Case Report
Posterior Aesthetic Restoration in Direct Technique: A Case Report
- Ameni Chadlia Belghith *
- Amira Kikly
- Foued Brigui
- Wided Glii
- Neila Zokkar
- Nabiha Douki
Department of Dentistry, University Hospital, Sahloul, Tunisia Faculty of Dental Medicine, Research Laboratory LR12ES11, University of Monastir, Avicenna Street, Tunisia.
*Corresponding Author: Ameni Chadlia Belghith,Department of Dentistry, University Hospital, Sahloul, Tunisia Faculty of Dental Medicine, Research Laboratory LR12ES11, University of Monastir, Avicenna Street, Tunisia.
Citation: Ameni C. Belghith, Kikly A, Brigui F, Wided G, Zokkar N, et al. (2024). Posterior Aesthetic Restoration in Direct Technique: A Case Report. Dentistry and Oral Health Care, BioRes Scientia Publishers, 3(1):1-10. DOI: 10.59657/2993-0863.brs.24.020
Copyright: © 2024 Ameni Chadlia Belghith, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: December 15, 2023 | Accepted: December 30, 2023 | Published: January 02, 2024
Abstract
In modern dental practice, advances in adhesive techniques, coupled with increased attention to the aesthetic qualities of dental restorations and the adoption of a minimally invasive approach to dentistry, have had a major influence on the treatment plan in both the posterior and anterior regions. In recent years, posterior composites have generally been preferred for restorations of posterior teeth using direct methods due to their advantages such as the single visit and short application time, aesthetics, ability to protect dental tissue during preparation, and the fact that they are less expensive compared to indirect methods. The direct Composite Resin Restorations meets the biological, functional and aesthetic requirements of current adhesive dentistry, but its sensitivity to operating conditions requires great rigor. A patient in whom the clinical examination revealed the presence of reversible pulpitis on a posterior tooth requiring dentinal curettage and restoration by direct composite restoration using the "composite up" technique. An operating methodology with a strict protocol makes it possible to obtain reproducible results. The operating protocol for this technique consists in reconstructing the proximal wall with the enamel composite, filling the deep two-thirds of the cavities with a dent in substitute and restoring the occlusal anatomy by adding mini-increments of composite on each cuspidal side. The quality of an aesthetic restoration by direct technique integrates the concept of colorimetry, morphology, anatomy and surface condition. The objective of our work is to illustrate, through a clinical case, a simple protocol for aesthetic restoration of posterior teeth using the direct technique.
Keywords: aesthetic restoration; posterior teeth; resin composite; bonding systems
Introduction
The search for a restorative material that can replace and mimic missing tooth tissue has been fruitful over the last few decades. With the adoption of minimally invasive dentistry, materials research has focused on improving bioactive materials. Recent developments have significantly improved the properties of dental materials [1]. Nowadays, various dental materials have been developed, such as glass ionomer cements, resin-based composites, and so on. Among these dental restorative materials, resin-based composites have been widely used because of their ability to withstand high compressive forces in the mouth and their good aesthetic properties [2]. Infarct, the direct composite aesthetic restoration of posterior teeth is becoming more and more popular in our daily practice. This technique is indicated for the restoration of small and medium-sized cavities in premolars and molars. For its optical and mechanical properties, composite is now the alternative of choice for a high-quality permanent restoration [3]. And the incremental lamination technique is still considered the "gold standard" today. The composite is applied in successive layers, with a maximum thickness of 2 mm. This is due to the polymerization characteristics and limited light-curing depth of these materials. Even in the posterior region, composites of different shades or degrees of opacity/translucency (dentin and enamel composites) can be used, as part of the polychromatic technique, with high aesthetic quality to optimize the optical results of this direct restoration. The technique of "composite up" meets the biological, functional and aesthetic requirements of current adhesive dentistry, but its sensitivity to operating conditions requires great rigor. The objective of our work is to illustrate, through a clinical case, a simple protocol for the aesthetic restoration of posterior teeth in direct technique.
