Research Article
Patient Care of STEMI In Algeria: The STAMI Study
- M.A. Bouraghda 1*
- M.A. Bouzid 2
- K. Boussouf 3
- B. Kichou 4
- A. Rouati 5
- N. Hammoudi 6
- D. Nibouche 7
- M. Chettibi 2
1Blida University Hospital, Algeria.
2Béjaïa University Hospital Center, Algeria.
3CHU Saadna Abdenour, Algeria.
4CHU Nedir Mohamed, Algeria.
5CHU Ibn Badis, Algeria.
6CHU Maouche Mohand Amokrane, Algeria.
7CHU Issad Hassani, Algiers university hospital, Algeria.
*Corresponding Author: M.A. Bouraghda, Blida University Hospital, Algeria.
Citation: Bouraghda M. A., Bouzid M. A., Nibouche D., Boussouf K., Kichou B. (2024). Patient Care of STEMI In Algeria: The STAMI Study, Journal of Clinical Cardiology and Cardiology Research, BioRes Scientia Publishers. 3(1), 1-7. DOI: 10.59657/2837-4673.brs.24.028
Copyright: © 2024 M.A. Bouraghda, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: March 21, 2024 | Accepted: April 22, 2024 | Published: April 30, 2024
Abstract
Background: ST-segment elevation myocardial infarction (STEMI) is associated with a significant short- and medium-term mortality rate despite progress at several levels of intervention worldwide. Few data are available in Algeria.
Objectives: To evaluate major cardiovascular events in STEMI patients in Algeria, during hospitalization, 1 month and 12 months after discharge.
Materials and Methods: STAMI (STEMI: Algerian national registry) is a descriptive, non-interventional, national, multicenter, prospective registry-based study that was conducted in Algerian university public hospitals and included adults hospitalized within 24 hours of STEMI symptoms’ onset. Major in-hospital cardiovascular events and after hospital discharge were recorded at 1 and 12 months.
Results: Between November 2016 and January 2017, 329 patients were enrolled; 322(97.9%) patients constituted the full-analysis set. Median age was 61[53; 68] years, 79.5% were males, their median body mass index was 26.0[23.4; 28.4] kg/m². Most of them presented with a Killip class I. The first 2 main risk factors were smoking (46.6%) and high blood pressure (40.1%). Median time between symptoms’ onset and arrival to the emergency room was 240 minutes and median time between symptoms’ onset and primary angioplasty was 330 minutes. Fibrinolysis was administered to 194 (60.2%) patients and primary angioplasty to 94 (29.2%) patients. During hospitalization, 7 (2.2%) patients had a bleeding, 3(0.9%) patients had a recurrent MI, 3 (0.9%) patients a stroke and overall, 12 (3.7%) patients experienced at least 1 major cardiovascular event. In-hospital death rate was 2.2%. At 1 month and 12 months, major cardiovascular events rates were: death 2.3% and 6.2%; MI 0.3% and 0.4%, and stroke 1.0% and 0.4%, respectively.
Conclusion: Coronary emergencies remain a major public health issue in Algeria; more effective strategies aimed at the prevention of cardiovascular disease need to be implemented in Algeria to reduce the delays in access to hospital and minimize morbidity and mortality.
Keywords: ST-segment elevation myocardial infarction (STEMI); Algeria; Registry; Outcomes; Mortality
Introduction
In 2017, the Global Burden of Diseases, Injuries, and Risk Factors Study, estimated that the cardiovascular diseases (CVD) were responsible for the largest number of deaths within non-communicable diseases (17·8 million; 95% uncertainty interval [UI]: 17·5–18·0 deaths). On a global level, between 2007 and 2017, deaths from ischemic heart disease increased from 7.30 million (95% UI: 7·22–7·46) to 8.93 million (95% UI: 8·79–9·14) [1]. According to the World Health Organization (WHO), at least three-quarters of the world's deaths from CVDs occur in low- and middle-income countries. People living in low- and middle-income countries often do not have the benefit of primary health care programs for early detection and treatment of people with risk factors for CVDs [2]. According to the Algerian Society of Cardiology, CVD, including myocardial infarction (MI), kill almost twice as many people as all cancers combined. In 2019, ischemic heart disease was regarded as responsible for 127 deaths per 100,000 population in Algeria [3].
