Research Article
Prognostic Significance of Degree of Anaemia and Blood Transfusions in Gastric Cancer Patients
1 University Hospitals of North Midlands, Staffordshire, United Kingdom.
2Dubai Hospital, Dubai Academic Health Corporation, UAE.
*Corresponding Author: Shahid Gilani, University Hospitals of North Midlands, Staffordshire, United Kingdom.
Citation: S Gilani, S H H Tirmazy, Muhammad F Latif, N Ikram, A Jamil. (2023). Prognostic Significance of Degree of Anaemia and Blood Transfusions in Gastric Cancer Patients. International Journal of Clinical and Molecular Oncology, BRS Publishers. 2(1); DOI: 10.59657/2993-0197.brs.23.003
Copyright: © 2023 Shahid Gilani, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: May 03, 2023 | Accepted: May 18, 2023 | Published: May 23, 2023
Abstract
Background: Anaemia is a common complication of many solid tumours and occurs in approximately 41 % of patients with advanced gastric cancer at the time of diagnosis. Studies have shown that anaemia is an independent prognostic factor in gastric cancer, however it is less clear if blood transfusion alters the outcome in these patients. Aim of this study is to evaluate the effect of anaemia and blood transfusion on survival in advanced gastric cancer patients at our institution.
Methods: This is a retrospective review of electronic medical records of gastric cancer patients treated from January to December 2013. Patients' demographics and clinical data was collected and analysed in relation to various factors including level of haemoglobin and use of blood transfusion. Survival was calculated using Univariate, multivariate and Kaplan-Meier survival analysis.
Results: A total of 112 patients were identified including 79 (70%) males and 33 (30%) females with a median age of 73 years. Vast majority (n=88, 79%) of patients had locally advanced (T4 or node positive) disease at initial presentation. Eighty-three patients did not proceed to surgery after neoadjuvant chemotherapy due to inoperable disease. Initial Haemoglobin was >100 gram per litre in 28 (25%) patients. Nineteen patients had Haemoglobin of <80 gram per litre. 96 (86%) patients received blood transfusion. Overall, 98 (87.5%) patients died. The estimated median overall survival was 12 months (95% CI=11-81; SD=17). The 1-, 3-, and 5-years OS were 55%, 30% and 10% respectively. The median progression free survival (PFS) with any treatment was 10 months (SD=20). Univariate analysis showed statistical significance of level of Hb and surgical resection to overall survival (P=0.0122 and P=0.0001). Multivariate analysis showed disease stage, surgical resection and Hb level as independent factors to the outcome.
Conclusion: The point prevalence of anaemia in our gastric cancer patients during treatment had an effect on overall survival. The outcome couldn't be improved with blood transfusion. Our findings indicate the need for a consistent diagnostic and treatment approach to anaemia in this setting.
Keywords: anaemia; blood transfusion; gastric cancer; solid tumour; neoadjuvant chemotherapy; inoperable disease
Introduction
Gastric Cancer is the 5th most common neoplasm worldwide and the 3rd leading cause of death according to the latest Global Cancer Statistics. Over 1 million cases of gastric cancer were diagnosed in 2020 [1]. However, there is wide geographic variation in the incidence of gastric cancer and it is more commonly diagnosed in developed countries. Regions with high incidence include East Asia, Eastern Europe, and Central and South America [2].
The overall 5-year survival rate for gastric cancer is 33%. However, survival varies with the stage of the disease. Up to one third of gastric cancers are diagnosed as stage 4 disease and unfortunately 5-year survival is less than 6% [3]. Several prognostic factors have been implemented in the outcome of both resected and advanced metastatic gastric cancer. The prognostic factors for resected gastric cancer include depth of tumour invasion, lymph node metastasis, location and histologic type. However, in patients with advanced metastatic cancer, prognostic factors include performance status, presence of liver and/or peritoneal metastases, and serum alkaline phosphatase levels [4,5].
Anaemia is a common complication in many solid tumours and occurs frequently in gastric cancer [6]. A systematic quantitative review reported anaemia as an independent prognostic factor for survival in patients with several cancers including lung carcinoma, cervicouterine carcinoma, head and neck carcinoma, prostate carcinoma, lymphoma, and multiple myeloma [7]. It has been hypothesised that tumour hypoxia due to low haemoglobin (Hb) level leads to tumour growth and resistance to therapy as it can lead to angiogenesis, resistance to apoptosis, and a resistance to free radicals from chemotherapy and radiotherapy [8,9]. Several studies have reported anaemia as an independent prognostic factor in patients undergoing surgery for gastric cancer [10,11,12]; however fewer have focused on the prognostic effect of anaemia in patients with advanced metastatic gastric cancer [13,14]. We conducted this study to evaluate the impact of anaemia and blood transfusion on clinical outcomes including progression free survival (PFS) and overall survival (OS) in patients with gastric cancer.
