Case Report
Plummer-Vinson Syndrome in A Young African Woman
- Zewdu Hurissa Dadi
- Mengesha Akale Tekle *
- Gezahegn Kefyalew Hirko
Department of Internal Medicine, Arsi University, Asella, Ethiopia.
*Corresponding Author: Mengesha Akale Tekle, Department of Internal Medicine, Arsi University, Asella, Ethiopia.
Citation: Dadi Z. H., Tekle M. A., Hirko G. K. (2024). Plummer-Vinson Syndrome in A Young African Woman, Clinical Case Reports and Studies, BioRes Scientia Publishers. 7(2):1-11. DOI: 10.59657/2837-2565.brs.24.182
Copyright: © 2024 Mengesha Akale Tekle, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: September 04, 2024 | Accepted: September 25, 2024 | Published: October 16, 2024
Abstract
Plummer-Vinson syndrome (PVS) is a classic triad of iron deficiency anemia, dysphagia, and esophageal webs. It is an uncommon cause of dysphagia that classically affects middle-aged women. The literature on PVS is very limited. Here, we present a rare case of PVS in a 20-year-old African woman who presented with easy fatiguability, lightheadedness, and dysphagia for several weeks. Even though PVS is a rare clinical condition, it is worth considering it as a cause of these problems in clinical practice.
Keywords: plummer-vinson syndrome; dysphagia; esophageal webs; anemia
Introduction
The classic triad of iron deficiency anemia, dysphagia, and a cervical esophageal web is known as Plummer–Vinson syndrome or Paterson–Brown–Kelly syndrome [1]. Other common manifestations include glossitis, angular cheilitis, koilonychia, atrophic gastritis, diarrhea, and hoarseness.
The exact cause and pathogenesis of PVS are still unclear. Iron deficiency anemia is the most accepted causal association [2]. PVS is associated with autoimmune diseases such as celiac disease, Crohn's disease, rheumatoid arthritis, and thyroid disease, which suggests the possibility of immune dysregulation during pathogenesis [3].
Most of the patients are white middle-aged women in the fourth to seventh decade of life, but this has been described in children and adolescents [4]. In developed countries, the prevalence of PVS is extremely low due to a decrease in iron deficiency and malnutrition [1,2]. Even though both malnutrition and iron deficiency anemia are common in Africa, very few cases have been reported. Here, we describe the case of a young African woman diagnosed with PVS, which is a rare cause of dysphagia.
Clinical Presentation
History and Physical Examination
A 20-year-old young woman presented with progressive difficulty swallowing for one year. It was initially for solid meals, but for the past month, she has also had trouble with semisolid food. Associated with this, she had significant but unquantified weight loss and easy fatiguability of the same duration. She worked in Yemen when she left her job three months ago due to health issues, and she then moved back to Ethiopia.
She also had a history of blurring of vision, lightheadedness, vertigo and epigastric burning type of abdominal pain for one month. Due to the above complaints, she visited multiple nearby health facilities and was given unspecified oral medication but without significant improvement.
Otherwise, she did not complain of loss of appetite. There was no history of fever, nausea, vomiting, bowel habit change or stool color change. There was no history of ingestion of nonsteroidal anti-inflammatory drugs or any other drugs. The history of alkaline or acid ingestion was negative. There was no family or personal history of asthma, skin rash with itching, or runny nose. There was no family history of similar complaints. She had an irregular menstrual cycle that lasted for four to seven days.
Physical examination revealed normal vital signs except for tachycardia (PR=104 beats/minute). She had paper-white palpebral conjunctiva and palmar pallor. Otherwise, no abnormal physical findings were detected. There was no lymphadenopathy or glandular abnormalities. Auscultation of the heart revealed no murmurs. Examination of the abdomen revealed it to be soft and nontender with no organomegaly.
Laboratory Investigations
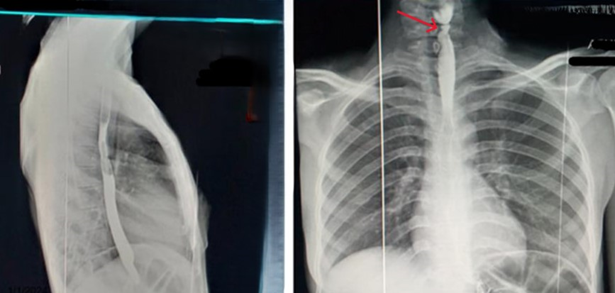
Her laboratory data revealed iron deficiency anemia with a hemoglobin level of 6.3 g/dl, mean cell volume (MCV) 61.4 FL, mean cell hemoglobin (MCH) 22 pg., mean corpuscular hemoglobin concentration (MCHC) 26.7 g/dl, red blood cell distribution width (RDW) 24.3. The serum ferritin concentration was 10.3 ng/dl. A peripheral smear revealed microcytic hypochromic cells. Radiological examination via barium swallow showed the presence of a cervical esophageal web (Figure 1). Upper endoscopy was desired, but it was not affordable.
Management and Outcome
Considering her presentation and investigation, a diagnosis of PVS was made at the local specialty clinic, and she was referred to Asella Teaching and Referral Hospital for blood transfusion. She was discharged after two cycles of cross-matched blood transfusion with 325 mg iron sulfate and TID and was scheduled for regular follow-up. Following iron therapy and transfusion, she achieved significant improvement in fatigue and dysphagia without endoscopic intervention.