Acute ST-segment elevation myocardial infarction (ST-elevation myocardial infarction (STEMI) is defined as a separate entity among acute coronary syndromes due to its to its own pathophysiological, prognostic and therapeutic characteristics [4]. Overall, 30% to 50% of patients die within one month after MI, half of them by cardiac death suffered during the first two hours after the onset of symptoms. In contrast to the pre-hospital prognosis, early mortality in the hospital phase over the last 40 years has been reduced to 6-8.4% thanks to the creation of specialized units for revascularization treatments and secondary prophylactic drug treatments [5]. Factors of poor prognosis are age, high heart rate, diabetes, history of MI, coronary artery bypass grafting, Killip class at admission and previous location of necrosis [6]. The objectives of the STAMI study were to evaluate major cardiovascular events in STEMI patients in Algeria. Secondary objectives included evaluation of time to patient’s care, hospitalization and mortality at 1 and 12 months.
Materials and Methods
Study Design
STAMI (ST elevation acute myocardial infarction: Algerian national registry) is a descriptive, non-interventional, national, multicenter, prospective and longitudinal registry-based study conducted among cardiologists in university hospitals, from the public sector in Algeria.
Patient’s Selection
Females and males ≥18 years diagnosed with ST-segment elevation myocardial infarction (STEMI), defined by a history of chest pain/discomfort and persistent ST-segment elevation (> 30 min) of ≥ 0.1 mV in 2 or more contiguous leads on electrocardiogram (ECG) or presumed new left bundle branch block (LBBB) upon admission, were eligible to participate if they signed the informed consent and completed the Contact Order Form. They also had to be hospitalized within 24 hours of current episode symptoms onset. Patients were not eligible to participate if STEMI was precipitated by or as a complication of surgery, trauma or gastrointestinal bleeding or post-percutaneous coronary intervention (PCI) or occurred in patients already hospitalized for other reasons. Additional exclusion criteria were any condition which could significantly limit the complete follow-up of the patient (e.g., tourist, does not understand the local language), and presence of serious/severe co-morbidities which may limit short-term (i.e., 12 months) life expectancy.
Data Collection
During the hospitalization period, socio-demographics, medical history, patient care, evolution and hospital discharge, and treatment patterns of eligible patients were collected in an electronic case report form (eCRF). During the follow-up, data on medical procedures/hospitalizations, and living status were recorded over the phone at one and 12 months. Site’s characteristics were also recorded. Patients underwent clinical assessments and received the standard medical care as determined by the treating physician. Patients did not receive any experimental intervention or treatment as a consequence of their participation in STAMI.
Ethical Considerations
Collection of data started only after the obtention of the patient’s written informed consent and data were analyzed respecting their autonomy and anonymity. The study was conducted in accordance with the Declaration of Helsinki, the Good Clinical Practice guidelines, and the applicable local legislations on non-interventional studies.
Statistical Analysis
The primary endpoint was the percentage of major cardiovascular events (mortality, recurrence of MI and stroke). A total of 300 patients were to be recruited from the participating sites in order to have an acceptable precision.
Mean ± Standard Deviation (SD) or median and interquartile ranges [IQR] for non-normal distributions are displayed. Missing data were reported but not included in the analyses. The full-analysis set (FAS) was defined as all enrolled patients with no major protocol deviation and the follow-up population (FUP) as all FAS patients discharged from hospital. Data are summarized using standard descriptive statistics. All statistical tests are two-sided and are displayed with their bilateral 95% confidence interval (95%CI). Cumulative mortality rate after discharge was estimated using the Kaplan-Meier method with its 95% CI at 30 days and 12 months. Statistical analysis was done using SAS/STAT software, version 14.3 for Windows.
