Case Series
Ovarian Vein Embolisation for Pelvic Congestion Syndrome
- Amana Sharif 1*
- Andrew Simon 1
- Ratna Das 2
- Kunal Rathod 3
- Ahmed Tariq Saleh 4
- Mohamed Shariq 4
- Krishna Prasad Bellam Premnath 4
1ST 5 trainee in Obstetrics and Gynaecology.
2Specialist registrar obstetrics and gynaecology.
3Consultant Obstetrician and Gynaecologist.
4Consultant Radiologist Barking Havering and Redbridge university hospital NHS foundation trust, London.
*Corresponding Author: Amana Sharif, ST 5 trainee in Obstetrics and Gynaecology.
Citation: Sharif A, Simon A, Das R, Rathod K, Saleh A T, et, al. (2024). Ovarian Vein Embolisation for Pelvic Congestion Syndrome. Journal of Women Health Care and Gynecology, BioRes Scientia Publishers. 3(3):1-13. DOI: 10.59657/2993-0871.brs.24.035
Copyright: © 2024 Amana Sharif, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: January 24, 2024 | Accepted: February 17, 2024 | Published: February 29, 2024
Abstract
Pelvic Congestion Syndrome, also known as ovarian and pelvic vein reflux is a cause of chronic pelvic pain mainly affecting pre-menopausal, multiparous women. Chronic pelvic pain is defined as pain in the lower abdomen present for more than 6 months. The aetiology of PCS is not fully understood. Multiple factors, i.e., physiological changes in pregnancy, varicosities of the ovarian or pelvic veins due to valvular incompetence and anatomical variations can lead to this. During pregnancy the ovarian vein can be compressed by the enlarging womb or become dilated due to the increased blood flow. The diagnosis of PCS is confirmed by radiological imaging including ultrasound and CT of the pelvis as first line non-invasive methods. Ultrasound features include torturous and dilated para-uterine veins more than 4mm in diameter or ovarian veins greater than 5-6mm. Ovarian vein embolisation is an effective and safe treatment option for PCS, with a low risk for complications, which can significantly improve the quality of life for patients suffering from this chronic, debilitating condition.
Keywords: ovarian vein; embolisation; pelvic congestion syndrome
Introduction
Pelvic Congestion Syndrome (PCS), also known as ovarian and pelvic vein reflux [1] is a cause of chronic pelvic pain mainly affecting pre-menopausal, multiparous women [2]. Chronic pelvic pain (CPP) is defined as pain in the lower abdomen present for more than 6 months. The aetiology of PCS is not fully understood. Multiple factors, i.e., physiological changes in pregnancy, varicosities of the ovarian or pelvic veins due to valvular incompetence and anatomical variations can lead to this. During pregnancy the ovarian vein can be compressed by the enlarging womb or become dilated due to the increased blood flow. This is thought to affect the valves in the vein causing them to stop working and allowing the blood to flow backwards, contributing to the development of PCS. Nutcracker syndrome describes the compression of the left renal vein between the aorta posteriorly and superior mesenteric artery anteriorly. Diagnostic symptoms include loin pain, pelvic varices, haematuria and proteinuria [3].
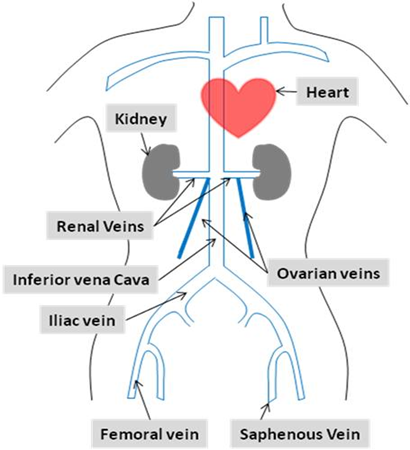
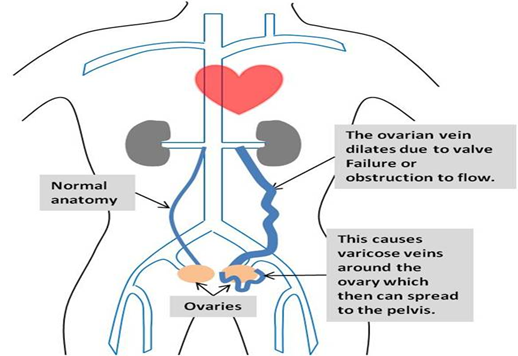
Diagram 1: Normal pelvic venous anatomy [4].
