Case report
Placenta Percreta with Bladder Invasion: Case Report
- Mariam Mahtate 1
- Aziz Slaoui 2*
- Soukaina Cherradi 1
- Najia Zeraidi 1
- Amina Lakhdar 1
- Aicha Kharbach 2
- Aziz Baydada 1
1Department of Gynecology-Obstetrics and Endoscopy, Maternity Souissi, University Hospital Center IBN SINA, University Mohammed V, Rabat, Morocco.
2Department of Gynecology-Obstetrics and Endocrinology, Maternity Souissi, University Hospital Center IBN SINA, University Mohammed V, Rabat, Morocco.
*Corresponding Author: Aziz Slaoui, Department of Gynecology-Obstetrics and Endocrinology, Maternity Souissi, University Hospital Center IBN SINA, University Mohammed V, Rabat, Morocco.
Citation: M Mahtate, A Slaoui, S Cherradi, N Zeraidi, A Lakhdar, A Kharbach, A Baydada. (2022). Placenta Percreta with Bladder Invasion: Case Report. International Journal of Medical Case Reports and Reviews, BRS Publishers. 2(1); DOI: 10.59657/2837-8172.brs.23.003
Copyright: © 2022 Aziz Slaoui, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: October 23, 2022 | Accepted: December 05, 2022 | Published: January 10, 2023
Abstract
Background: Placenta previa with bladder invasion is an uncommon and serious pathology, involving the maternal prognosis. However, as the rate of cesareans has increased, the disease has become more common.
Case presentation: We present the case of placenta previa percreta in 34 weeks of amenorrhea, gravida 2 para 1, with a history of a single caesarean section 5 years prior. Initially admitted for threat of premature delivery, we found a totally covering placenta previa with accretization sign and suspicion of bladder invasion. Abdomino pelvic MRI confirmed the diagnosis of placenta previa percreta. During monitoring, the patient presented an acute fetal distress requiring an emergency fetal extraction. She underwent a caesarean section for fetal rescue followed by a total hysterectomy requiring the removing of the anterior part of the bladder.
Conclusion: With a rising rate of cesarean sections, the risk of placenta accreta spectrum is increasing as well. Obstetricians and clinicians should be vigilant in prenatal diagnosis, especially if the risk factors are present. Multidisciplinary approach for preoperative, intraoperative and postoperative management can significantly improve maternal and fetal prognosis.
Keywords: placenta percreta; placenta accreta spectrum; total hysterectomy; bladder invasion
Introduction
Placenta percreta accounts for 7-10% of maternal deaths worldwide [1]. It is an uncommon pathology, that can lead to severe maternal morbidity or mortality if not diagnosed early. Placenta percreta is a specific subtype of placenta accreta spectrum. About 5% of cases of placenta accreta are percreta [2]. Compared to the other two subtypes, placenta accreta and placenta increta, placenta percreta shows villous invasion through the entire myometrium and possibly into surrounding structures, such as the bladder [3]. The cause is idiopathic but the most common risk factors are a previous history of cesarean section, placenta previa, grand multiparity, uterine curettage and Asherman syndrome [3].
We hereby describe an uncommon case of placenta percreta with invasion of the bladder wall. The surgery was performed in the context of emergency for fetal rescue. A total hysterectomy was performed that required the removing of a part of the bladder.