Clinical Case 1
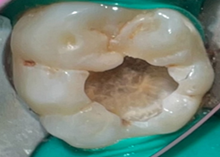
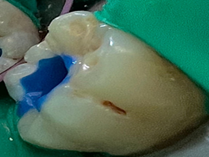
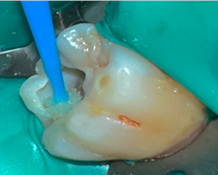
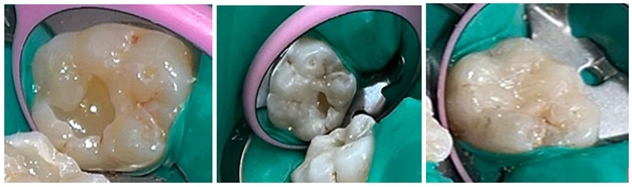
A 21-year-old girl patient consulted the dental department of Sahloul Hospital for pain caused by cold and sugar in relation to the right mandibular first molar (46). On clinical examination, Ex buccally nothing was to be reported. The tooth (46) presented an occlusal caries Sista 1.3(Fig.1) and was slightly sensitive to transverse percussion. The response to the cold test was pain that stopped when the stimulus was stopped and the diagnosis of a reversible pulpitis was retained. The treatment consists on a perfect isolation of the tooth, a curettage of the caries, an indirect pulp capping and an aesthetic direct restoration using a nanohybrid resin. The first step was the shade selection: Shades are always taken in natural light, before the rubber dam is placed. This is because colored reflections from the dam and dehydration of the tooth can distort the choice of shade. The next step was to isolate the tooth with a rubber dam, cure the carious lesion (Fig.2) and indirectly cap the pulp with calcium hydroxide Cal LC® (Fig.3). Orthophosphoric acid 37% was applied to the enamel for 20 seconds to improve retention (Fig.4).
Figure1: Preoperative clinical view
Figure 2: Clinical view of the cavity after dentine curettage
Figure 3: Indirect pulp capping with Cal LC® calcium hydroxide
The adhesive ALL-BOND UNIVERSAL® BISCO was applied (Fig.5), spread with a jet of air and photopolymerized for 20 seconds (Fig.6). It must be ensured that all cavity areas are covered by the adhesive.
Figure 4: Enamel etching for 20 seconds
Figure 5: Application of adhesive (ALL-BOND UNIVERSAL® BISCO).
Figure 6: Light curing for 20sec
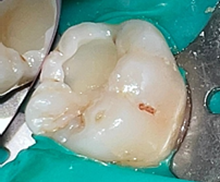
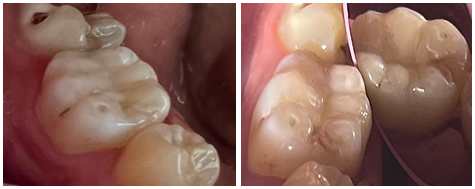
The next step is the filling of the deep two-thirds of the cavity in a single step by dentin substitute Any-Com Flow® fluid resin in order to reduce the retraction to the polymerization (Fig.7) then the restoration of the occlusal anatomy in order to ensure the aesthetics and the function by adding small increments of composite on each internal cuspid side that are light-cured with a 10-second flash in order to freeze the material (Fig.8). Successive additions are repeated until the restoration of the entire occlusal face with its furrows and dimples and light-curing final 40 seconds is performed at the end of the restoration. DeOx™ designed to prevent the formation of an oxygen-inhibited layer on the surface of resin materials. Once the dam was deposited, we proceeded to check the occlusion (Fig.9), finish and polish. Macro-geography and micro-geography are customized using fine- or medium-grain diamond burs, followed by roughing to give us a smoother surface, which is achieved using disks with decreasing grain size or polyester abrasive strips, and then finishing with a good polishing: siliconized tips and polishing paste are the most commonly used (astropol System) or brushes with bristles containing silicon carbide abrasive particles (Fig: 10.11).
Figure 7a: Filling the deep two thirds of the cavity with Any-Com Flow® fluid resin
Figure 7b: Edification of the cusps (BISCO Aelite™ Aesthetic Universal Kit) and light-curing for 20sec.
Figure 8: Occlusion control with articulating paper.