Diagram 2:Illustration of the vein dilatation and the formation of varicose veins around the ovary due to insufficiency of the valves. Blood flows in the wrong direction, causing pooling in the veins and causing them to enlarge [4]. Patients can present with a variety of signs and symptoms, for example, chronic pelvic or perineal pain, pelvic heaviness, deep dyspareunia, and varicosities affecting the vulva, perineum or lower limbs [1].
Diagnosis of PCS
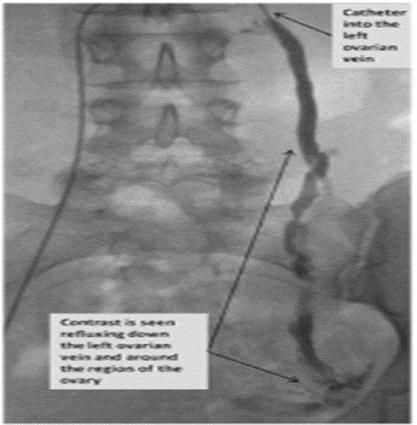
PCS should be considered by clinical history of the above symptoms and on examination if visible varicose veins are found. Ultrasound examination (US) may also prove useful, using sound waves to detect the abnormal veins. It is effective at showing the blood flow through the veins and is non-invasive. However, sometimes the veins in the pelvis are difficult to see through the abdomen. The diagnosis may require further investigation through non-invasive imaging modalities, such as, magnetic resonance imaging (MRI) and computed tomography (CT). This allows visualisation of the location of varicose veins to enable appropriate planning of intervention. Pelvic venography is still used to diagnose PCS and assess the anatomy before treatment is considered. This can be done at the same time as ovarian vein/pelvic vein treatment (embolisation) or as a separate procedure. A catheter is placed in the ovarian and pelvic veins, contrast is then injected, and the images seen on the fluoroscopic machine give a picture of the anatomy.
Treatment for PCS
Medical drug treatments, include medroxyprogesterone acetate and more recently, goserelin, have been shown to be effective in approximately 75% of women in reducing pain and the size of the varicose veins. Medroxyprogesterone acetate is a progestin and goserelin a gonadaotropin-relasing hormone agonist (GnRH agonist). However, the usual treatment is percutaneous transcatheter pelvic vein embolisation. This is a minimally invasive treatment that is safe and can be done as a day-case. Other treatment options are open or laparoscopic surgery to ligate the culprit veins. Both these procedures are more invasive than ovarian vein embolisation and require a general anaesthetic and a longer recovery period.
Pelvic Vein Embolisation
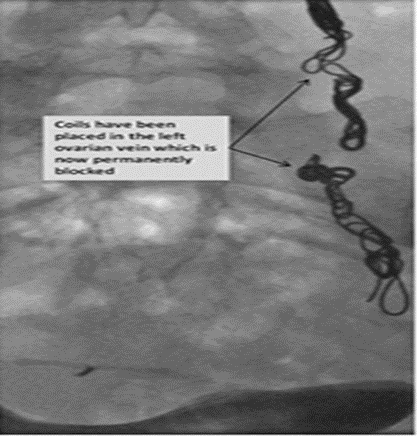
Pelvic vein embolisation is a minimally invasive procedure performed transcutaneously under the guidance of interventional radiology. Venous catherisation is performed either via the femoral or the internal jugular veins. Proximal to the dilated veins the catheter deploys metal coils with the aim of blocking the vein. Alternatively, sclerosing agents such as glue or foam can be infiltrated locally via the intravenous catheter at the desired site.
Figure 1a: The catheter is seen within the left ovarian vein. Contrast (X-ray dye) is seen refluxing down the left ovarian vein [4, 5].
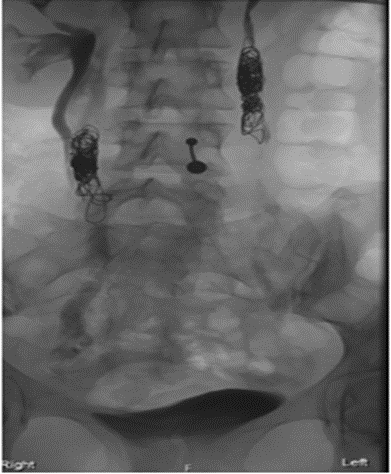
Figure 1b: The left ovarian vein has been successfully embolised (permanently blocked) with coils [4,5].