Case Presentation
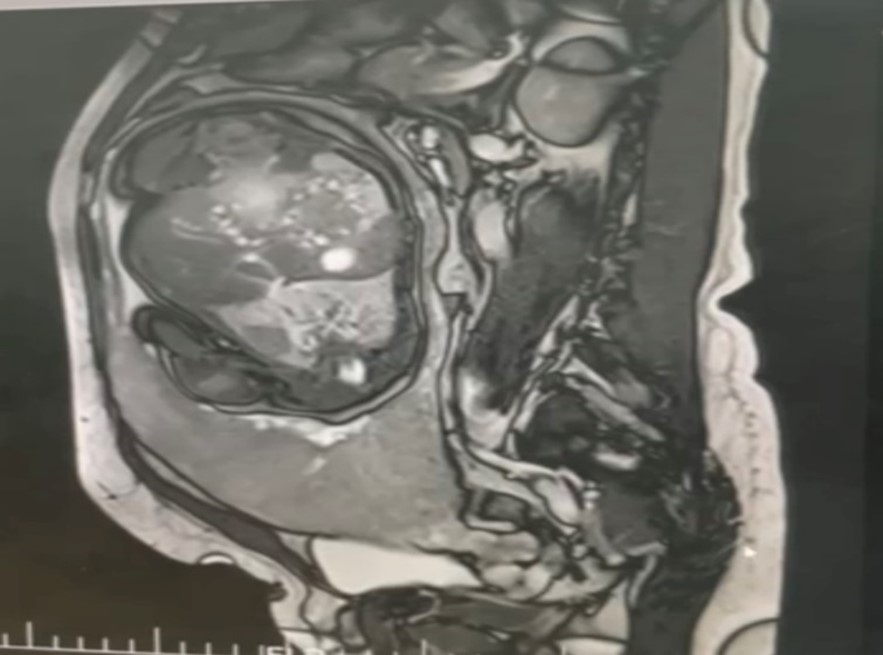
We herein report the case of a 37-year-old woman, gravida 2 para 1, with an obstetric history of cesarean section for acute fetal distress five years prior. She was initially admitted to our hospital in the context of threatened preterm labor with uterine contractions and minimal bleeding. Obstetric ultrasound showed an anterior low-lying placenta with signs of accretization and invasion of the posterior wall of the bladder. The patient was benefited from tocolytics to receive the fetal lung maturation by 12 mg of dexamethasone per day during 48 hours. Pelvic MRI done the next day confirmed placenta percreta with invasion into the muscularis of the posterior bladder wall (Figure 1).
Figure 1: Pelvic MRI sagittal image showing the placenta previa percreta with partial bladder invasion.
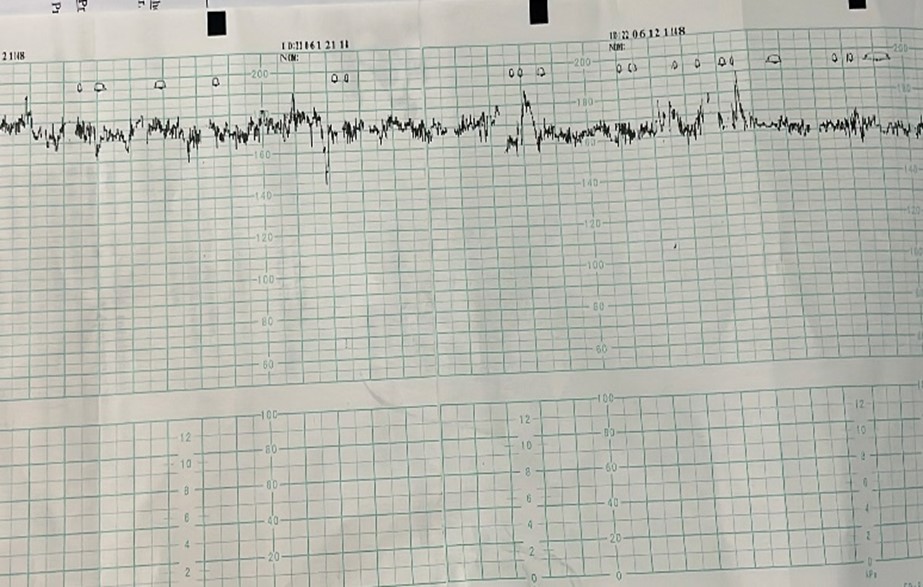
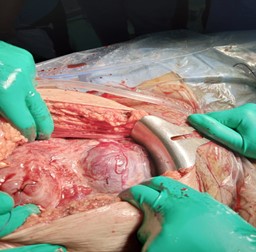
During monitoring, a moderate tachycardia of 180 beats/min was objectified on the fetal heart rate CTG (Figure 2). Emergency C-section was indicated for fetal rescue. She benefited from a spinal anesthesia and median laparotomy was performed (Figure 3).
Figure 2: Fetal heart rate CTG showing moderate tachycardia at 180 bpm rate.
Figure 3: Perioperative photography showing placental invasion of the bladder.
