Research Article
Pattern of Clinical Profile and Outcome of Gillian Barre Syndrome in Sudanese Patients
- Mahmoud H.S. Daoud ID 1
- Mohmed Hussien Ahmed Mohmed ID 2*
- Mohamed KhalafAllah Saeed 3
- Ammar El Tahir Mohamed Ahmed 4
- Khalid Mohammed Ali 5
- Abubakr Elmotesim Abdulla Elamin 6
- Abdalrahman Abdalmagid 7
1Department of Medicine, Facultyof Medicine, University of Gezira, Sudan.
2Faculty of Medicine, University of Gezira, Sudan.
3Faculty of Medicine, University of Science and Technology, Sudan.
4Department of Medicine, Faculty of Medicine, University of Khartoum, Sudan.
5Faculty of medicine, University of Gadarif,Sudan.
6Department of Medicine, Faculty of Medicine, University of Gezira, Sudan.
7Alsalam University, Aldamer Teaching Hospital, Aldamer, Sudan.
*Corresponding Author: Mohmed Hussien Ahmed Mohmed, Faculty of Medicine, University of Gezira, Sudan.
Citation: M. H. D. Salih, M. H. A. Mohmed, M.K.A. Saeed, A. T. M. Ahmed, Khalid M Ali. et al. (2024). Pattern of Clinical Profile and Outcome of Gillian Barre Syndrome in Sudanese Patients, Journal of BioMed Research and Reports, BioRes Scientia Publishers. 4(1):1-6. DOI: 10.59657/2837-4681.brs.24.059
Copyright: © 2024 Mohmed Hussien Ahmed Mohmed, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: November 21, 2023 | Accepted: December 13, 2023 | Published: January 08, 2024
Abstract
Introduction: Guillian Barre'-Syndrome (GBS) is an acute, autoimmune disease affecting spinal roots and peripheral nerves, characterized by a rapidly progressive, ascending weakness of the extremity, trunk and even respiratory and facial muscles and with minor sensory and autonomic dysfunction. As in Sudan there is no enough data regarding the pattern of presentation and outcome of GBS, our research aimed to study clinical profile, electrophysiological variant, and outcome of Sudanese patients diagnosed with (GBS).
Methods: A multi centers cross-sectional hospital-based study conducted in Khartoum from March to September 2020, 62 patients enrolled in the study, structured questionnaire consists of personal data, clinical history, examination findings, electrophysiological study result, management and outcome is used to assess the clinical profile and outcome of the disease.
Results: The study revealed that males and females are equally represented, 70% patients are between 18 years and 50 years. The onset of the weakness was less than or equal 3 days in 33.9% of patients, from 4 to 7 days in 41.9%, from 8 to 14 days in 11.3% and above 14 days in 12.9%.40.3% patients had Evidence of autonomic dysfunction. The majority of patients presented with weakness that started in the lower limbs (93.5%), in (4.8%) the weakness started in the upper limbs and then descend. In (1.6%) the weakness started in the pharyngeal and respiratory muscles from the start. Sensory complains were observed in 54 patients (87.1%), 3 patients (4.8%) developed urinary bladder incontinence and 36 patients (58.1%) had back pain at the onset of the disease. On clinical examination; (98.4%) of patients had absent reflexes, (35.5%) had bilateral facial nerve palsy and (4.8%) had unilateral facial nerve pals. Based on the electrophysiological studies, (37.09 %) were recorded as acute motor axonal neuropathy (AMAN), (29.03%) as acute inflammatory demyelinating poly neuropathy (AIDP) and (29.03%) as acute motor-sensory axonal neuropathy (AMSAN). Regarding the outcome, 30 patients (48.4%) fully recovered, 25 patients (40.3%) recovered with motor deficit, and 7 patients (11.3%) unfortunately died.
Conclusion: This study concluded that Guillian Barre'-Syndrome (GBS) in Sudanese population mainly affects age group from 18 to 50 years with variable maximum onset of weakness, presentation and outcome. Lower limb weakness and absent reflexes were the most presenting features. NCS showed axonal type of GBS found to be in nearly 66% of patients and 40% showed clinical evidence of dysautonomia.
Keywords: guillian barre'-syndrome; variants; outcome and sudanese patients
Introduction
Guillian Barre'-Syndrome (GBS) is an acute, autoimmune disease affecting spinal roots and peripheral nerves, characterized by a rapidly progressive, ascending weakness of the extremity, trunk and even respiratory and facial muscles and with minor sensory and autonomic dysfunction [1]. It affects .8-1.9 cases per 100,000 people per year [2], can occur in any age with bimodal distribution in age specific curve, peaks in young adults and the elderly [3] and Males appear to be affected more commonly [4], however, most of these studies were done in Europe and North America. In most of the cases rapidly progressive weakness is key presenting features, with nadir can be reached within 4 weeks and limb weakness appear to be commonest manifestation with proximal affection more than distal. Facial palsy represents most of cranial nerve involvement, followed by bulbar weakness, ophthalmoplegia, and tongue weakness. In about half the cases the illness is associated by sensory symptoms [5].
