesia care unit (PACU) and was observed for 1 hour. The patient maintained stable hemodynamic. The patient was given an Injection of Paracetamol 1g IV for postoperative analgesia and positional pain. The patient was discharged from the PACU after a modified Aldrete score of 9/10 was achieved.
Case 2
A 50-year-old male presented with pain and swelling over the right calf. The patient was a known case of diabetes mellitus, non-compliant with the treatment. The patient was diagnosed with a right calf abscess and was planned for incision and drainage of the abscess on an emergency basis. In the pre-anaesthetic checkup, the patient was assessed thoroughly. His baseline haematological and biochemical investigations were within the normal limits. Random blood sugar values over the last 24 hours were within 140 mg/dL. The patient was wheeled inside the operation theatre and monitors were attached as per the American Society of Anaesthesiologists standards. The choice of anaesthesia was a subarachnoid block with the patient in a prone position to facilitate surgical access and patient comfort. A pillow was placed under the patient’s abdomen to adequately expose the lumbar intervertebral spaces (Figure 1).
Figure 1: Image showing patient positioning for prone spinal anaesthesia
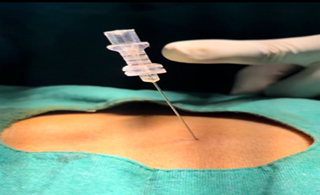
Under all aseptic precautions, a subarachnoid block was performed with a 23G spinal needle. 2.5 mL of 0.5% hyperbaric bupivacaine with 0.5 mL (25 mcg) of fentanyl was administered (Figure 2, 3).
Figure 2: Image showing flow of cerebrospinal fluid (CSF) at the needle hub.
Figure 3: Image showing administration of the spinal drug after confirming backflow.
Post subarachnoid block, the onset and maximum level of the sensory blockade were confirmed using a pinprick test. The level of motor blockade was confirmed using the Modified Bromage scale. The maximum level of sensory blockade was up to T10 level. The patient’s hemodynamic were stable throughout the case. The surgery lasted for 45 minutes. No adverse events such as hypotension or bradycardia were noted. Post-procedure, the patient was shifted to the recovery room and observed for 30 minutes. The patient was shifted to the ward after a modified Aldrete score of 9/10 was achieved.
Discussion
Surgeries done under spinal anaesthesia reduce blood loss and hypoxic events and provide better postoperative analgesia [4]. Spinal anaesthesia in the prone position has been performed in various surgeries [5]. Complications associated with the administration of spinal anaesthesia in the prone position are the rapid ascent of the drug thereby leading to hemodynamic instability and respiratory depression [6]. The unpredictable spread of the hyperbaric spinal drug and the rise of the level of the block was shown in a study by Gudaitytė J et al [7]. In our case, appropriate measures were taken to prevent the rapid ascent of the spinal drug. Immediately after the administration of the spinal drug the head and the table were flattened, and the foot was further lowered. By performing the technique of spinal anaesthesia in the prone position, a further change of position is not required, which would avoid the hemodynamic changes and change in the spread of the drug and level of block. This would provide the already optimal position required by the surgeon for gluteal abscess surgery. In a study conducted by Mohamed Alkhayarin et al [5], in which the patients were administered standard spinal anaesthesia and then turned prone for lower limb orthopaedic procedures, hypotension was a major complication. In our study, no major complication occurred, and the level of the block was monitored meticulously using a pin prick test. Another advantage of spinal anaesthesia in the prone position is the very low incidence of backache and post-dural puncture headache (PDPH). In a case reported by Rajendra et al [8], in which spinal anaesthesia was given in the prone position for a 32-year-old with a large neurofibroma over the left buttock region did not experience any low backache or PDPH. On follow-up, neither of our patients complained of backache or PDPH despite using wide-bore spinal needles (23 Gauge).
Conclusion
In the above case scenarios, spinal anaesthesia administered in the prone position was uneventful and can be used in patients who are unable to sit or lie in a lateral position. Through its ability to enhance surgical access, mitigate airway complications, optimize spinal alignment, and improve patient comfort, prone spinal anaesthesia stands out as a valuable technique in the armamentarium of anaesthesia providers. As research continues to unveil its unique benefits and refine our understanding of its mechanisms and applications, prone spinal anaesthesia remains a promising avenue for improving patient outcomes and advancing the field of anaesthesia practice. Spinal anaesthesia in the prone position for procedures of short duration is feasible and safe.
References
- Kwee, M. M., Ho, Y. H., & Rozen, W. M. (2015). The prone position during surgery and its complications: a systematic review and evidence-based guidelines. International surgery, 100(2):292-303.
Publisher | Google Scholor - Imbelloni LE, Pistarino MA, Miranda Junior MG, Ferreira BTP, Magalhães HL, et al. (2020). Posterior Spinal Anesthesia for Orthopedic, Anorectic and Plastic Surgeries in Prone Position: It Should Be Used More. Int J Anaesth Res, 3(3):126-135.
Publisher | Google Scholor - Baral BK, Poudel PR, Regmi S, et al. (2021). Subarachnoid Block in Prone Position for lower limb surgery. Journal of Nepal Health Research Council, 18(4):801-803.
Publisher | Google Scholor - Attari MA, Mirhosseini SA, Hornarmand A, Safavi MR. (2011). Spinal anaesthesia versus general anaesthesia for elective lumbar spine surgery: a randomised clinical trial. J Res Med Sci, 16:524-529.
Publisher | Google Scholor - Alkhayarin M, Shaikh N, Ghouri SI, Vegesna ARR. (2018). Standard Spinal Anaesthesia Then Turned Prone for Lower Limb Orthopaedic Surgeries. Int J Anesth Pain Med, 4:4.
Publisher | Google Scholor - Missouri S, Ray J, Geara E, Ayoub M, Grieco M. (2023). Administration of Spinal Anesthesia in the Jack-knife Prone Position for Anorectal Surgeries. J Anaesth Surg Res, 3(2):178-183.
Publisher | Google Scholor - Gudaitytė J, Marchertienė I, Pavalkis D. (2004). Anesthesia for Ambulatory Anorectal Surgery. Medicina (Kaunas). 40(2).
Publisher | Google Scholor - Rajendra P, Priti D, Sudha H. (2016). Subarachnoid block in prone position for giant gluteal neurofibroma. J Anesth Crit Care Open Access, 4(2):41-42.
Publisher | Google Scholor