Research Article
Primary Hydatid Cyst of the Pancreas
- Lada Paul Eduardo 1*
- Badra Roberto 2
- Janikow Christian 3
- Janikow Christian 3
- Caballero Fabián 3
- Sánchez Martín 3
- Martínez Peluaga Julián 3
- Casares Gonzalo 3
- Rojas Alejandra 3
- Mazzei Fernando 4
- Matcoski Florencia 4
- Flórez Nicollini Francisco 3
1General Surgery Professor, General Surgery Service "Pablo Luis Mirizzi", National Hospital of Clinics, Faculty of Medical Sciences, UNC, Córdoba, Argentine.
2General Surgery Service, Allende Sanatorium, Córdoba, Argentine.
3General Surgery Service, Private Clinic Caraffa, Córdoba, Argentine.
4General Surgery Resident, General Surgery Service "Pablo Luis Mirizzi", National Hospital of Clinics, Faculty of Medical Sciences, UNC, Córdoba, Argentine.
*Corresponding Author: Lada Paul Eduardo, General Surgery Professor, General Surgery Service
Citation: Lada P Eduardo, Roberto B, Christian J, Diego T, Fabian C, et. al. (2024). Primary Hydatid Cyst of the Pancreas, Clinical Research and Reports, BioRes Scientia Publishers. 2(5):1-5. DOI: 10.59657/2995-6064.brs.24.030
Copyright: © 2024 Lada Paul Eduardo, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: May 27, 2024 | Accepted: June 22, 2024 | Published: July 17, 2024
Abstract
Background: Pancreatic primary hydatic cysts are rare not to say exceptional, with their incidence in large series being only 0.2% to 0.3%
Setting: General Surgery Service "Pablo Luis Mirizzi" of the National Hospital of Clinics, Allende Sanatorium and Caraffa Clinic of Córdoba.
Design: Retrospective and cooperative.
Methods: Between December 2000 and December 2019, 9 patients with primary pancreatic hydatic have been treated surgically, with 5 of the male sex and the remaining four of the female sex, with an average age of 39.4 years. In relation to the clinic, all patients had abdominal pain, accompanied by vomiting, bloating and fever. In three they had a palpable abdominal mass. All were asked for laboratory and hydatic tests, highlighting in 6 of the 9 patients tested positive.
Results: All patients with abdominal ultrasound, abdominal CT and a patient were studied for CPRMN plus MRI of the abdomen. Abendazole was previously treated prior to surgical treatment in all cases. In relation to surgical treatment, the traditional unroofing and drainage of the cyst was carried out with the Mabit-Lagrot technique in 6 opportunities and in 3 with the Goinard Technique.
Conclusion: The location of hydatic cysts in the pancreas is rare. Diagnosis is based primarily on imaging studies, in addition if they correlate with epidemiology and positive hydatic serology. Treatment of the pancreas hydatic cyst is surgical.
Keywords: pancreatic primary hydatic cysts; diagnosis; mabit-lagrot technique; goinard technique
Introduction
Hydatic cyst is a zoonosis produced in our region by Echinococcus granulosus, in its larval stage produces cysts forms in intermediate or accidental guests like humans. In its adult stage lives in the canids guts (definite guests) being a public health problem [1]. Liver and lungs are the most frequent organs involved but there are other uncommon localizations like kidney, spleen and thyroid that they reach by arterial route skipping liver and lungs filters. [2-4]. Pancreatic localization is extremely rare but even exceptional. In large series of primary hydatic cyst they reach 0, 2-0, 3%, there are a few cases in the literature [5, 6].