Nerve conduction study NCS is useful confirmatory diagnostic tool, also to differentiate between demyelinating and axonal subtypes of GBS [6], along with albumin cytological dissociation in cerebrospinal fluid [3]; however, GBS is clinical diagnosis. Acute inflammatory demyelinating polyneuropathy AIDP, acute motor and sensory axonal neuropathy AMSAN and acute motor axonal neuropathy AMAN are the commonest subtypes and tow aforementioned subtypes characterized by immune attack directed at axons rather than Schwann cells and myelin [7, 8].
Several randomized controlled trials studying the effect of immunotherapy in GBS have been done in the past few decades. Intravenous immunoglobulins IVIG and plasma exchange have proved effective [9]. Nevertheless, GBS is still a life-threatening disorder, patients can die in the acute progressive stage, most probably because of ventilator insufficiency or pulmonary complications, or from autonomic dysfunction including arrhythmia [10]. And Patients who survive frequently have residual complaints and deficits, which can have a substantial effect on daily activities and quality of life [11]. As in Sudan data regarding pattern of presentation, electro-physiologic subtype and outcome in GBS are scared, therefore this research aimed to study clinical profile and electrophysiological variants of Sudanese patients diagnosed with (GBS).
Methods
A descriptive cross-sectional study involving multi-Sudanese centers in Ibrahim Malik Hospital ICU, the National Center for Neurosurgery and Neurosciences (NCSN), Soba University Hospital and Omdurman teaching hospital. These are the major hospitals in Sudan receiving neurology patients from Khartoum and all Sudan states. Also, these health facilities provide clinical and electrophysiology services and ICUs. This study conducted from March to September 2020, 62 patients was enrolled in this study, and structured questionnaire consisted of personal data, clinical history, examination findings, management and outcome of the disease. And Nerve conduction study (NCS) was performed using standard procedure, and reported by expert neurologists and electrophysiologists.
Results
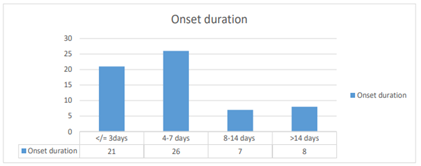
In a total of 62 patients with Guillian Barre'-Syndrome, there were 32 (51.6%) males and 30 (48.4%) females with male to female ratio of (1.07: 0.93). 20 patients (32.3%) were between 18 and 30 years, 23 patients (37.1%) were between 31 and 50 years, 15 patients (24.2.2%) were between 51 and 65 years and 4 patients (6.5%) were above 65 years. The majority of patients presented with weakness that started in the lower limbs (93.5%), in (4.8%) the weakness started in the upper limbs and then descend. In (1.6%) the weakness started in the pharyngeal and respiratory muscles from the start. Onset of the weakness was less than or equal 3 days in (33.9%) of patients, from 4 to 7 days in (41.9%), from 8 to 14 days in (11.3%) and above 14 days in (12.9%) (Figure 1). On clinical examination; (98.4%) of patients had absent reflexes, (35.5%) had bilateral facial nerve palsy and (4.8%) had unilateral facial nerve palsy.
Distal paresthesia, pins or sensory complains preceding the weakness were observed in 54 patients (87.1%), 3 patients (4.8%) developed urinary bladder incontinence and 36 patients (58.1%) had back pain at the onset of the disease. Regarding the autonomic dysfunction, 4 patients (6.5%) had minimum heart rate at rest (abnormal <50>110) and 25 patients (40.3%) had liable blood pressure. Overall, 25 patients (40.3%) developed clinical evidence of autonomic dysfunction. Based on the electrophysiology, (40.32%) were classified as acute motor axonal neuropathy (AMAN), (30.65%) as acute inflammatory demyelinating poly neuropathy (AIDP) and (29.03%) as acute motor-sensory axonal neuropathy (AMSAN). Regarding treatment, (87.1%) received intra venous immune globulin, (3.2%) underwent plasma exchange, and (1.6%) received both of them while (8.1%) didn’t receive any treatment. Near half of the patients (43.5%) were admitted to the ICU. Regarding the outcome; 30 patients (48.4%) fully recovered, 25 patients (40.3%) recovered with motor deficit, and 7 patients (11.3%) died.