Results
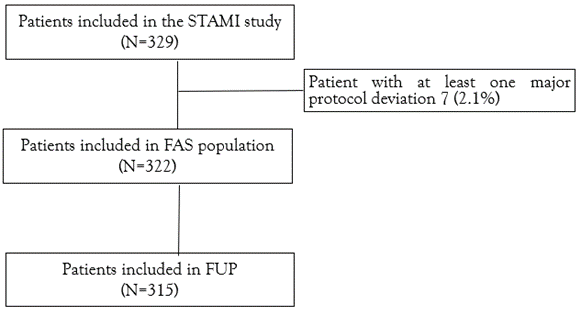
Overall, 329 patients were enrolled between November 2016 and January 2017, of whom 322 (97.9%) patients constituted the FAS. The 315 (95.8%) patients who were discharged from the hospital constituted the FUP (Figure 1); 310 (98.4%) patients had at least one follow-up phone call (Figure 1).
Figure 1: Patient's disposition.
FAS: Full Analysis Set (patients with no major protocol deviation); FUP: Follow-up population (patients included in FAS population, not dead during hospitalization, and discharged)
Baseline Characteristics, Initial Presentation, And Early Management
Patient’s characteristics are displayed in Table 1. Patients were mostly male with a median age of 61 [53; 68] years old and a median body mass index (BMI) of 26.0 [23.4; 28.4] kg/m2. Most patients presented with a Killip class I.
Table 1: Patient's characteristics upon admission (FAS population).
| Overall n=322 | |
| Males | 256 (79.5%) |
| Age (years) | 61 [53; 68] |
| BMI (kg/m²) | 26 [23.4; 28.4] |
| Heart rate (beat/min) | 80 [70; 97] |
| SBP (mmHg) | 130 [120; 150] |
| DBP (mmHg) | 80 [70; 90] |
| Killip class I II III IV | 299 (92.9%) 13 (4.0%) 9 (2.8%) 1 (0.3%) |
n (%) patients or median [Q1; Q3]. BMI: body mass index; DBP: diastolic blood pressure; SBP: systolic blood pressure.
Patient’s risk factors are presented in Table 2.
Table 2: Patient's risk factors (FAS population).
| Overall n=322 | |
| Smoking | 150 (46.6%) |
| Hypertension | 129 (40.1%) |
| Dyslipidemia | 38 (11.8%) |
| Family history of coronary heart disease | 33 (10.2%) |
| Diabetes Type 1 Type 2 | 1 (0.3%) 108 (33.5%) |
| Unstable angina | 25 (7.8%) |
| Renal failure | 19 (5.9%) |
n (%) patients
Initial patient management is presented Table 3. Median time between symptoms’ onset and arrival to the emergency room was 240 [120; 420] minutes; 191 (59.3%) patients had previously been in another medical facility. At arrival, an ECG was performed for all patients. ST+ elevation show that ischemia affected the anterior area for 181 (56.2%) patients, the inferior area for 130 (40.4%) patients, the basal area for 49 (15.2%) and the lateral area for 52 (16.1%) patients. Arrhythmia was present in 27 (8.4%) patients including: ventricular tachycardia in 7 (25.9%) patients, ventricular fibrillation in 6 (22.2%) patients and atrial fibrillation in 9 (33.3%) patients. Overall, 22 (6.8%) patients presented conduction defects with mostly 3rd degree atrioventricular block [12 (54.5%) patients] or right bundle branch block [7 (31.8%) patients].