Discussion
The most common causes of dysphagia, such as stricture, esophageal cancer, and motility disorders such as Achalasia, have been well studied. However, PVS is a rare cause of dysphagia and is worth considering in patients who present with symptoms of anemia and esophageal webs.
Dysphagia is usually painless and intermittent or progressive over several years, limited to solids and sometimes associated with weight loss. Patients can be asymptomatic until the luminal diameter at the esophageal web becomes less than 12 mm [5]. Over time, dysphagia can progress to involve liquids as well. Symptoms resulting from anemia, such as weakness, pallor, fatigue and tachycardia, may dominate the clinical picture, as in our case.
Esophageal webs and strictures can be detected via radiographic methods or endoscopy. The barium swallow test is the most sensitive test for diagnosing esophageal webs. During upper endoscopy, esophageal webs appear as smooth, thin, and gray lesions with an eccentric or central lumen and are most commonly located on the anterior wall of the esophagus. However, the web may be missed or accidentally ruptured during endoscopy [5,6].
Our patient is a young woman from a developing country where iron deficiency is common; thus, PVS was diagnosed based on iron deficiency anemia via laboratory testing and through the use of esophageal webs on barium esophorias (Figure 1). Upper endoscopy was planned to confirm the esophageal web and to rule out another differential diagnosis, but unfortunately, this was not performed.
The first step in the management of PVS is to identify the cause of iron deficiency [7]. This patient had no evidence of gastrointestinal (GI) bleeding, and the risk of GI malignancy was less likely in this age group. Her menses were irregular and lasted for 4-7 days but not massive enough to cause this degree of anemia. Thus, nutritional iron deficiency was considered a cause of anemia.
Plummer–Vinson syndrome can be treated easily and effectively with iron supplementation and mechanical dilation. Iron supplementation alone can resolve dysphagia in many patients [4]. However, in the case of significant obstruction of the esophageal lumen, rupture and dilation of the web should be performed [4,8]. This held true in our patient, in whom the symptoms improved after iron therapy. Dysphagia improvement after iron therapy strongly supports PVS rather than other possible causes of dysphagia, which is expected to persist.
The prognosis is very good, but due to the possibility of malignant transformation, regular follow-up is necessary. The most common cancer that develops in PVS patients is squamous cell carcinoma of the pharynx and esophagus [9]. Therefore, it is essential to recognize and treat esophageal webs as soon as possible and to replenish iron stores
Conclusion
Although Plummer-Vinson syndrome (PVS) is a rare condition, we should have high clinical suspicion in patients with dysphagia, IDA and post cricoid esophageal webs.
Declarations
Consent for Publication
Written informed consent was obtained from the patient for publication of her case reports.
Ethical Approval
The case report meets ethical guidelines and local legal requirements.
Conflict of Interest
No conflicts of interest
Funding Sources
This study did not receive any funding.
Author's Contributions
Zewudu Hurissa: Conceptualization, methodology, resources, review and editing. Mengesha Akale; Data curation, visualization, review and editing. Gezahgn Kefyalew: Writing original draft.
References
- Phatak S, Redkar N, Patil MA, Kuwar A. (2012). Plummer-Vinson Syndrome. BMJ Case Rep. Bcr2012006403.
Publisher | Google Scholor - Chhabra P, Khurana H. (2018). Image Diagnosis: Plummer-Vinson Syndrome: An Unusual Cause of Dysphagia. Perm J. 22:18-35.
Publisher | Google Scholor - Hefaiedh R, Boutreaa Y, Ouakaa-Kchaou A, Kochlef A, Elloumi H, et al. (2013). Plummer Vinson Syndrome Association with Coeliac Disease. Arab J Gastroenterol. 14(4):183-185.
Publisher | Google Scholor - Hoffmann RM, Jaffe PE. (1995). Plummer-Vinson Syndrome. A Case Report and Literature Review. Arch Intern Med. 155:2008-2111.
Publisher | Google Scholor - Karthikeyan P, Aswath N, Kumaresan R. (2017). Plummer Vinson Syndrome: A Rare Syndrome in Male with Review of The Literature. Case Rep Dent. 6205925.
Publisher | Google Scholor - Kundumadam, Shanker D.; Tama, Maher; Naffouj, Sandra; Kathi, Pradeep; Ehrinpreis, Murray N. (2018). Plummer Vinson Syndrome in A Young African American Female: A Rare Entity: 1776. American Journal of Gastroenterology. 113:S1013.
Publisher | Google Scholor - S. K. Swain, R. Panigrahy, M. C. Sahu, (2015). Plummer Vinson Syndrome in A Male and His Chromosomal Study-A Case Report, Egyptian Journal of Medical Human Genetics, 16(3):283-286.
Publisher | Google Scholor - Sreenivas DV, Kumar A, Mannar R, Babu GR. (2002). Results Of Savary-Gilliard Dilatation in The Management of Cervical Web of Esophagus. Hepato-Gastroenterology. 49:188-190.
Publisher | Google Scholor - Novacek G. (2006). Plummer-Vinson Syndrome. Orphanet J Rare Dis. 1:36.
Publisher | Google Scholor