Figure 9: Finishing and polishing
Figure 10: Postoperative clinical view
Discussion
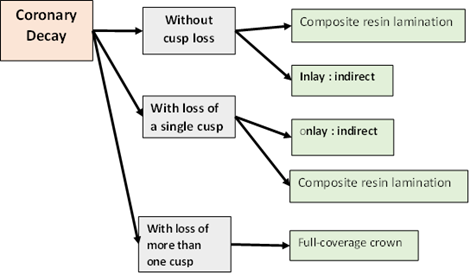
Maximum preservation of hard dental tissue using direct composites as an alternative to indirectly and partial crowns is one of the main advantages and key elements when restoring severely damaged teeth with cusp involvement. However, when the replacement of three or four cusps is required in very large defects, indirect restorations find their indications (Fig: 11). In fact, studies on the longevity of laminated composites on posterior teeth have shown acceptable performance and have qualified this treatment option as a good alternative to conventional indirect restorative techniques [4].
Figure 11: decision-making chart for tissue loss
The preparation consists of the complete removal of carious and pigmented tissue that may compromise the esthetic result. The preparation must not include a bevel at the Cavo superficial angles to avoid any cracking of the composite lamina. For this reason, it should be close to 90° (up to 120°) to ensure clean edges and internal angles should be rounded to reduce stress concentration. Chlorhexidine 2% was used to disinfect the cavity prior to adhesive application, but there are many other products available. However, only a few products have been thoroughly tested [5]. In fact, a disinfectant must be able to properly sanitize the dental cavity without affecting adhesion. Its effect depends not only on the properties of the disinfectant, but also on the type of substrate, adhesive system and restorative material used. In the case of chlorhexidine, the results were essentially positive, and CHX pre-treatment was shown to maintain adequate adhesion to dentin. According to the American Dental Association, if after 18 months the retention rate is at least 90%, restorations achieve full acceptance. Following these guidelines, the study by Dutra-Correa et al. was able to achieve full acceptance, as the retention rate of the restoration after 18 months was over 90% when tested with a 2% chlorhexidine solution. On the other hand, there is no consensus for sodium hypochlorite, as some reported positive results with maintained or increased bond strength values, while others reported decreased results. The decrease in bond strength may also be due to the oxygen released by NaOCl molecules, which can inhibit adhesive polymerization and compromise the mechanical performance of bonded surfaces. As for EDTA, studies have reported a maintenance or even an increase in the average adhesion strength regardless of the adhesive system used, but more in-depth studies are needed. Another possible method of cavity disinfection is laser irradiation. According to some studies, irradiation of the dentin surface helps to improve microhardness, increase resistance to demineralization and reduce dentin permeability, thus minimizing bacterial penetration into the pulp. However, results on the use of lasers as oral antiseptics are inconsistent [6,7]. Composite resins can be classified according to different criteria like viscosity, in fact different viscosities (liquid, medium, compressible) make it possible to meet different needs. Fluid composites spread more easily over the cavity walls; a phenomenon known as wettability. But because of their consistency, mechanical properties are often inferior to those of medium-viscosity composites, and polymerization shrinkage is often greater. Polymerization method is also a criterion to consider. There are materials capable of chemical polymerization, where polymerization takes place by chemical reaction. There are also composite resins capable of light-curing. This represents the majority of composite resins. The resin is packaged as a paste containing a photo initiator (for example camphor quinone). The photopolymerization reaction is initiated with a lamp. Finally, there are also dual-setting materials. Furthermore, filler dimensions are a consistent way of classifying different types of composite resins, as fillers determine many material properties. Macro-filled materials have good mechanical properties but poor surface finish and wear resistance. Microfilmers include silica microfilmers with an average size of 0.04 microns, and can be homogeneous or heterogeneous, or even reinforced. Hybrid composites combine both silica microparticles and large or small glass particles of varying composition, size and shape. The composite resin itself is divided into several parts due to its diversity (presence or absence of nanofillers / particle size). Indeed, nano-filled composites are the current choice, as they offer a wide range of shades, good mechanical properties, optimizing posterior restorations, good polish ability which improved aesthetic appearance. Because of these multiple advantages, we used a nanofiller resin in our clinical cases.