Figure 1: Onset Duration
Table 1: Clinical presentations of the disease
| Presentations | Frequency | Percentage |
| Weakness | 62 | 100% |
| Distal paresthesia/pins/or sensory complication | 54 | 87.1% |
| Back painat onset | 36 | 58.1% |
| urinary bladder incontinence | 3 | 4.8% |
| Evidence of autonomic dysfunction | 25 | 40.3% |
Table 2: Disease variants basedon electrophysiological study
| Clinical variants based on electrophysiological study | Frequency | percentage |
| AMAN | 25 | 39.51% |
| AMSAN | 18 | 29.03% |
| AIDP | 19 | 31.45% |
Discussion
GBS occurs throughout the world, it affects .8-1.9 cases per 100,000 people per year. Our results showed that there were no differences in incidence distribution between male and female, this may be due to the type of study and the number of cases, these results are similar to studies conducted in India [12, 13]. Study conducted in USA showed that males are more likely to be affected than female. GBS has been reported in all age groups from infancy to elderly with bimodal age distribution [14]; however, it is more frequently affected adults and older people. In this study, people who are 50 years and less are more commonly affected, finding similar to results from previous studies [12, 13]. The most frequent symptom at the onset of the disease was limb weakness, mainly due to inflammation of the nerves which lead to muscle weakness. The weakness starts in the feet and then ascends to involve the upper body and limb [4]. Focal conduction block at the level of the lumbar and cervical nerve roots, rather than along the length of the nerve fiber can easily explained this [6]. No obvious differences in the pattern of classical muscle weakness were noted in this study.
Respiratory failure is dangerous consequences in GBS due to Weakness of respiratory and bulbar muscles as progressive weakness of both inspiratory and the expiratory muscles is the mechanism leading to respiratory failure in patient with GBS [15]. In this study few patients developed respiratory or bulbar muscle weakness, findings are less to another studies [15, 16]. Distal paresthesia is common in GBS. The study showed that about 87% of patients experienced distal paresthesia. This result supported by another study concluded that more than half of GBS patients developed paresthesia of distal extremities [17]. Autonomic dysfunctions in GBS are high and reported to affect (65%) of patients with mild GBS and may reach up to (90%) in moderate to severe GBS [18] and autonomic disturbance is reported to occur in (40%) of patients with GBS in this study with abnormal heart rate and labile blood pressure appear to be the most frequent manifestations. The frequency of autonomic dysfunction is low in our study because we did not use any of validated autonomic testing to document autonomic dysfunction, we just depended on reviewing the records of pulse and blood pressure monitoring.
Reduced or absent deep tendon reflexes is of particular importance to diagnose GBS, this may reflect desynchronization or dispersion of impulses carried by myelinated fibers in the afferent arm of the reflex arc. Our study showed that approximately all patients have reduced or absent deep tendon reflexes at the time they are first examined. Several studies support this result [12, 17]. Facial nerve is the most commonly affected cranial nerve in GBS affecting around half of the cases and typically occurs when there is substantial limb weakness. It is often bilateral (35.5%), but occasionally asymmetrical and rarely unilateral (4.8%). GBS variants vary in frequency, severity and from region to region. This study revealed that AMAN was still the commonest subtype accounted for 37.09% followed by AIDP and AMSAN (29.03% for each). Study from north china showed that AMAN was the commonest subtype there. On the other hand, AIDP subtype was found to be dominated in Europe and United States [19, 20].
GBS is still a life-threatening disorder, patients can die in the acute progressive stage and patients who survive frequently have residual complaints and deficits [10, 11]. In this study 48.4%fully recovered, 40.3% recovered with motor deficit, and 11.3% died, in contrary to study conducted in Nepal in which 90% of cases showed good functional outcome and 6.45% died [21]. The increase in mortality number in our study partially encountered due to limited resources like ICU beds and the high cost of IVIG and plasma exchange.
Conclusion
This study concluded that Guillian Barre'-Syndrome (GBS) in Sudanese population affects age group from 18 to 50 years with variable maximum onset of weakness, presentation and outcome. Lower limb weakness and absent reflexes were the most presenting features. NCS showed axonal type of GBS found to be in nearly 66% of patients and 40% showed clinical evidence of dysautonomia.
Declarations
Ethical considerations
Ethical clearance was obtained from committee of SMSB (Sudan Medical Specialization Board). Acceptance of hospitals administrations on approval was obtained. Written informed consent from patients was obtained before participation.
Conflict of interest
The authors declare no conflict of interest
References
- Hughes RAC, Cornblath DR. (2023). Guillain-Barré syndrome. The Lancet, 366(9497):1653-1666.
Publisher | Google Scholor - Willison HJ, Jacobs BC, van Doorn PA. (2016). Guillain-Barré syndrome. The Lancet. Lancet Publishing Group, (318):717-727.