Table 3: Initial presentation and management (FAS population).
| Overall n=322 | |
| Time delays (minutes) | |
| Time between symptoms’ onset and arrival to the emergency room | 240 [120; 420] |
| Time between symptoms’ onset and primary angioplasty | 330 [189; 600] |
| Procedures upon arrival | |
| ECG (at inclusion) | 322 (100%) |
| ECG (90 min) | 306 (95.0%) |
| Primary angioplasty | 94 (29.2%) |
| Fibrinolysis: | 194 (60.2%) |
| Tenecteplase | 154 (81.9%) |
| Alteplase | 34 (18.1%) |
| Medications | |
| Unfractionated Heparin | 41 (13.6%) |
| LMWH | 261 (86.4%) |
| Aspirin | 321 (99.7%) |
| Beta-blockers | 202 (62.7%) |
| Clopidogrel | 308 (97.2%) |
| Ticagrelor | 9 (2.8%) |
| Diuretic | 21 (6.5%) |
| Statin | 200 (62.1%) |
| Nitrates | 30 (9.3%) |
| Morphine | 48 (14.9%) |
| ACE inhibitor | 200 (62.1%) |
| Others | 60 (18.6%) |
median [Q1; Q3] or n (%) patients. ACE: angiotensin-converting enzyme; ECG: electrocardiogram; LMWH: Low Molecular Weight Heparin.
In-Hospital Complications
The median duration of hospitalization was 4 [3; 6] days. During hospitalization, a control angiography was performed in 129 (40.1%) patients. Recurrent MI occurred in 3 (0.9%) patients (95%CI: [0.0%; 2.0%]) and 17 (5.3%) experienced recurrent chest pain. Emergency revascularization by angioplasty was performed in 65 (20.2%) patients. A stroke occurred in 3 (0.9%) patients [0.0%; 2.0%]. Overall, 12 (3.7%) patients experienced at least 1 major cardiovascular event during hospitalization (3.7% [1.7%; 5.8]). In-hospital death rate was 2.2% [0.6%; 3.8%]; in the 7 patients who died (1 stroke and 7 cardiac deaths), median time to death was 2 [1; 5] days.
Discharge
Overall, 315 patients were discharged. Treatments prescribed at discharge are displayed in Table 4.
Table 4: Medications at discharge.
| Overall n=315 | |
| Aspirin | 311 (98.7%) |
| Clopidogrel | 296 (94.9%) |
| Ticagrelor | 16 (5.1%) |
| Oral Anticoagulant | 21 (6.7%) |
| Statin | 308 (97.8%) |
| Beta-blockers | 295 (93.7%) |
| ACE inhibitor | 291 (92.4%) |
| Oral Antidiabetics | 46 (14.6%) |
| Insulin | 41 (13.0%) |
n (%) patients. ACE: angiotensin-converting enzyme.
Follow-up
The follow-up by phone was effective in 307 (97.5%) and 271 (86.0%) patients, at 1 and 12 months respectively. Cardiovascular events reported during the follow-up are presented Table 5. Mortality rate was 2.3% [0.6%; 3.9%] at 30 days and 6.2% [3.4%; 9.0%] at 12 months.
Table 5: Follow-up.
| 1 month n=307 | Between 1- and 12-months n=271 | |
| Myocardial infarction | 1 (0.3%) | 1 (0.4%) |
| New hospitalization for a cardiac event | 16 (5.2%) | 29 (10.7%) |
| Stroke | 3 (1.0%) | 1 (0.4%) |
| Hemorrhage | 3 (1.0%) | 0 |
n (% column) patients.
Discussion
The STAMI study was the first national registry describing patient management of acute MI and risk assessment after MI in Algeria. Patient’s characteristics were similar to the STEMI patients from the French FAST-MI 2015 study in term of age (61 [53; 68] years vs 63 ± 14 years), sex (79 % vs 75 % males) and risk factors (smoking: 47% vs 42%; hypertension: 40% vs 45%) [7]. Previous registry studies conducted in the Middle East and North Africa (MENA) region reported a higher prevalence of cardiovascular risk factors especially tobacco which was recorded in 58% to 65 % in STEMI patients [8-10]. Indeed, a recent estimation by the WHO, indicated that prevalence of smoking in Algeria is decreasing [11], most likely as a result from the national preventive measures. One main difference between the STAMI patients and the FAST-MI 2015 patients was the percentage of Killip class I: in STAMI, most patients (93%) present a Killip class I when the FAST-MI 2015 proportion was slightly lower (88%). This suggests that the most serious cases of STEMI died before arrival at the hospital or were not able to give their informed consent.