Case Series
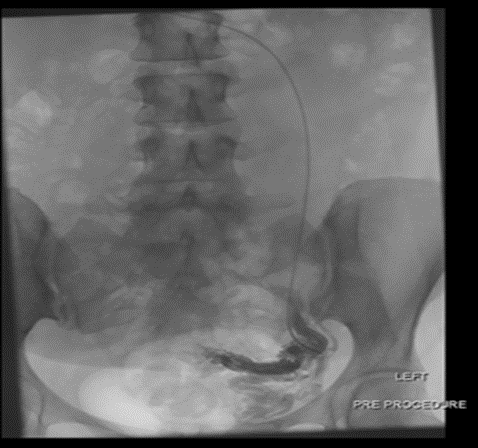
Case 1
A 38-year-old woman, P3 with three normal deliveries. Her main presenting symptoms were menorrhagia, irregular uterine bleeding, and chronic pelvic pain for the past 2 years. Pain was constant in nature, with heaviness and constant swelling in the lower abdomen. She sub-optimally managed her pain with simple NSAIDs, i.e. paracetamol and ibuprofen. Her quality of life was significantly impacted to the extent that she stopped exercising, missed work, and avoided social events. She had an ultrasound pelvis and CT pelvis scan, which was unremarkable. She was otherwise medically fit and well and had laparoscopic sterilisation in the past, and a diagnostic laparoscopy for pelvic pain, along with mirena coil insertion to regulate her periods. Diagnostic laparoscopy was unremarkable, although a degree of congested dilated pelvic veins was seen. She underwent CT Venogram of pelvic veins which showed mild para-uterine varices. Ovarian vein embolisation was performed using multiple coils in October 2021. Within the first two weeks she started getting relief from heaviness, and now she reports complete resolution of her symptoms and a significant improvement in her quality of life.
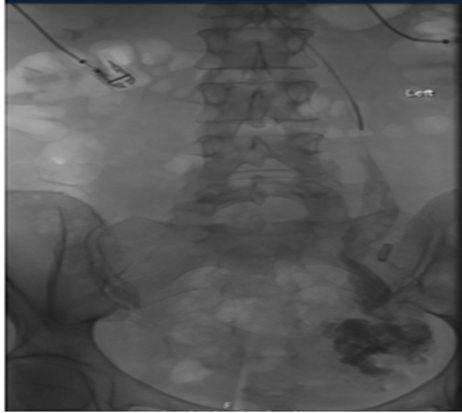
Figure 2a: Via the right internal jugular vein, a catheter and a Terumo soft wire were passed to reach the left ovarian vein. Accumulation of the contrast shows the dilated left ovarian vein.
Figure 2b: This image shows the deployment of multiple Nester (2 x 12mm, 6 x 10 mm, 4 x 8 mm, 1 x 6 mm), ensuring the left ovarian vein totally thrombosed.
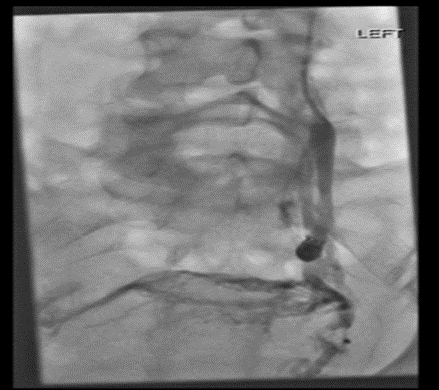
Case 2
A 41-year-old woman, P4 with two normal deliveries and two previous caesarean sections, with no significant past medical history. She presented with a 2-year history of pelvic, lower back and hip pain, which were constant throughout her menstrual cycle, but worsened during menses. The pain was sharp and stabbing in nature, 4/10 in severity. Associated symptom of increased urinary frequency. Her symptoms did not affect her quality of life and taking paracetamol on an as required basis did help to alleviate the pain. A transvaginal ultrasound pelvis and a CT pelvis with contrast revealed: ‘bilateral engorgement of the gonadal veins and mild-moderate venous varicosity noted bilaterally, predominantly on the left side around the left adnexa and uterus. Both gonadal veins draining into the renal veins. No engorgement of vessels noted extending deep into the vaginal wall. Both iliac veins and inferior vena cava appear normal in calibre. No evidence of thrombosis. An ovarian vein embolisation was performed. Ultrasound-guided right internal jugular vein access was taken. The left ovarian vein was cannulated and a venogram was performed, which revealed a dilated left ovarian vein with stagnation of contrast and reversal of flow. There was no reflux into the pelvic veins or to the contralateral side. Left ovarian vein embolization was done using 3% Fibrovein foam as sclerosant and 12mm coils with an occlusion balloon catheter. Left internal iliac venogram was also done with the balloon occlusion catheter, which did not show any significant varices or reflux of contrast into collateral veins. Post-procedure she felt considerably better, with a significant improvement in her pain, also a marked reduction in her urinary frequency. A Mirena coil was inserted in August 2023.
