Research Article
Pancytopenia as Another Collateral Damage of Covid-19 Infection in a Previously Healthy Child
- Binita Poudel
- Manidipa Barman
- Sarthak Chakrabarti
- Vinod Kumar *
Department of Paediatrics, All India Institute of Medical Sciences, Rishikesh, Uttarakhand, India.
*Corresponding Author: Vinod Kumar, Department of Paediatrics, All India Institute of Medical Sciences, Rishikesh, Uttarakhand, India.
Citation: Poudel B., Barman M., Chakrabarti S., Kumar V. (2023). Pancytopenia as Another Collateral Damage of COVID-19 Infection in A Previously Healthy Child-A Case Report. Clinical Case Reports and Studies, BRS Publishers. 2(5); DOI: 10.59657/2837-2565.brs.23.044
Copyright: © 2023 Vinod Kumar, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: June 02, 2023 | Accepted: June 19, 2023 | Published: June 23, 2023
Abstract
Aim and Background: Pancytopenia is a reduction of all the three cells of peripheral blood lineage: leukocytes, erythrocytes and platelets. The bone marrow can be primarily hypocellular in pancytopenia either due to reduction of hematopoietic cell production or ineffective haemopoiesis. Generally, infections, toxins or malignant transformation of the marrow are responsible for most of the cases of pancytopenia.1 After the incidence of Covid-19 pandemic, pancytopenia has been seen to occur as a rare complication secondary to SARS-COV 2. Here, we report a unique case of pancytopenia in a previously healthy child with SARS-CoV-2 infection.
Keywords: anaemia; COVID-19, infections; pancytopenia
Introduction
The new coronavirus was first reported in Wuhan, China, in December 2019 [2]. The virus was called SARS-CoV-2 and causes a disease called COVID-19 (a form of severe pneumonia). COVID 19 pandemic has led to a lot of repercussions for the entire medical world. COVID 19 mainly causes mild disease in children with fever and involvement of the lower respiratory tract as the common clinical characteristics in children [3]. Common laboratory abnormalities include increased inflammatory markers (C-reactive protein CRP, procalcitonin, ferritin) and deranged coagulation parameters (increased d-dimer, increased fibrinogen). Lymphopenia and eosinopenia are the common cell-lines abnormalities found. Increased interleukin-6 (IL-6) and elevated markers of cardiac injury like creatine kinase-MB (CK-MB) and lactate dehydrogenase (LDH) are also common [4]. Pancytopenia is a rare complication of COVID 19 and usually not seen in the previously healthy individual. Usual causes of pancytopenia in children are inherited bone marrow failure syndrome (IBMFS), malignancy, infection, drugs and megaloblastic anaemia (nutritional vitamin B 12 deficiency). Pancytopenia associated with COVID-19- can be self-limiting and does not necessarily need bone marrow biopsy [5].
Method
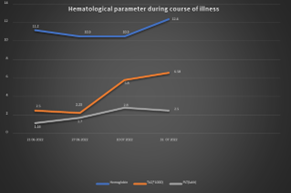
An 11 years old, male child, with normal birth history, pre-morbidly healthy, presented with the chief complaint of fever for 15 days. Fever was acute in onset, high grade, not associated with chills and rigors, with the maximum recordable temperature to be 104. There was no diurnal variation of the fever episodes, and the episodes got relieved with oral anti-pyrectics. There were no symptoms of cough, running nose, rashes, joint pain, sore throat, fast breathing, loose stool, burning micturition, cyanosis, bleeding manifestations, recent travel history, or animal exposure associated with the illness. On examination, child had pallor and was afebrile at admission. There was no lymphadenopathy, tachypnoea, or organomegaly on physical examination. Initial laboratory workup revealed pancytopenia with a haemoglobin (Hb) of 11.2 gm/dl (range: 11.5-14.5 g/dl), total leucocyte count (TLC) of 2500 cells/mm3 (range: 4,000-11,000 cells/cu mm), absolute neutrophil count of 1125 cells/mm3 (normal: ≥1500 cells/mm3), and platelet count of 1.16 lac/microliter (range: 1.5-4.5 lac/microliter) (Figure 1). Peripheral