[8] Recently, new "Bulk Fill" bulk resins with higher translucency, lower filler content and new photocatalysts have been placed in 4 to 5 mm increments, and studies have shown marginal adaptation similar to the oblique layering technique in 2 mm increments. These composites are indicated for posterior cavities, with multiple advantages such as simplification of the procedure and therefore faster obturation, since the composite layer used is 4 mm instead of 2 mm .In fact, Bulk Fill composites are characterized by an increased depth of polymerization thanks to its three features: increased translucency , specific photo initiators and stress modulators and a higher degree of polymerizations well as better adaptation of the deep layer with the pulp cavity wall. However, this material does have its limitations, including aesthetic appearance, translucency requiring the use of a shade Modificator to mask dentin discolorations with amalgam, low shade nuance restricting them to posterior use only, and the need to control polymerization depth, which may be insufficient if exposure time is short. with low-power curing lamp [3,9]. In the past, the classification of adhesive systems was based on chronology. The new classification takes into account the principle of action and the number of clinical steps. The bond between tooth and restorative material is achieved by a number of systems: self-etching systems or SAMs, and M&Rs. The difference between these two types lies in the use of the orthophosphoric acid in the M&R system, which will be rinsed off, whereas in the SAM system, the mordanting acid is included in the adhesive. The adhesive is the biological material that forms the interface between the tooth and the restorative material, providing a durable, watertight bond between the tooth surfaces and the material. Generally speaking, there are two types of adhesion: Mechanical adhesion/micro-locking and Chemical bonding II or M&R III systems are mainly used, as the dentin surface to be restored is larger in posterior teeth. Even if a self-etching system is used, several authors recommend a 20S etch at the enamel level to improve retention. However, SAMs are mainly used on living teeth, since the risk of postoperative sensitivity is lower with this type of adhesive since the infiltration of intra-tubular anfractuosities takes place at the same time as the creation of these anfractuosities by the application of the self-etching agent. Also, by the application of the self-etching agent, the smear layers conserved and it plays a part in resisting to intra-tubular fluid flow and hydrodynamic movements [10]. Four steps are required for the composite up technique, an adhesion protocol that must be rigorous to guarantee bio integration of our future restoration. In the case of site 2 cavities, the proximal wall is constructed in compliance with anatomical and physiological requirements, in particular with a correctly positioned contact point using a formwork system. To reduce polymerization shrinkage, the deep two-thirds of the cavity are filled with dentin substitute and to ensure esthetics and function, the occlusal anatomy is restored. To fill two-thirds of the cavity in a single step, some authors have proposed the use of so-called "sandwich" techniques, the aim of which is to simplify the clinical procedure by reducing the time needed , the number of material additions and polymerization stresses, thanks to the use of materials with a low coefficient of elasticity close to that of dentin [11].The dentine substitute such as fluid composite, glass ionomer cement, or bioventing must be compatible with the bonding system used. Although the effects of Bio dentin on the generation of extracellular matrix proteins have been studied in many cell types involved in dentin regeneration, the opposing effects suggest a reported stimulatory or inhibitory effect. Clinical observations mainly report the formation of reparative tissue for tricalcium silicate cement. Since Bio dentine has physical and clinical properties comparable to those of MTA, secondary criteria such as ease of handling, applicability and faster setting time will be taken into account.[12] For occlusal anatomy reconstruction, small increments of composite are applied to each cuspidal side and light-cured with a 10-second flash to set the material. Successive increments are repeated until the entire occlusal surface, with its grooves and dimples, has been restored. A final 40-second light-cure is applied at the end of the restoration, the grooves can be simulated with make-up shades at the level of the final layer [5]. For better polymerization, it's best to use oxygen barrier solution such as DeOx™ to prevent the formation of an oxygen-inhibited layer on the surface of resin materials [13]. In fact, restoring with mini-increments covering fewer cavity walls reduces the surface area to be bonded and improves the cavity configuration factor (the c-factor), while 2mm-thick increments allow sufficient polymerization of the material, resulting in fewer free monomers and the risk of gaps and leakage. Finishing and polishing is a very important step because it affects the marginal integrity of the resin restoration and help maintain its seal, thus preventing small cracks and affecting the strength of the material. Most authors recommend finishing after 24 hours, until polymerization is complete, to reduce the risk of leakage. However, newer composites cure faster and can therefore be finished at the same time [14].