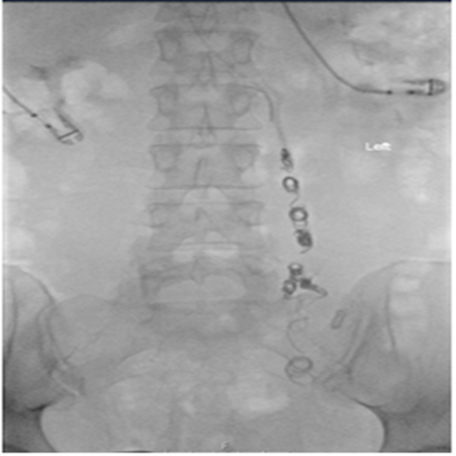
Figure 3a: Under US guidance the right internal jugular vein was entered, and he left ovarian vein cannulated. The venogram shows dilated left ovarian vein.
Figure 3b: Left ovarian vein embolisation was done using 3% fibrovein foam as sclerosant and 12 mm coils with an occlusion balloon catheter.
Case 3
A 58-year-old woman, P3 with 3 normal vaginal deliveries, described a 10-year history of pain in her left iliac fossa, lower back, and left leg. It was a dragging sensation in her perineum that was constant throughout her cycle. She was “miserable and felt very depressed and isolated,” because of a lack of a definitive diagnosis. She was unable to stand up for long periods and found that co-codamol provided no relief. CT pelvis was performed in July 2017, which showed: ‘minor para-uterine vessel distension with 6mm left ovarian vessels.’ Transvaginal pelvis in April 2018 revealed: ‘tortuous congested parametrial vessels up to 6mm diameter, especially on the left side; indicative of pelvic congestion.’ She underwent ovarian vein embolisation in May 2019. The venogram demonstrated an ectatic, incompetent left ovarian vein with a large network of para-uterine veins. Reflux to the contralateral internal iliac vein was alSo seen. 6 ml of sclerosant foam (Fibrovein 3%) was slowly injected. The majority of the para-uterine varicosities disappeared after a couple of minutes in the final venogram. On follow-up 1-month post-procedure, she reported some relief from the perineal aching and the sensation of dragging and heaviness; however, stated she still had pain in her left iliac fossa. Despite this, she did improve her physical activity, and started going on long walks.
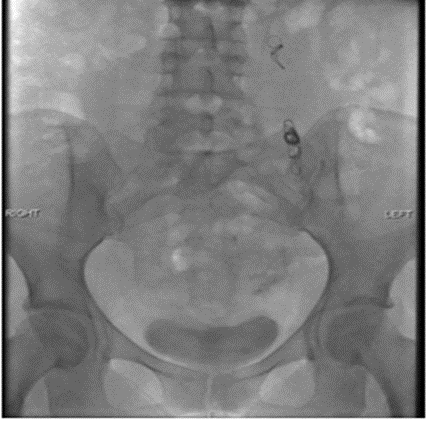
Figure 4a: The right femoral vein was entered for antegrade access and cannulation of the left ovarian vein was performed. The venogram hows an incompetetnt lt ovarian vein with large network of parauterine veins. Reflux to the contralateral internal iliac vein is seen.
Figure 4b: Sclerosant foam (Fibrovein 3%) was injected in to the ovarian vein. Subsequent to this the parauterine varicosities dissappeared at the end of the proceedure.