Publisher | Google Scholor - Yuki N, Hartung HP. (2023). Guillain–Barré Syndrome. New England Journal of Medicine, 366(24):2294-2304.
Publisher | Google Scholor - Beghi E, Kurland LT, Mulder DW, Wiederholt WC. (2023). Guillain-Barré Syndrome: Clinicoepidemiologic Features and Effect of Influenza Vaccine. Arch Neurol, 42(11):1053-1057.
Publisher | Google Scholor - Fokke C, Van Den Berg B, Drenthen J, Walgaard C, Van Doorn PA, Jacobs BC. (2014). Diagnosis of Guillain- Barré syndrome and validation of Brighton criteria. Brain. 2014;137(1):33-43.
Publisher | Google Scholor - Hadden RDM, Cornblath DR, Hughes RAC, Zielasek J, Hartung HP, Toyka K V., et al. (1998). Electrophysiological classification of guillain-barré syndrome: Clinical associations and outcome. Ann Neurol, 44(5):780-788.
Publisher | Google Scholor - McKhann GM, Cornblath DR, Griffin JW, Ho TW, Li CY, Jiang Z, et al. (1993). Acute motor axonal neuropathy: A frequent cause of acute flaccid paralysis in China. Ann Neurol, 33(4):333-342.
Publisher | Google Scholor - Griffin JW, Li CY, Ho TW, Tian M, Gao CY, Xue P, et al. (1996). Pathology of the motor-sensory axonal Guillain-Barré syndrome. Ann Neurol [Internet]. 1996 Jan 1 [cited 2023 Nov 30];39(1):17-28.
Publisher | Google Scholor - Hughes RAC, Swan A V., Raphaël JC, Annane D, Van Koningsveld R, et al. (2007). Immunotherapy for Guillain-Barré syndrome: A systematic review. Brain, 130: 2245-2257.
Publisher | Google Scholor - Van Den Berg B, Walgaard C, Drenthen J, Fokke C, Jacobs BC, Van Doorn PA. (2014). Guillain–Barré syndrome: pathogenesis, diagnosis, treatment and prognosis. Nature Reviews Neurology, 10(8):469-482.
Publisher | Google Scholor - Desforges JF, Ropper AH. (2010). The Guillain–Barré Syndrome. 326(17):1130-1136.
Publisher | Google Scholor - Sudulagunta SR, Sodalagunta MB, Sepehrar M, Khorram H, Bangalore Raja SK, et al. (2015). Guillain-Barré syndrome: clinical profile and management. GMS German Medical Science, 13.
Publisher | Google Scholor - Dhadke S, Dhadke V, Bangar S, Korade MB. (2013). Clinical profile of Guillain Barre syndrome. Journal of Association of Physicians of India.
Publisher | Google Scholor - McGrogan A, Madle GC, Seaman HE, De Vries CS. (2009). The epidemiology of Guillain-Barré syndrome worldwide: A systematic literature review. Neuroepidemiology, 32:150-163.
Publisher | Google Scholor - Orlikowski D, Prigent H, Sharshar T, Lofaso F, Raphael JC. (2004). Respiratory Dysfunction in Guillain- Barré Syndrome.
Publisher | Google Scholor - Hahn AF. (2001). The Challenge of Respiratory Dysfunction in Guillain-Barré Syndrome. Arch Neurol, 58(6):871-872.
Publisher | Google Scholor - Piccione EA, Salame K, Katirji B. (2014). Guillain-barré syndrome and related disorders. Neuromuscular Disorders in Clinical Practice, 9781461465676:573-603.
Publisher | Google Scholor - Samadi M, Kazemi B, Oskoui SG, Barzegar M. (2013). Assessment of Autonomic Dysfunction in Childhood Guillain-Barré Syndrome. J Cardiovasc Thorac Res, 5(3):81.
Publisher | Google Scholor - Tian J, Cao C, Li T, Zhang K, Li P, Liu Y, et al. (2023). Electrophysiological Subtypes and Prognostic Factors of Guillain-Barre Syndrome in Northern China. Front Neurol, 714.
Publisher | Google Scholor - Ho TW, Mishu B, Li CY, Gao CY, Cornblath DR, Griffin JW, et al. (2023). Guillain-Barré syndrome in northern China Relationship to Campylobacter jejuni infection and anti-glycolipid antibodies. Brain, 118(3):597-605.
Publisher | Google Scholor - Bhagat SK, Sidhant S, Bhatta M, Ghimire A, Shah B. (2023). Clinical Profile, Functional Outcome, and Mortality of Guillain-Barre Syndrome: A Five-Year Tertiary Care Experience from Nepal. Neurol Res Int.
Publisher | Google Scholor