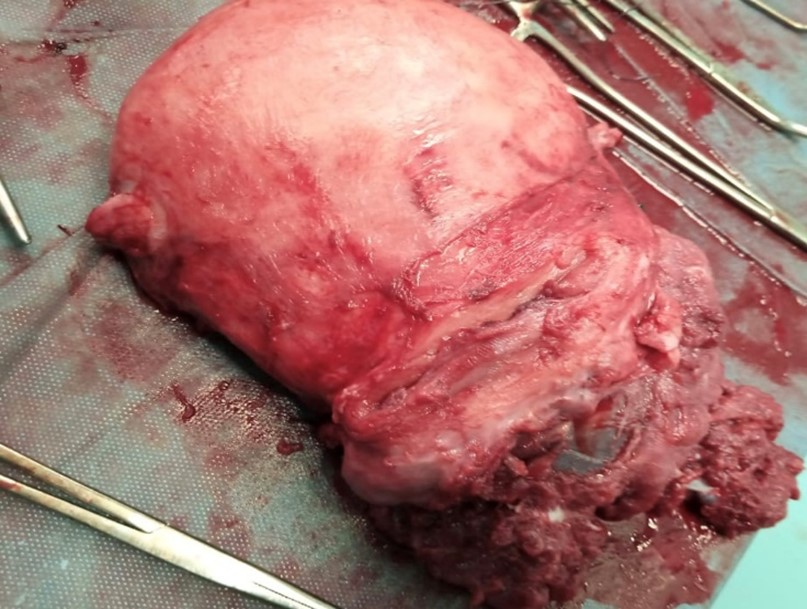
Anterior fundic incision (far from the implantation of the placenta) allowed us to extract the baby who had an Apgar score at 7/10/10 at respectively 1/5/10 minutes. Hysterorrhaphy was done without any attempt to separate the placenta. General anesthesia was then induced to allow better muscle relaxation and improve patient and surgeon comfort. Two large bore intravenous catheters and a radial arterial catheter were placed in anticipation of severe bleeding. Urologist medical team initially performed a partial cystectomy to separate the placenta. Then the gynecologic surgical team performed a total interadnexal hysterectomy with repair of the bladder (Figure 4). Blood loss was estimated at 1500 ml and the patient presented a moderate hemodynamic instability. A transfusion protocol was initiated and the patient received six units of PBRC and 2 units of FFP and allowed us to retrieve a stable hemodynamic state.
Postoperatively, she was transferred to the intensive care unit for monitoring. She was extubated the next day and discharged in the fifth day with her baby. Follow-up was uneventful.
Figure 4: Postoperative photography showing the inter adnexal total hysterectomy with partial cystectomy.
Discussion
Placenta accreta spectrum includes first accreta, in which the placenta is only adherent to the myometrium; then increta, in which the placenta invades the myometrium; and finally, percreta, when it penetrates the myometrium and attaches to other intra-abdominal organs. [4] The incidence of placenta percreta has increased from approximately 0.8/1000 deliveries in the 1980s to 3/1000 deliveries in the past decade [5]. Authors suggested that it is primarily due to an increase in the rate of cesarean delivery [6]. Other risk factors include low-lying placenta previa as well as history of placenta accreta, maternal age, multiparity, previous uterine surgery or curettage and Asherman's syndrome [7].
Placenta percreta may be asymptomatic or associated with symptoms of unusual pelvic pain, discomfort, distension, abdominal pain and hematuria in case of bladder invasion. Diagnosis is made in high-risk patients using ultrasonography and/or MRI [8]. Ultrasonography findings of accreta and percreta are loss of myometrial interface, retroplacental clear space, reduced myometrial thickness, turbulent placental lacunar flow, intraplacental lacunae and irregular bladder wall. Placental bulging or invasion into the bladder is also often seen. MRI is more accurate in diagnosing a posterior placenta, placenta percreta and for imaging morbidly obese patients [8]. Although our patient underwent a prenatal ultrasound examination showing an adherent low-lying placenta with suspicion of bladder invasion, it is the MRI that confirmed the diagnosis of placenta percreta.
Management strategy depends mainly on the anatomical type of placenta and the patient's desire for fertility. Placenta percreta is a situation with a high risk of hemorrhage, disseminated intravascular coagulation, surgical wounds of the bladder and ureters, multiple organ failure or even maternal death. Caesarean should be programmed in a level 3 maternity with well experienced practicians for this type of pathology [9]. Hysterectomy remains the most common surgical procedure in these cases [10]. Nowadays, conservative interventions are recommended before radical procedure in order to minimize surgical complications and preserve fertility. Conservative options include uterotonics drugs, external compression with uterine sutures (B-Lynch), intrauterine packing (Bakri balloon) and selective devascularization by ligation or embolization of the uterine artery [11]. Given the emergency context of our case and her wish not to have other children, we opted for a radical treatment.