Methods
In this retrospective study, the electronic medical records of patients with gastric cancer from the year January to December 2013 were reviewed. Follow up data was collected till December 2018 (5 years follow up). Patients were identified through the hospital cancer registry. Eligibility criteria included all adult patients with early or advanced stage disease who received systemic therapy with curative or palliative intent during the study period.
Data was collected regarding patients’ demographics, disease stage, histological subtype, HER2 status, intent of treatment, sites of metastatic disease, chemotherapy regimen, local therapy including radiotherapy or surgery, postoperative pathology, initial Haemoglobin level at the time of presentation and use of blood transfusion. Survival was calculated for the overall study population and compared with different variables including age, gender, and histological subtype, stage of disease, chemotherapy regimen, Haemoglobin levels and blood transfusion. Similarly, the effect of various Hb levels on overall survival in metastatic disease was calculated. Univariate and multivariate Cox proportional hazard regression models were used to assess the association between haemoglobin level and overall survival. Overall survival was assessed using Kaplan-Meier survival curves. Statistical analysis was performed by using SPSS version 29.
Results
A total of 112 patients with gastric cancer were identified including 79 (70%) males and 33 (30%) females. Median age of the patients was 73 years. Seventy-one (64%) patients had poorly differentiated adenocarcinoma, 35 (31%) had moderately differentiated adenocarcinoma and 6 (5%) patients had other histological subtypes. Gastric tumour location was proximal (n=59, 53%), middle (n=36, 32%) and distal (n=17, 15%) in the study cohort. Vast majority (n=88, 79%) of patients had locally advanced disease at initial presentation. Subsequently 100 (89%) patients developed recurrent or metastatic disease and 12 (11%) patients remain on surveillance. Forty-one patients had visceral metastases including liver (n=20), lung (n=9) and both (n=12). Sites of non-visceral metastatic disease were lymph nodes (n=68), peritoneum (n=27) and bone (n=3). Most (n=64) patients had single site metastatic disease followed by 2 sites (n=21) and 3 sites (n=14).
Majority (n=105) of the patients received combination chemotherapy either Epirubicin, Oxaliplatin, Capecitabine (EOX) or Epirubicin, Cisplatin, Capecitabine (ECX). Eighty-three patients did not proceed to surgery after neoadjuvant chemotherapy due to inoperable disease. Initial Haemoglobin was >100 gram per litre in 28 (25%) patients and less than 100 gram per litre in 84 (75%) patients. Nineteen patients had Haemoglobin of less than 80 gram per litre. Ninety-six (86%) patients received blood transfusion [Table 1].
Table 1: Patients’ demographics and clinical data
| Demographics/Clinical data | (n) | % |
|---|---|---|
| Male | 79 | 70% |
| Female | 33 | 30% |
| G3 adenocarcinoma | 71 | 64% |
| G2 adenocarcinoma | 35 | 31% |
| Other histologic subtypes | 6 | 5% |
| Proximal gastric cancer | 59 | 53% |
| Middle Gastric cancer | 36 | 32% |
| Distal gastric cancer | 17 | 15% |
| Locally advanced disease | 88 | 79% |
| Metastatic disease | 24 | |
| Visceral metastases | 41 | |
| Liver metastases | 20 | |
| Lung metastases | 9 | |
| Liver & lung metastases | 12 | |
| Non visceral metastases | 98 | |
| Lymph nodes metastases | 68 | |
| Peritoneal metastases | 27 | |
| Bone metastases | 3 | |
| Single site metastases | 64 | |
| 2 sites metastases | 21 | |
| 3 sites metastases | 14 | |
| Hb > 100 g/l | 28 | 25% |
| Hb < 100> | 84 | 75% |
| Hb < 80> | 19 | |
| Blood transfusion | 96 |
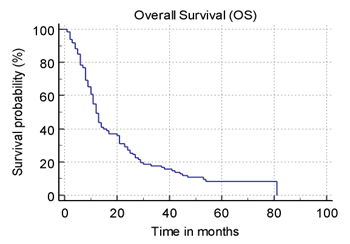
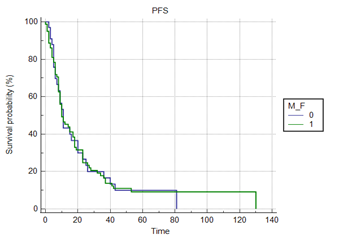
Overall, 98 (87.5%) patients died. The estimated median overall survival was 12 months (95% CI=11-81; SD=17). The 1-, 3-, and 5-years survival were 55%, 30% and 10% respectively. The median progression free survival with any treatment was 10 months (SD=20). [Figure 1, 2] The patients with higher Hb (>100 g/L) had better outcomes as compared to patients with lower Hb (less than 80 g/L).