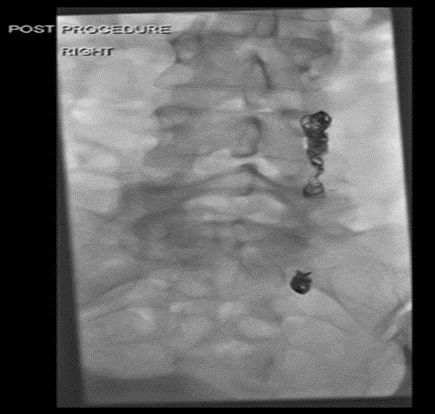
Case 4
A 43-year-old woman, P3 with three previous caesarean sections. Her presenting complaints were chronic pelvic pain, deep dyspareunia, and painful, varicose veins. These had been present since 2012, when she underwent a diagnostic laparoscopy and adhesiolysis. She was seen by vascular surgery, who noted varicosities in the peri-vulval region and buttock crease. US Doppler lower limb veins performed in September 2015 showed the left saphenous vein had a maximum diameter of 12mm and was incompetent. CT venogram and ovarian vein embolisation was performed in July 2016. A trans-brachial approach was used, and the left gonadal vein was cannulated. The venogram was performed which demonstrated significant left-sided ovarian varices. The right common femoral vein was cannulated, and the angioplasty balloon was sited within the left iliac vein and inflated. 3% fibrovein sclerosant was injected into the distal left ovarian vein with minor post injection extravasation seen, following which multiple coils were successively deployed within the mid-ovarian vein. On follow-up post-procedure there was no improvement in the symptoms of pain on standing and dyspareunia. Her pain had now increased to 4/10 in severity, for which she took co-codamol daily and naproxen during her menses.
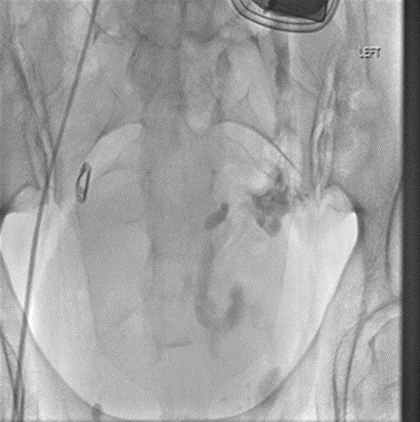
Figure 5a: A trans brachial approach was used and the left gonadal vein was cannulated and a venogram was performed which demonstrated significant left-sided ovarian varices.
Figure 5b: The right common femoral vein was cannulated and the angioplasty balloon was sited within the left iliac vein. The 3% Fibrovein sclerosant was injected into the distal left ovarian vein. Following which multiple coils were successively deployed within the mid ovarian vein.
Case 5
A 56-year-old woman, P3 with three normal vaginal deliveries presented with a 1-year history of left-sided abdominal pain, worse on standing and relieved by lying down. A severe pain which affected her quality of life as a teacher, preventing her from standing up too long. Associated symptoms of vulval pressure and soreness, for which she took paracetamol and ibuprofen. CT pelvis in June 2015 showed: ‘dilated tortuous para-uterine veins and dilated bilateral ovarian veins, measuring up to 7 mm in calibre, features in keeping with pelvic congestion syndrome.’ Ovarian vein embolisation was performed in January 2016. A right trans-jugular approach was taken. The left ovarian vein was cannulated with MPA 5F catheter. A venogram confirmed the reflux within the vein and multiple peri-ovarian and peri-uterine veins. Embolisation was performed with combination of coils and foam (Fibrovein 1%) using sandwich technique. Final venogram showed cessation of the reflux through the left ovarian vein. There was a significant improvement in her symptoms, with the abdominal and vulval pain dissipating. She would occasionally experience self-limiting, mild pain when standing for long periods, which would not require analgesia.
Figure 6a: A right transjugular approach was used and the left ovarain vein was cannulated and a venogram was performed which confirmed reflux within the vein and multiple peri-ovarian and peri-uterine veins.
Figure 6b: Embolisation was performed with combination of coils and 1% Fibrovein sclerosant foam using a sandwich technique. The Final venogram showed cessation of the reflx through the left ovarian vein.