The 240-minute median time between symptoms’ onset and arrival to the emergency room was high whereas in another study performed in the MENA median was 178 minutes [12]. The median time between symptoms’ onset and primary angioplasty was 330 minutes when the ESC guidelines recommend to initiate primary angioplasty within 120 minutes of STEMI diagnosis [13]. These differences may be due to variations in clinical management, but also to socioeconomic factors such as the type of hospital, and delays to presentation and treatment [10]. For hospitals with no available percutaneous coronary intervention, transfers remain the optimal strategy. For expected delays of greater than 120 minutes, a pharmaco-invasive strategy is recommended [14]. To minimize patient delay, guidelines recommend increasing public awareness of how to recognize common symptoms [13]. Indeed, in the STAMI study, more than half patients consulted in another facility before arriving to the emergency room.
The main objective of the STAMI study was to estimate the incidence of major cardiovascular events. In-hospital bleeding and stroke were higher than the respectively reported <1>1. In-hospital mortality of unselected patients with STEMI in the national registries of the European Society of Cardiology countries, varies between 4 and 12% [13]. In a similar STAMI setting, a Tunisian study reported a higher in-hospital mortality in STEMI patients of 7.0 % [9].
The rates of major cardiovascular events at 1 month were lower in the STAMI study than in a large Indian study: death (2.3% vs 8.6%), reinfarction (0.3% vs 2.3%) and stroke (1.0% vs 0.7%) [15].
In the present study the acute reperfusion rate was high (fibrinolysis 60.2% and primary angioplasty 29.2%) compared to other developing countries. A prospective analysis of registry data of acute coronary syndromes in India, the CREATE registry, reported a high rate of reperfusion with fibrinolytic therapy for patients with STEMI (59%) but a very low rate of in-hospital percutaneous coronary intervention (PCI) (8.0%) [15]. In comparison with a similar study performed in Maghreb, only 30% of STEMI patients received a fibrinolytic therapy, and PCI was performed in 27% of STEMI patients, of whom 97% received a stent [10]. Additionally, the FAST-MI Tunisia registry (2014-2015) recorded a total rate of reperfusion of 61.8% of STEMI patients: 30% with primary PCI and 31.8% with intravenous fibrinolysis, total reperfusion rate is still lower than the one reported in the present study [16].
More effective strategies aimed at the prevention of cardiovascular disease need to be implemented in Algeria to reduce the delays in access to hospital and minimize morbidity and mortality. Also, a longer door-to-balloon delay in primary PCI for STEMI is related to higher risk of adverse outcomes [17].
This observational study is subject to limitations and biases, as all observational studies, such as potential selection bias and missing or incomplete information. As with most registries, hospital and patient enrolments were voluntary; thus, the study results may not be representative of patients in all hospitals in the country.
Conclusion
Coronary emergencies remain a major public health issue in Algeria during which saving time is a real challenge. The more systematic use of primary angioplasty and adjuvant therapies to angioplasty has allowed an improvement of the prognosis of infarction. Early diagnosis in the hospital setting makes it possible to offer appropriate therapeutic management.
Declarations
Patient Consent and Ethical Approval
This study was approved by the Algerian Ministry of Health and a central ethical committee on October 06, 2016. All patients provided written informed consent before any collection of study data, and data were analyzed respecting their autonomy and anonymity. The study was conducted in accordance with the Declaration of Helsinki, the Good Clinical Practice guidelines and all the applicable local legislations on non-interventional studies.
Acknowledgements
The authors would like to thank the investigators, the study staff as well as the patients for their participation.
Funding Information
This work was supported by the Algerian society of Cardiology (SAC) who was involved in each of the following tasks: study design, collection, analysis, and interpretation of data, writing of the article.