Figure 1: Median OS= 12 Months; 95% CI=11-81
Figure 2: Progression Free Survival: 10 months
Univariate analysis showed statistical significance of level of Hb and surgical resection to overall survival (P=0.0122 and P=0.0001). Multivariate analysis showed no effect of Blood transfusion, gender, age, chemotherapy regimen and histology on the outcome. Multivariate analysis showed disease stage, surgical resection and Haemoglobin level as independent factors to the outcome [Figure 3].
Figure 3: Regression analysis showed statistical significance of level of Hb and surgical resection to overall survival (P=0.0122 and P=0.0001).
| Independent variables | Coefficient | Std. Error | t | P | rpartial | rsemipartial | VIF |
|---|---|---|---|---|---|---|---|
| (Constant) | 3.4489 | ||||||
| Hb | 5.3898 | 2.1087 | 2.556 | 0.0122 | 0.2537 | 0.2205 | 1.118 |
| Blood Transfusion | 6.3358 | 4.9920 | 1.269 | 0.2075 | 0.1291 | 0.1095 | 1.134 |
| M_F | -1.1031 | 3.4507 | -0.320 | 0.7499 | -0.03278 | 0.02758 | 1.056 |
| age | 0.1252 | 0.1939 | 0.646 | 0.5202 | 0.06608 | 0.05570 | 1.182 |
| Stage | -2.3852 | 2.0008 | -1.192 | 0.2362 | -0.1214 | 0.1029 | 1.183 |
| Operation | 16.2844 | 4.0045 | 4.066 | 0.0001 | 0.3850 | 0.3509 | 1.342 |
| Chemo_Regimen | -4.0473 | 3.6099 | -1.121 | 0.2650 | -0.1143 | 0.09674 | 1.332 |
| Histology | 4.0903 | 3.5513 | 1.152 | 0.2523 | 0.1174 | 0.09938 | 1.172 |
Discussion
Anaemia is associated with a poor prognosis in cancer patients due to its impact on the patient's quality of life and overall health. Anaemia can contribute to fatigue, reduced immune function, impaired cognitive function, and increased risk of infection. In addition, anaemia may be a sign of advanced cancer, which can lead to a decrease in overall survival rate [7,14,16]. Prevalence of anaemia is variable in cancer patients. Studies have reported prevalence of 30 to 90%. Type and stage of cancer, pre and post treatment assessment and also definition of anaemia are some of the factors which impact the reported prevalence of anaemia [17,18].
The National Cancer Institution (NCI) grading of anaemia is defined as follows: “mild (Grade 1), Hb from 10 g/dL to the lower normal limits; moderate (Grade 2), Hb 8.0–9.9 g/dL; severe (Grade 3), Hb less than 8 g/dL to 6.5 g/dl; life-threatening (Grade 4), Hb less than 6.5 g/dL. Baseline anaemia is defined as having Hb levels of less than 120.0 g/l for males and less than 110.0 g/l for females at presentation before any cancer related treatment [19]. Patients with GI malignancies especially gastric and colorectal cancer often present with anaemia. Up to 50% of gastric cancer patients have anaemia at presentation as per some studies [6]. Our study reported that the majority of patients had anaemia at presentation. Haemoglobin (Hb) less than 100 gram per litre was found in 84 (75%) of patients. This is higher than other studies and probably explained by the higher number of patients with advanced disease in our study.
Anaemia is an independent prognostic factor of survival in cancer patients. A systematic review reported that the relative risk of death increased by 19% (95% confidence interval, 10-29%) in anaemic patients with lung carcinoma, by 75% (37-123%) in anaemic patients with head and neck carcinoma, by 47% (21-78%) in anaemic patients with prostate carcinoma, and by 67% (30-113%) in anaemic patients with lymphoma. The overall estimated increase in risk was 65% (54-77%) [7]. A number of studies have assessed preoperative haemoglobin levels and associated morbidity and mortality in patients with gastric cancer. Preoperative anaemia was associated with poor overall survival in stage I, II and III gastric cancer patients [11,12]. In a meta-analysis of Seventeen studies involving 13,154 gastric cancer patients, preoperative anaemia was identified in 36% of patients. Both overall survival and disease-free survival was significantly lower in patients with preoperative anaemia [10]. In patients with advanced metastatic gastric cancer, association of low haemoglobin (Hb) levels and prognosis has been reported in few studies. Qing Wei et al reported correlation between Hb Levels and the prognosis of first-Line chemotherapy in patients with advanced gastric cancer. The median progression free survival was 5.7 months in pts with severe anaemia as compared with 6.4 months for patients with non-severe anaemia (Hb≥8g/dl). The median overall survival was 15.0 months for pts with non-anemia and mild anaemia (Hb≥10g/dl) versus 11.5 months for pts with moderate or severe anemia [20]. In our study we also found association of anaemia with prognosis. The patients with higher Hb (>100 g/L) had better outcomes as compared to patients with lower Hb (less than 80 g/L).