blood smear showed normocytic normochromic, with a reticulocyte count of 0.25% (normal: 0.5-2.5%). Renal function tests (RFT) and liver function tests (LFT) were within normal limits. His inflammatory markers were raised with a C‐reactive protein of 7.5 mg/L (normal: ≤5 mg/L), ferritin of 658 ng/ml (normal: 12-300 ng/ml), and a Lactate Dehydrogenase (LDH) of 850 IU/L (normal: 105-333 IU/l). Serum triglycerides were within normal limits. He was evaluated for the possible causes of pancytopenia which included leukaemia, myelodysplastic syndrome, megaloblastic anaemia, and infections. For the evaluation of focus of fever, serological tests for dengue and enteric fever, immunochromatographic test (ICT) for malaria, and urine examination for pus cells and culture sensitivity were done, which were all inconclusive. As child had a history of fever for more than 14 days, tuberculosis (TB) workup (chest x-ray, tuberculin skin testing and CBNAAT) were done, which came to be normal. Peripheral blood smear (PBS) examination showed normocytic normochromic anaemia with moderate anisocytosis without the presence of any macro-ovalocytes or hyper-segmented neutrophils. There was no evidence of haemolysis, sepsis, or atypia. No history of weight loss, bleeding manifestations, weakness, lymphadenopathy, or organomegaly ruled out malig-nancy for all practical purpose.
Probability of post COVID-19 pancytopenia was made in view of prolonged history of high-grade fever without any other particular focus of infection. SARS CoV2 IgG antibody was sent for the same which came out to be elevated (2976 AU/ml, ≥13 AU/ml is considered positive). HRCT thorax was not done due to absence of any respiratory symptoms. Regular and periodic monitoring of the cell lines were done (viz. Hb, TLC, ANC and platelet counts). Child’s haematology parameters improved over the next 96 hours without the need of any specific therapy. At his most recent OPD visits, all his cell-line parameters have returned to the baseline values.
Figure 1: Line Diagram Showing Haematological Parameter.
Discussion
Clinical presentation of the COVID 19 is variable, including asymptomatic infection, mild upper respiratory infection with non-specific symptoms like diarrhoea, sore-throat, etc, and severe pneumonia and respiratory failure [6]. Some studies have shown that it also has effect on the haematopoietic system and haemostasis also. COVID 19 associated haematological abnormalities are lymphopenia, thrombocytopenia, leukopenia and hypercoagulability [7]. Lymphopenia is the most common overall [7].
There are very few case reports on SARS-CoV2-induced pancytopenia [8]. Neither the CONFIDENCE study nor the study done by Lu et al. reported to have cases with pancytopenia [3, 9]. Pancytopenia in children is due to nutritional deficiencies, megaloblastic anaemia, infection, malignancies, radiation therapy, chemo-therapy drug-induced bone marrow toxicity, and immunosuppressive medications [10]. Issa et al reported the first case of pancytopenia in a 53-year-old man with mantle cell lymphoma in complete remission following autologous bone marrow transplant (immune-compromised state) [8]. Adel et al reported the case of a COVID-19 induced pancytopenia in a 71-day old infant [11]. His initial laboratory testing revealed marked pancytopenia with low reticulocyte count (0.2%). The PBS showed no atypical cells. Bone marrow aspirate showed a hypocellular marrow without any abnormal cells. However, this case developed a secondary hemophagocytic lympho-histiocytosis (HLH) like picture and ultimately succumbed. Our case did not fit into the HLH criteria. Bone marrow was not done in our case due to short course of the illness on periodic monitoring.
Fritch et al reported three cases of severe aplastic anaemia with hypocellular bone-marrow, all with positive SARS COV2 antibody levels. Hence, COVID-19 is emerging as a plausible cause of acquired aplastic anaemia in the post-pandemic era.