Competing Interests
All authors have no conflict of interest to declare.
Author Contribution
All authors read, revised, and approved the final version of the article.
References
- Roth GA, Abate D, Abate KH, et al. (2018). Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980–2017: a systematic analysis for the Global Burden of Disease Study 2017. The Lancet. 392:1736–88.
Publisher | Google Scholor - (2021). cardiovascular diseases (CVDs).
Publisher | Google Scholor - (2021). Global health estimates: Leading causes of death.
Publisher | Google Scholor - Hanssen M, Cottin Y, Khalife K, et al. (2012). French Registry on Acute ST-elevation and non ST-elevation Myocardial Infarction 2010. FAST-MI 2010. Heart. 98:699–705.
Publisher | Google Scholor - Goldberg RJ, Samad NA, Yarzebski J, et al. (1999). Temporal trends in cardiogenic shock complicating acute myocardial infarction. N Engl J Med 340:1162–8.
Publisher | Google Scholor - Hasdai D, Califf RM, Thompson TD, et al. (2000). Predictors of cardiogenic shock after thrombolytic therapy for acute myocardial infarction. J Am Coll Cardiol 35:136–43.
Publisher | Google Scholor - Belle L, Cayla G, Cottin Y, et al. (2017). French Registry on Acute ST-elevation and non-ST-elevation Myocardial Infarction 2015 (FAST-MI 2015). Design and baseline data. Arch Cardiovasc Dis. 110:366–78.
Publisher | Google Scholor - Alhabib KF, Gamra H, Almahmeed W, et al. (2020). Acute myocardial infarction and acute heart failure in the Middle East and North Africa: Study design and pilot phase study results from the PEACE MENA registry. PLoS One. 15:e0236292.
Publisher | Google Scholor - Addad F, Gouider J, Boughzela E, et al. (2015). [Management of patients treated for acute ST-elevation myocardial infarction in Tunisia: Preliminary results of FAST-MI Tunisia Registry from Tunisian Society of Cardiology and Cardiovascular Surgery]. Ann Cardiol Angeiol (Paris). 64:439–45.
Publisher | Google Scholor - Moustaghfir A, Haddak M, Mechmeche R. (2012). Management of acute coronary syndromes in Maghreb countries: The ACCESS (ACute Coronary Events – a multinational Survey of current management Strategies) registry. Archives of Cardiovascular Diseases. 105:566–77.
Publisher | Google Scholor - (2021). Tabagisme et covid-19.
Publisher | Google Scholor - Alhabib KF, Sulaiman K, Al-Motarreb A, et al. (2012). Baseline characteristics, management practices, and long-term outcomes of Middle Eastern patients in the Second Gulf Registry of Acute Coronary Events (Gulf RACE-2). Ann Saudi Med. 32:9–18.
Publisher | Google Scholor - Ibanez B, James S, Agewall S, et al. (2017). ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). European Heart Journal. 39:119–77.
Publisher | Google Scholor - Larson DM, McKavanagh P, Henry TD, et al. (2016). Reperfusion Options for ST Elevation Myocardial Infarction Patients with Expected Delays to Percutaneous Coronary Intervention. Interv Cardiol Clin. 5:439–50.
Publisher | Google Scholor - Xavier D, Pais P, Devereaux PJ, et al. (2008). Treatment and outcomes of acute coronary syndromes in India (CREATE): a prospective analysis of registry data. Lancet. 371:1435–42.
Publisher | Google Scholor - Addad F, Mahdhaoui A, Gouider J, et al. (2019). Management of patients with acute ST-elevation myocardial infarction: Results of the FAST-MI Tunisia Registry. PLOS ONE. 14:e0207979.
Publisher | Google Scholor - Foo CY, Bonsu KO, Nallamothu BK, et al. (2018). Coronary intervention door-to-balloon time and outcomes in ST-elevation myocardial infarction: a meta-analysis. Heart. 104:1362–9.
Publisher | Google Scholor