Another study evaluated the impact of anaemia on prognosis of patients treated with 5-fluorouracil (FU)-based first-line chemotherapy in patients with advanced gastric cancer. They reported lower response rates (9%) in patients with Hgb values less than 10g/dl than in patients with Hb > or = 10 g/dl (53%; P less than 0.001) [14]. A retrospective analysis of 598 patients with advanced gastric showed that patients with Hgb level ≤ 80 g/L had a trend toward a shortened median OS and PFS (p = 0.009 and p = 0.049, respectively) [20]. Cancer related anaemia is multifactorial and hence it is important to identify multiple potential treatable causes. Treatment of cancer itself can cause anaemia and may require interruption or delay in treatment. Often the progression of cancer itself is the cause of anaemia. Hence management of cancer related anaemia can be challenging. Apart from the treatment of cancer itself, other management options include erythropoietic agents, iron supplementation or blood transfusions, and nutritional supplementation etc [19].
Treatment of cancer related anaemia can lead to improvement in quality of life as well as better tolerance to anti-cancer treatment and potentially improve treatment efficacy and survival [21,22,23]. However, impact of blood transfusion in gastric cancer patients to correct anaemia is controversial. Some studies show improvement in quality of life however there does not appear any improvement in survival and some even report poor outcomes [22,23,24,25]. Our study showed no association between blood transfusion and prognosis of patients.
Conclusion
Overall, our results suggest that anaemia has a significant negative impact on the overall survival, progression-free survival, and quality of life of patients with advanced gastric cancer. Therefore, identifying and treating anaemia early on in the disease course may be beneficial for improving the outcomes of these patients.
The point prevalence of anaemia in our gastric cancer patients during treatment had an effect on overall survival. The outcome couldn't be improved with RBC transfusion. Our findings indicate the need for a consistent diagnostic and treatment approach to anaemia in this setting.
Declaration of interests
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper. This study was conducted after approval and registration from the respective institution.
References
- Sung H, Ferlay J, Siegel RL, et al. (2020). Global cancer statistics: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA: a cancer journal for clinicians. 2021;71(3):209-249.
Publisher | Google Scholor - Wong MCS, Huang J, Chan PSF, et al. (2021). Global incidence and mortality of gastric cancer, 1980-2018. JAMA Network Open. 4(7): e2118457.
Publisher | Google Scholor - (2022). National cancer institute, SEER data.
Publisher | Google Scholor - CHAU I, NORMAN AR, CUNNINGHAM D, WATERS JS, OATES J. et al. (2004). Multivariate prognostic factor analysis in locally advanced and metastatic esophago-gastric Cancer—Pooled analysis from three multicenter, randomized, controlled trials using individual patient data. Journal of clinical oncology, 22(12):2395-2403.
Publisher | Google Scholor - Maruyama K. (1987). The most important prognostic factors for gastric cancer patients: A study using univariate and multivariate analyses. Scandinavian journal of gastroenterology, 22(S133):63-68.
Publisher | Google Scholor - Tang G, Hart R, Sholzberg M, Brezden-Masley C. (2017). Iron deficiency anemia in gastric cancer: A single site retrospective cohort study. Journal of clinical oncology, 35:188.
Publisher | Google Scholor - Caro JJ, Salas M, Ward A, Goss G. (2001). Anemia as an independent prognostic factor for survival in patients with cancer: A systemic, quantitative review. Cancer, 91(12):2214-2221.
Publisher | Google Scholor - Varlotto J, Stevenson MA. (2005). Anemia, tumor hypoxemia, and the cancer patient. International journal of radiation oncology, biology, physics, 63(1):25-36.
Publisher | Google Scholor - Harrison L, Blackwell K. (2005). Hypoxia and anemia: Factors in decreased sensitivity to radiation therapy and chemotherapy? The Oncologist, x9:31-40.