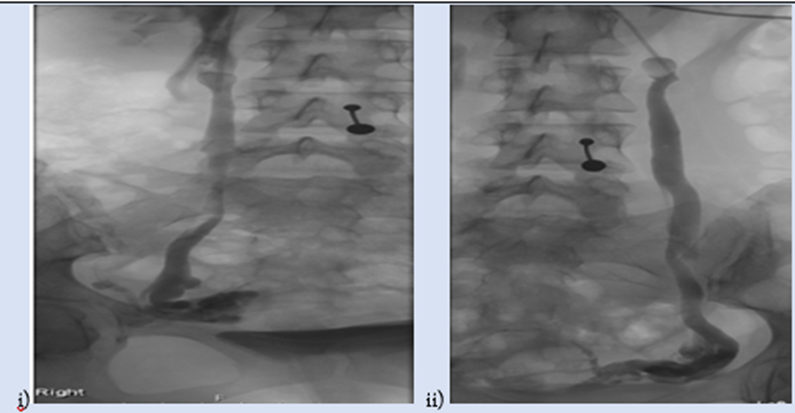
Case 6
A 31-year-old woman, P2 with two normal vaginal deliveries presented with a 4-year history of shooting pelvic pain on the right side of the abdomen. It was 4/10 in severity and had associated right hip pain and poor appetite. It had a detrimental impact on her quality of life, occasionally causing her to call in sick from her work as a school dinner lady. It was not related to her menses and occurred sporadically throughout her menstrual cycle. She was diagnosed with pelvic congestion syndrome from a transvaginal ultrasound in November 2019. A CT pelvis with contrast in October 2020 showed: ‘enlarged pelvic veins draining via bilateral prominent ovarian veins and draining into the bilateral common femoral vein. Appearances are of pelvic venous congestion syndrome. The left renal vein is compressed between the superior mesenteric artery and aorta (Nutcracker syndrome).’ Ovarian vein embolisation was performed in August 2020. Right jugular vein access was obtained, and an 8-French sheath was placed. Bilateral ovarian veins were cannulated one after the other, and embolised initially with a mixture of sclerosant (Gelfoam mixture through an occlusion balloon catheter), followed by occluding coils. Post-procedure fluoroscopy showed complete stasis of the sclerosant - Gelfoam mixture and optimal placement of the coils. Initially, she was pain-free for 1 month; but the pain returned thereafter, and was worse on the right-side of her abdomen, with associated menorrhagia. Thereafter, she was commenced on the combined oral contraceptive pill on a tricyclic basis.
Figure 7a: A right transjugular approach was used and bilateral ovarian veins were cannulated. Venogram shows bilateral ovarian vein dilatation (i) right and (ii) left.
Figure 7b: Embolisation was performed with a mixture of sclerosant – Gelfoam thorugh an occlusion balloon catheter and followed by coils. Post procedure fluroscopy showed complete stasis of the sclerosant mixture and optimal placement of the coils.
| Questions | Case 1 | Case 2 | Case 3 | Case 4 | Case 5 | Case 6 |
| Presenting symptom | 2 years of menorrhagia, irregular uterine bleeding, and chronic pelvic pain | 2-years of pelvic, lower back and hip pain, constant throughout her menstrual cycle, but worsened during menses | 10-years of pain in her left iliac fossa, lower back, and left leg. Dragging sensation in perineum She was unable to stand up for long periods | 11- years of chronic pelvic pain, deep dyspareunia, and painful, varicose veins. | 1-year of left-sided abdominal pain, worse on standing and relieved by lying down. Associated symptoms of vulval pressure and soreness | 4-years of shooting pelvic pain on the right side of the abdomen. Right hip pain and poor appetite |
| Pain Score | 0/10 | 0/10 | 3/10 | 4/10 | 0/10 | 4/10 |
| Recurrence of Symptoms | No | No | Yes | Yes | No | Yes |
| Menopausal symptoms | No | No | Menopause started age 48. Symptoms: insomnia, sweats, hot flushes, dry vagina, mood swings, anxiety, depression. Takes HRT - Kliovance for 10 years, no improvement. | No | Perimenopausal symptoms began 2022 (not after the procedure) | No |
| Effect on Libido | No | No | Secondary to the menopause. Atrophic vaginitis causing dyspareunia and affecting her libido and preventing her from initiating sexual intercourse or maintaining it for long. | Yes. Ongoing deep dyspareunia and chronic abdominal pain | No | No |
| VTE complication | No | No | No | No | No | No |
| Any Other Important Points | Nil | Nil | Nil | Nil | Nil | Nil |
Discussion
Benefits and risks of Pelvic Vein Embolisation
The table below summarises the benefits and the risks of pelvic vein embolization.