Conclusion
The evolution of adhesive dentistry has led to the development of a wide variety of materials, with improvements to optimize results while ensuring the concept of biomimicry. However, despite the advantages of the incremental stratification technique, it remains operator-dependent, requiring a rigorous protocol and a very long operating time, especially in the case of large posterior cavities. The longevity of the restoration can be affected by a number of factors, including age, parafunction, patient motivation and hygiene, and the volume and position of the composite on the dental arch.
References
- Bayazit EÖ, Başeren M, Meral E. (2023). Clinical comparison of different glass ionomer-based restoratives and a bulk-fill resin composite in Class I cavities: A 48-month randomized split-mouth controlled trial. Journal of dentistry, 131:104473.
Publisher | Google Scholor - Pratap B, Gupta RK, Bhardwaj B, Nag M. (2019). Resin based restorative dental materials: Characteristics and future perspectives. Japanese Dental Science Review, 55(1):126-138.
Publisher | Google Scholor - Borgia E, Baron R, Borgia JL. (2017). Quality and Survival of Direct Light-Activated Composite Resin Restorations in Posterior Teeth: A 5- to 20-Year Retrospective Longitudinal Study. Journalof Prosthodontics, 28(1):195-203.
Publisher | Google Scholor - ManhartJ. (2015). Cusp replacement with an extensive posterior direct restoration using a nanohybrid bulk-fill ormocer. International Dentistry – African Edition, 9(3):6-16.
Publisher | Google Scholor - KoubiSA, Brouillet JL, Pignoly C. (2005). Restaurations esthétiques postérieures en technique directe. EMC-Odontologie, 1(4):340-347.
Publisher | Google Scholor - Coelho A, Amaro I, Rascão B, Marcelino I, Paula A, Saraiva J, Spagnuolo G, Ferreira MM, Marto CM, Carrilho E. (2020). Effect of cavity disinfectants on dentin bond strength and clinical success of composite restorations—a systematic review of in vitro, in situ and clinical studies. International Journal of Molecular Sciences, 22(1):1-27.
Publisher | Google Scholor - Fibryanto E, Suprastiwi E, MeidyawatiR, Gunawan HA, Herda E. (2019). The Effect of Sodium Hypochlorite Irrigation on Dentin’s Collagen and Shear Bond Strength of Composite Resin to Dentin. Journal of International Dental & Medical Research, 12:111-116.
Publisher | Google Scholor - RandolphLD, PalinWM, Leprince JG. (2018). Composition of dental resin-based composites for direct restorations. Dental Composite Materials for Direct Restorations, 11-24.
Publisher | Google Scholor - Veloso SRM, Lemos CAA, De Moraes SLD, Do Egito Vasconcelos BC, Pellizzer EP, De Melo Monteiro G. (2019). Clinical performance of bulk-fill and conventional resin composite restorations in posterior teeth: a systematic review and meta-analysis. Clinical oral investigations, 23:221-233.
Publisher | Google Scholor - Meerbeek B, Yoshihara K, Van Landuyt K, Yoshida Y, Peumans M. (2020). From Buonocore’s Pioneering Acid-Etch Technique to Self-Adhering Restoratives. A Status Perspective of Rapidly Advancing Dental Adhesive Technology. J Adhes Dent, 22(1):7‑34.
Publisher | Google Scholor - Chandrasekhar V, RudrapatiL, Badami V, Badami V, Tummala M. Incremental techniques in direct composite restoration. Journal of conservative dentistry, 20(6):386.
Publisher | Google Scholor - Nikfarjam F, Beyer K, König A, Hofmann M, Butting M, Valesky E, Kippenberger S, Kaufmann R, Heidemann D, Bernd A, Zoller NN. (2016). Influence of Bio dentine®-a dentine substitute-on collagen type I synthesis in pulp fibroblasts in vitro, 11(12):1‑20.
Publisher | Google Scholor - AromaaMK. ,Vallittu PK. (2018). Delayed post-curing stage and oxygen inhibition of free-radical polymerization of Di methacrylate resin. Dental Materials, 34(9):1247-1252.
Publisher | Google Scholor - Rathi SD, Nik hade P, Chandak M,Motwani N, Rathi C, Chandak M. (2020). Microleakage in composite resin restoration-a review article. J Evol Med Dent. Sci, 9:1006-1011.
Publisher | Google Scholor