Publisher | Google Scholor - Huang X, Yang Y, Chen Y, et al. (2019). Preoperative anemia or low hemoglobin predicts poor prognosis in gastric cancer patients: A meta-analysis. Disease Markers, 2019:7606128-9.
Publisher | Google Scholor - Kunishige T, Migita K, Matsumoto S, et al. (2022). The prognostic significance of preoperative anemia in gastric cancer patients. In vivo (Athens), 36(5):2314-2322.
Publisher | Google Scholor - Liu X, Qiu H, Huang Y, et al. (2018). Impact of preoperative anemia on outcomes in patients undergoing curative resection for gastric cancer: A single‐institution retrospective analysis of 2163 chinese patients. Cancer Medicine, 7(2):360-369.
Publisher | Google Scholor - Li W, Zhang J, Liu W, Chen X. (2020). Role of the initial degree of anaemia and treatment model in the prognosis of gastric cancer patients treated by chemotherapy: A retrospective analysis. BMC cancer, 20(1):414.
Publisher | Google Scholor - SE HOON PARK, LEE J, KIM S, et al. (2006). Anemia is the strongest prognostic factor for outcomes of 5-fluorouracil-based first-line chemotherapy in patients with advanced gastric cancer. Cancer chemotherapy and pharmacology, 57(1):91-96.
Publisher | Google Scholor - Busti F, Marchi G, Ugolini S, Castagna A, Girelli D. (2018). Anemia and iron deficiency in cancer patients: Role of iron replacement therapy. Pharmaceuticals, 11(4):94.
Publisher | Google Scholor - Gluszak C, de Vries-Brilland M, Seegers V, et al. (2022). Impact of iron-deficiency management on quality of life in patients with cancer: A prospective cohort study (CAMARA study). The oncologist (Dayton, Ohio), 27(4):328-333.
Publisher | Google Scholor - Ludwig H, Van Belle S, Barrett-Lee P, et al. (2004). The european cancer anaemia survey (ECAS): A large, multinational, prospective survey defining the prevalence, incidence, and treatment of anaemia in cancer patients. European journal of cancer (1990), 40(15):2293-2306.
Publisher | Google Scholor - Steegmann JL, Sánchez Torres JM, Colomer R, et al. (2013). Prevalence and management of anaemia in patients with non-myeloid cancer undergoing systemic therapy: A spanish survey. Clin Transl Oncol. 15(6):477-483.
Publisher | Google Scholor - Madeddu C, Gramignano G, Astara G, et al. (2018). Pathogenesis and treatment options of cancer related anemia: Perspective for a targeted mechanism-based approach. Frontiers in Physiology, 9:1294.
Publisher | Google Scholor - Wei Q, Yuan X, Xu Q, Li J, Chen L. et al. (2020). Correlation between hemoglobin levels and the prognosis of first-line chemotherapy in patients with advanced gastric cancer. Cancer management and research, 12:7009-7019.
Publisher | Google Scholor - Cella D, Dobrez D, Glaspy J. (2003). Control of cancer-related anemia with erythropoietic agents: A review of evidence for improved quality of life and clinical outcomes. Annals of oncology, 14(4):511-519.
Publisher | Google Scholor - Schrijvers D. (2011). Management of anemia in cancer patients: Transfusions. The oncologist (Dayton, Ohio), 16(S3):12-18.
Publisher | Google Scholor - T. J. Littlewood, J. W.R. Nortier, B. Rapoport, E. Bajetta, E. Vercammen. (2001). for the Epoetin Alfa Study Group. Effects of epoetin alfa on hematologic parameters and quality of life in cancer patients receiving nonplatinum chemotherapy: Results of a randomized, double-blind, placebo-controlled trial. Journal of clinical oncology, 19(11):2865-2874.
Publisher | Google Scholor - Kaneda M, Horimi T, Ninomiya M, et al. (1987). Adverse effect of blood transfusions on survival of patients with gastric cancer. Transfusion (Philadelphia, Pa.), 27(5):375-377.
Publisher | Google Scholor - Park SH, Nam E, Bang S, Cho EK, Shin DB. et al. (2008). A randomized trial of anemia correction with two different hemoglobin targets in the first-line chemotherapy of advanced gastric cancer. Cancer Chemother Pharmacol, 62(1):1-9.
Publisher | Google Scholor - Ye X, Liu J, Chen Y, Wang N, Lu R. (2015). The impact of hemoglobin level and transfusion on the outcomes of chemotherapy in gastric cancer patients. International journal of clinical and experimental medicine, 8(3):4228-4235.
Publisher | Google Scholor