Methods
Between December 2000 and December 2019 in a cooperative work that includes General Surgery Service “Pablo Luis Mirizzi” from the National Clinic Hospital, Sanatorium Allende and Caraffa Private Clinic from Córdoba Argentine, have been operated 9 patients with primary hydatid cyst of the pancreas, 5 male patients (55%) and 4 female (44%) whit a median age of 39,4 years (range between 18 and 71 years) (Table 1). All patients had abdominal pain as hyphen symptom (100%), vomiting showed up in 44%, abdominal distension in 33,3% and fever in 22,2%. Physical exam showed abdominal mass in 3 patients (33,3%). Everyone underwent laboratory test and specific hydatidosis with 6 positive cases (66,6%) (TABLE 1). The 9 patients underwent abdominal Ultrasound (US) and abdominal Computer Tomography (CT), one patient was studied with magnetic resonance cholangio-pancreatography (MRCP). The patients came from endemic regions.
Results
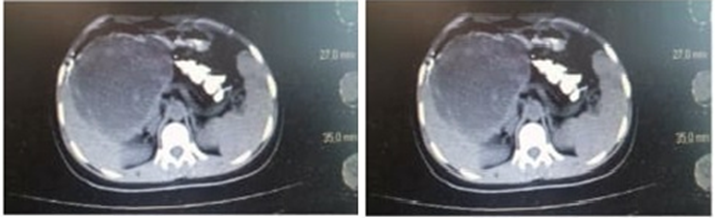
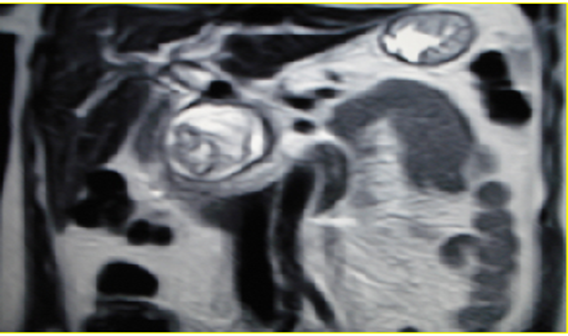
In 4 cases cyst location by US was in pancreatic body and tail (44.4%), other 4 cases in pancreatic head (44.4%) and 1 case in pancreatic head and body (11.1%). CT confirmed cyst diagnosis, those with location in body and tail had medium size of 126 mm x 87 mm of diameter (range between 70 x 180 mm) and they morphology was unilocular and multilocular. Cyst from head of the pancreas showed medium size of 93mm x 72 mm (range between 40 x 120 mm), they also where unilocular and multilocular. The cyst from head and body of the pancreas had 120 mm x 130 mm of size and was unilocular. (Figure 1) (Figure 2). The patient who received MRCP showed the scolex inside the cyst and common bile duct without parasite (Figure 3).
Table 1: Abdominal Cases
| Age (yeras) | Gender | Clinical findings | Imagen | Location | Surgery |
| 21 | F | Abdominal pain. Abdominal mass. | US and CT. (103 x 70 mm) | Body and tail. | Mabit-Lagrot- Good evolution |
| 26 | M | Abdominal pain, fever, abdominal distention | US and CT. (120 x 80 mm) | Head. | Goinard. Pancreatic leak. |
| 60 | M | Dispepsia and abdominal pain. | US and CT. (97 x 70 mm) | Body and tail. | Mabit-Lagrot. Good evolution. |
| 46 | M | Abdominal pain and vomiting. | US and CT. (125 x 89 mm) | Body and tail. | Mabit-Lagrot. Good evolution. |
| 18 | F | Abdominal pain and abdominal mass. | US and CT. (120x130x110mm) | Body and head. | Goinard. Good evolution |
| 38 | F | Abdominal pain, abdominal distention and vomiting. | US and CT. (100 x 90 mm) | Head. | Mabit-Lagrot- Good evolution. |
| 57 | M | Abdominal pain, abdominal mass and fever. | US and CT. (180x120x110mm) | Body and tail. | Goinard. Good evolution. |
| 71 | M | Abdominal pain, abdominal distention and vomiting. | US and CT, (95x80x70 mm) | Head. | Mabit-Lagrot. Pancreatic leak. |
| 57 | F | Abdominal pain and vomiting. | US, CT and MRCP (40X 60X 50 mm) | Head. | Mabit-Lagrot. Good evolution. |
Before surgery the patients received Abendazol 200mg per day for 2 weeks. In surgery at first the patients underwent an evacuation puncture with subsequent sterilization. In 6 of them they received Mabit-Lagrot technique with roofing and drainage (66.6%) and in 3 of them they cyst cavity was filled up with epiploon as Goinard technique indicates (33.3%) (Table 1). They were no mortality. The morbidity was low and in relation to the general anesthesia. Two patients with pancreatic head cyst showed pancreatic leak (22.2%), one of them during 5 days (operated with Goinard technique) and the other during 7 days (operated with Mabit-Lagrot technique). Follow up showed favorable evolution without recurrence of the disease, the underwent hydatid test, abdominal US and abdominal CT.