COVID-19 can lead to a cytokine storm like picture due to hypercoagulable state and increased production of IL-6. This can present as a HLH like picture as shown by Tiwari et al in a case of b cell acute lymphoblastic leukaemia (B-cell ALL) which was ultimately diagnosed by PBS blasts of 8% and bone marrow picture of hemophagocytes admixed with blast cells. Initial diagnosis of Covid induced aplastic anaemia turned into a diagnosis of B-ALL due to persistence of pancytopenia like picture on PBS. However, there was no need to do bone marrow in our case due to self-limiting course of the disease and improvement of counts on follow up. Hence, an initial cytokine storm in COVID -19 can seldom mask the underlying illness and make the patient present with just a HLH like picture [12].
Covid-19-associated pancytopenia can be self-limiting and does not necessarily need bone marrow biopsy for confirmation as was shown by Hereby et al. in a case of follicular lymphoma [5]. The pancytopenia persisted only for the time the patient was symptomatic for the upper respiratory tract infection caused by SAR-COV2.
Conclusion
Pancytopenia is a rare complication of COVID-19 and is self-limiting in most immunocompetent individuals. Pancytopenia due to SARS COV-2 can occur due to transient myelosuppression occurring in the same way as induced by other common viral infections. A high index of suspicion should be kept to attribute pancytopenia in any child with mild upper respiratory tract infection like illness in the current era.
References
- Bhatnagar SK, Chandra J, Narayan S, Sharma S, Singh V et al. (2005). Pancytopenia in children: etiological profile. J Trop Pediatr., 51:236-239.
Publisher | Google Scholor - Zhonghua Liu Xing Bing Xue Za Zhi. (2000). Epidemiology Working Group for NCIP Epidemic Response, Chinese Center for Disease Control and Prevention. The epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19) in China, 41:145-151.
Publisher | Google Scholor - Parri N, Lenge M, Buonsenso D. (2020). Coronavirus Infection in Pediatric Emergency Departments (CONFIDENCE) Research Group. Children with Covid-19 in Pediatric Emergency Departments in Italy. N Engl J Med. 383:187-190.
Publisher | Google Scholor - Henry BM, Benoit SW, de Oliveira MHS, Hsieh WC, Benoit J, Ballout RA, et al. (2020). Laboratory abnormalities in children with mild and severe coronavirus disease 2019 (COVID-19): A pooled analysis and review. Clin Biochem., 81:1-8.
Publisher | Google Scholor - Hersby DS, Do TH, Gang AO, Nielsen TH. (2021). COVID-19-associated pancytopenia can be self-limiting and does not necessarily warrant bone marrow biopsy for the purposes of SARS-CoV-2 diagnostics. Ann Oncol.m 32:121-123.
Publisher | Google Scholor - Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. (2020). Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet, 395:497-506.
Publisher | Google Scholor - Terpos E, Ntanasis-Stathopoulos I, Elalamy I, Kastritis E, Sergentanis TN, et al. Hematological findings and complications of COVID-19. Am J Hematol., 95:834-847.
Publisher | Google Scholor - Issa N, Lacassin F, Camou F. (2020). First case of persistent pancytopenia associated with SARS-CoV-2 bone marrow infiltration in an immunocompromised patient. Ann Oncol 31:1418-1419.
Publisher | Google Scholor - Lu X, Zhang L, Du H, Zhang J, Li YY. et al. (2020). SARS-CoV-2 Infection in Children. N Engl J Med. 382:1663-1665.
Publisher | Google Scholor - Jain A, Naniwadekar M. An etiological reappraisal of pancytopenia - largest series reported to date from a single tertiary care teaching hospital. BMC Hematol.13:10.
Publisher | Google Scholor - Adel M, Magdy A. (2023). SARS-CoV-2 infection in an infant with non-respiratory manifestations: a case report. Egyptian Pediatric Association Gazette, 69:3.
Publisher | Google Scholor - Tiwari N, Krishnan NR, Singh S, Madan J, Nath D, Tripathi S, et al. (2023). COVID 19 and Pancytopenia: A Single Case Experience of a Pediatrics Institute. SJPM, 05:308-310.
Publisher | Google Scholor