Conclusion
With a rising rate of cesarean sections, the risk of placenta accreta spectrum is increasing as well. Obstetricians and clinicians should be vigilant in prenatal diagnosis, especially if the risk factors are present. Multidisciplinary approach for preoperative, intraoperative and postoperative management can significantly improve maternal and fetal prognosis.
This work has been reported in line with the SCARE 2020 criteria [12].
Abbreviations
MRI: Magnetic Resonance Imaging
CTG: Cardiotocography
Bpm: Beats per minute
PRBC: Packed Red Blood Cell
FFP: Fresh Frozen Plasma
Declarations
Guarantor of Submission
The corresponding author is the guarantor of submission.
Acknowledgements
None.
Funding
There are no funding sources to be declared.
Availability of data and materials
Supporting material is available if further analysis is needed.
Competing interests
The authors declare that they have no competing interests.
Author contribution
MM: study concept and design, data collection, data analysis and interpretation, writing the paper. AS: study concept and design, data collection, data analysis and interpretation, writing the paper. SC: study concept, data collection, data analysis, writing the paper. NZ: study design, data collection, data interpretation, writing the paper. AL: study concept, data collection, data analysis, writing the paper. AK: study concept, data collection, data analysis, writing the paper. AB: study concept, data collection, data analysis, writing the paper.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Ethics approval and consent to participate
Ethics approval has been obtained to proceed with the current study. Written informed consent was obtained from the patient for participation in this publication.
References
- Chandraharan E, Rao S, Belli AM, Arulkumaran S. (2012). The Triple-P procedure as a conservative surgical alternative to peripartum hysterectomy for placenta percreta. Int J Gynaecol Obstet. 117(2):191-194.
Publisher | Google Scholor - Anderson DJ, Liu H, Kumar D, Patel M, Kim S. (2021). Placenta Percreta Complications. Cureus. 13(10):e18842.
Publisher | Google Scholor - Tillu N, Savalia A, Patwardhan S, Patil B. (2019). Placenta percreta with bladder invasion: the armamentarium available in its management. Urol Ann. 11:324-327.
Publisher | Google Scholor - Wu S, Kocherginsky M, Hibbard JU. Abnormal placentation: twentyyear analysis. Am J Obstet Gynec.
Publisher | Google Scholor - K M Flood, S. Said, M. Geary, M. Robson, C. Fitzpatrick, F D Malone. (2009). Changing trends in peripartum hysterectomy over the last 4 decades, American Journal of Obstetrics and Gynecology, 200(6):632-636.
Publisher | Google Scholor - K A Fox, A Shamshirsaz, D. Carusi, et al. (2015). Conservative management of morbidly adherent placenta: expert review, ACOG. 213(6):755-760.
Publisher | Google Scholor - Wu S, Kocherginsky M, Hibbard JU. Abnormal placentation: twentyyear analysis. Am J Obstet Gynec.
Publisher | Google Scholor - Silvia Canonico, Maurizio Arduini, Giorgio Epicoco, Giuseppe Luzi, Saverio Arena, Graziano Clerici, Giuseppe Affronti. (2013). Placenta Previa Percreta: A Case Report of Successful Management via Conservative Surgery, Case Reports in Obstetrics and Gynecology.
Publisher | Google Scholor - Baughman WC, Corteville JE, Shah RR. (2008). Placenta accreta: spectrum of US and MR imaging findings. Radiographics. 28(7):1905-1916.
Publisher | Google Scholor - H. A. Mousa and Z. Alfirevic. (2002). Major postpartum hemorrhage: survey of maternity units in the United Kingdom, Acta Obstetricia et Gynecologica Scandinavica, 81(8):727-730.
Publisher | Google Scholor - Konijeti R, Rajfer J, Askari A. (2009). Placenta percreta and the urologist. Rev Urol. 11:173-176.
Publisher | Google Scholor - Agha R.A, Franchi T, Sohrabi C, Mathew G, for the SCARE Group. (2020). The SCARE 2020 guideline: updating consensus Surgical CAse REport (SCARE) guidelines, Int J Surg. 84:226-230.
Publisher | Google Scholor