Figure 1: Abdominal CT. Cyst in body and tail of the pancreas.
Figure 2: Abdominal CT. Cyst in the head of the pancreas.
Figure 3: MRCP. Cyst that shows scolex inside and common bile duct without stones.
Discussion
Human’s infections happen because of the accidental ingestion of parasite eggs coming from others intermediate guest. In the guts the eggs release the exacanth embryo that crosses through intestine wall to reach the liver and lungs by the portal vein [1]. Pancreatic infection is extremely rare but even exceptional, big series of primary Hydatid estimates 0.2 to 0.3% in frequency [5, 6]. Some authors argue that the average surgical incidence of this zoonosis ranges from 15 to 12.6/100,000 habitants per year, being a major public health problem [7], considering that the incidence in the liver is 60% to 70. But when it spreads to other viscera such as the pancreas occurs through hematic route. For a hydatid cyst to be considered as primary of the pancreas must possess an adventitious developed at the expense of tissue proper to the gland, they are usually unique, characteristics that differentiate them from the hydatid cysts secondary to a multiple hydatic or a pancreatic settlement by contiguity from any other intra-peritoneal location [8]. Chinya et al. [9] estimates cyst localizations of the pancreas 50-58% in the head, 24-34% in the body and 19% in the tail. In our series we disagree whit Chinya because we found 4 cases in body and tail (44,4%), 4 cases in head (44,4%) and 1 in head and body of the pancreas (11,1%).
Clinical manifestations include acute and chronic abdominal pain, abdominal mass and sometimes asymptomatic cases discovered by imagine studies such as abdominal US and CT. Most of this cyst grows up to a big mass and simulates a tumours syndrome [1]. Some complications are jaundice, infections of the cyst, chronic pancreatitis, rupture of the cyst, fistula to neighboring organs, portal vein hypertension and acute pancreatitis [6, 10, 11]. In our experience abdominal pain was the hyphen symptom, cyst located in the head also showed vomiting and abdominal distention, those with body and tail localization presented also as an abdominal mass. Diagnosis can be done with imagine such as an abdominal US and CT with contrast. The correlation with epidemiological data is essential to approach the diagnosis such as a positive serological hydatid study [12], but a negative result doesn’t reject hydatid cyst. Imagine findings for hydatid cyst includes wall calcification and presence of vesicles in the inside [12]. The absence of this sings must suspect Serous and Mucinous Cyst adenocarcinoma of the pancreas and sometimes anatomo pathological study is necessary to make the diagnosis. CT is useful to establish the relation of the cyst with pancreatic vessels and common bile duct [13]. Some authors [13, 14] gives big value to the MRCP in the suspicious of a cyst-to-bile duct fistula. Zalequett et al [15] describes in T2 an active cyst and the ring sign including the vesicles in the inside as a pathognomonic diagnosis. If diagnostic dude persists, the US endoscopy can be useful to differentiate the content of the cyst from others pancreatic tumors [12]. We found by abdominal US thickening wall cyst, membrane cyst and vesicles inside, all of them pathognomonic signs of Hydatid cyst and in correlation to the Garbi type III [16] or CE2 from WHO-IWGE [17]. Abdominal CT confirmed US findings. The MRCP performed in one patient showed scolex inside the cyst and a normal bile duct without cyst-to-bile fistula.
Treatment of a pancreatic Hydatic cyst is surgery. The surgery depends because of the localization of the cyst and the presence or absence of a pancreatic fistula. Those located in the body and tail received Mabit-Lagrot technique that includes roofing and drainage of the cyst with or without filling it with omentum (Goinard). It has been an effective option according to the literature [14, 18] despite other postures in favor for resection [19]. In the OR room we perform an evacuation puncture of the cyst following a sterilization with hypertonic solution. We also perform a frozen sample of the cyst wall to confirm diagnosis and chose surgical technique [18, 20]. For some pancreatic surgeons [14, 18], pancreatic head cyst must receive conservative treatment (Evidence Level 5, Grade recommendation D). When it is involving neighbor organs and or Aorta or when the dissection could be dangerous, the surgical treatment must be Mabit-Lagrot procedure with or without omentum filling (Goinard procedure). Whippel procedure must be leave for selective cases [21]. In lesions of the body and tail of the pancreas, some authors [19, 21] argue that the trend is radical surgery (Evidence level 5, grade recommendation D), if there is a fistula between the main duct and the cyst, a resective procedure or an anastomosis of the cyst with digestive tract could be performed. On the contrary, there is no fistula detection procedures with drainage or with omentum are as suggested (Mabit Lagrot-Goinard). Treatment with PAIR is only indicating in those cases with no clinical conditions and high anesthesia risk, despite the probability of 10% of peritoneal dissemination and anaphylaxis [22]. Other authors recommend Albendazole treatment one week before surgery and continuing 2 months after the procedure (Evidence Level 2, Grade recommendation C), the sensibility with Albendazole during 4 to 6 months have been informed in 60 to 90% of successful [24].
Conclusion
Pancreatic localization of Hydatid cyst is extremely rare reaching. Mostly localized in the head of the pancreas in 50 to 58% of cases, in body in 24 to 34% and y tail in 19%. The diagnosis is based in imagine findings like abdominal US, CT and MRCP and correlated with epidemiological and serologic results. The treatment of Hydatid cyst of the pancreas is surgery and the technique depends on the location.
Conflicts of Interest
Authors declare no interest conflicts.
References
- Lada PE, Cornet M, Florez Nicollini F, Martinessi V, Gramatica L. (2000). Quistes hidatídicos del páncreas. Pren. Méd. Argent, 87:847-851.
Publisher | Google Scholor - Lada PE, Lermite E, Hennekinne-Mucci S, Étienne S, Pessaux P, Arnaud JP. (2005). Kyste hydatique primitif de la thyroïde, une localisation inhabituelle de l’hydatidose. Presse Med, 34:580-581.
Publisher | Google Scholor - Manterola C, Vial M, Fonseca F, Carrasco R, Bustos L, Muñoz S, et al. (2002). Hidatidosis abdominal de localización extra hepática. Características clínicas y evolución de una serie de casos. Rev. Chilena de Cirugía, 5(2):128-134.
Publisher | Google Scholor - Abi F, Fares F, Khaiz D, Bouzidi A. (1989). Unusual localizations of hydatid cysts. Apropos of 40 cases. J. Chir, 126:307-312.
Publisher | Google Scholor - Cosme A, Orive V, Ojeda E, Aramburu V, Irazusta M, Arenas J. (1987). Hydatidid cyst of the head of the pancreas with spontaneous fistula to the duodenum. Am J Gastroenterol, 82:1311.
Publisher | Google Scholor - Ternengo D, Casares G, Sánchez Tasone C, Moretti G, Caballero F, Lada PE et al. (2017). Prymary hydatid cyst of the pancreas. Rev. Fac. Cienc. Médi, 74(1):33-36.
Publisher | Google Scholor - Dziri C. (2001). Hydatid disease A continuing surgical health problem. World. J. Surg, 25:1-3.
Publisher | Google Scholor - Kattan YB. (1975). Hydatid cysts in pancreas Br. Med. J, 4:729-730.
Publisher | Google Scholor - Chinya A, Khanolkar A, Kumar J, et al. (2015). Isolated hydatid cyst of the pancreas masquerading as pancreatic pseudocyst. BMJ. Case Rep, 11.
Publisher | Google Scholor - Kowalczyk M, Kurpiewski W, Zieliński E, Zadrożny D, Klepacki L, Juśkiewicz W, et al. (2019). Un caso raro de la ubicación simultánea de Echinococcus multilocularis en el hígado y la cabeza del páncreas: análisis del informe del caso y revisión de la literatura. BMC Infectious Diseases, 19: 661-664.
Publisher | Google Scholor - Alsaid B, Alhimyar M, Rayya F. (2018). Pancreatic Hydatid Cyst Causing Acute Pancreatitis: A Case Report and Literature Review. Case Reports in Surgery.
Publisher | Google Scholor - Bedioui H, Chebbi F, Ayadi S, Daghfous A, Bakhtri M, Jouini M, et al (2008). Kyste hydatique primitif du pancréas: diagnostic et modalités chirurgicales. À propos de trois cas. Gastreoenterol. Clin. Biol, 32 (1):102-106.
Publisher | Google Scholor - Stojkovic M, Rosenberger K, Kauczor HU, Junghanss T, Hosch W (2012). Diagnosing and staging of cystic echinococcosis: how do CT and MRI perform in comparison to ultrasound? PLoS Negl. Trop. Dis, 6:1880.
Publisher | Google Scholor - Dziri C, Dougaz W, Bouasker I (2017). Surgery of the pancreatic cystic echinococcosis: systematic review. Transl. Gastroenterol. Hepatol, 2:105-112.
Publisher | Google Scholor - Zalaquett E, Menias C, Garrido F, Vargas M, Olivares JF, Campos D et al (2017). Imaging of Hydatid Disease with a Focus on Extrahepatic Involvement. Radiographics, 37:901-923.
Publisher | Google Scholor - Gharbi HA, Hassine W, Brauner MW, Dupuch K (1981). Ultrasound examination of the hydatic liver. Radiology, 139:459-463.
Publisher | Google Scholor - WHO Informal Working Group (2003). International classification of ultrasound images in cystic echinococcosis for application in clinical and field epidemiological settings. Acta Trop, 85: 253-261.
Publisher | Google Scholor - Karaman B, Battal B, Ustunsoz B, Ugurel MS (2012). Percutaneous treatment of a primary pancreatic hydatid cyst using a catheterization technique. Korean J. Radiol, 13:232-236.
Publisher | Google Scholor - Akbulut S, Yavuz R, Sogutcu N, Kaya B, Hatipoglu S, Senol A, et al (2014). Hydatid cyst of the pancreas: report of undiagnosed case of pancreatic hydatid cyst and brief literature review. World. J. Gastrointest. Surg, 6:190-200.
Publisher | Google Scholor - Warshaw AL, RutledgePL (1987). Cystic tumours mistaken for pancreatic pseudo cysts. Ann. Surg, 205(4):393-398.
Publisher | Google Scholor - Bouasker I, Zoghlami A, Ben Achour J, Najah H, Bedoui R, Hani ML, et al (2009). Hydatid cysts of the pancreas, report of two cases. Tunis Med, 87:155-158.
Publisher | Google Scholor - Kısaoğlu A, Özoğul B, Atamanalp SS, Pirimoğlu B, Aydınlı B, Korkut E (2015). Incidental Isolated Pancreatic Hydatid Cyst. Turkiye Parazitol. Derg, 39:75-77.
Publisher | Google Scholor - Dziri C, Haouet K, Fingerhut A (2004). Treatment of hydatid cyst of the liver: where is the evidence? World. J. Surg, 28:731-736.
Publisher | Google Scholor - Safioleas MC, Moulakakis KG, Manti C, Kostakis A (2005). Clinical considerations of primary hydatid disease of the pancreas. Pancreatology, 5:457-461.
Publisher | Google Scholor