| The main benefits of pelvic vein embolisation include | The risks of pelvic vein embolisation include |
| No surgical incision is needed. | Small risk of infection after embolisation |
| Embolisation is much less invasive than conventional open surgery. | Any procedure that involves placement of a catheter inside a blood vessel carries certain risks. These risks include damage to the blood vessel (called ovarian vein thrombophlebitis), bruising or bleeding at the puncture site. |
| Evidence has shown it to be a safe procedure with relief of the symptoms of pain, and improvement in the appearances of the varicose veins. | Radiation exposure to the ovaries. However, there has been no evidence that fertility or periods are affected by the procedure. |
| A majority of women (up to 85%) find they have an improvement within 2 weeks of the procedure. | Recurrence of the varicose veins can occur in up to 10%. |
Diagnosis of PCS in literature compared to our patients
PCS can present as a wide symptomatic spectrum complicating and prolonging the diagnosis of this disease. Pelvic pain is the most common presentation; however, this can vary in its form from sharp and acute pain to chronic and dull pain2. The pain is compounded by prolonged standing, pregnancy and symptoms can be reproduced by the Valsalva manoeuvre during imaging investigation. Analogous to endometriosis, dyspareunia and urinary symptoms can also occur in PCS, making it difficult to differentiate clinically. Although, the dyspareunia associated with PCS is thought to continue after intercourse. Lower urinary tract symptoms of dysuria and urinary frequency may occur, particularly if there are varicosities affecting the bladder trigone [2]. Diagnosis of PCS is often delayed due to the above challenges and often it is not considered early on as a differential diagnosis for the cause of chronic pelvic pain. This can compound psychological symptoms that can occur in PCS, as with other chronic pelvic pain conditions, i.e., depression and anxiety, which can negatively impact a women’s quality of life, relationships, and occupations.
The diagnosis of PCS is confirmed by radiological imaging including ultrasound and CT of the pelvis as first line non-invasive methods. With these, the presence of dilated pelvic veins and assessment of the severity of the congestion can be made. Ultrasound features include torturous and dilated para-uterine veins more than 4mm in diameter or ovarian veins greater than 5-6mm. Additionally, there may be evidence of reversed or slow venous blood flow using doppler study. These features can be extenuated by the Valsalva manoeuvre [6]. Furthermore, although invasive, venography of the pelvic veins remains the gold standard method of the diagnosis and classification of the severity of PCS. The methods used include catheterisation of the internal jugular or femoral veins. This can be performed prior or concurrently with embolization of the affected veins. Of our case series 5 of the 6 patients had US or CT of the pelvis initially to investigate the CPP symptoms (Cases 1,2,3 and 6). In one of our patients both US and CT pelvis were normal, however congested pelvic veins were noted at diagnostic laparoscopy. The patient in case 5 had a CT abdomen and pelvis to assess her renal tract to investigate bilateral loin pain. This confirmed PCS due to the identification of bilateral torturous para-uterine and ovarian veins, which was further confirmed on pelvic transvaginal ultrasound.
All patients with radiologically confirmed PCS had bilateral dilated vessels involving the para-uterine veins. In all but one of these patients, the ovarian veins were also noted to be congested and the left vein was more prominent in its’ dilatation (case 2,3,5 and 6). Anatomically the right ovarian vein drains directly into the inferior vena cava, whereas the left ovarian vein drains into the left renal vein. The anastomoses of the left ovarian vein to the left renal vein is often at a right angle, increasing the likelihood of dilatation due to reflux of venous flow [7]. Those dilated vessels that were measured ranged from 6-7mm in calibre. The ovarian veins are usually normally 3-4mm in diameter [7]. In one of our patients (case 6) there was radiological evidence of Nutcracker Syndrome. This is the detection of left renal vein compression between the superior mesenteric artery and the aorta, which can lead to distal pelvic congestion syndrome, due to obstruction and pooling of venous circulation. The aim of the treatment should be to relieve the anatomical compression [8]. Case 4 was diagnosed with PCS during investigations for severe varicose veins affecting her buttock and peri-vulval area. In addition to severe ascending saphenous vein incompetence detected on a lower limb doppler, a CT venogram confirmed the diagnosis of PCS in this patient. Notably, this woman had undergone laparoscopic investigation of her CPP and dyspareunia and the significance of the ovarian vein dilatation was not noted. This highlights the possible phenomenon of increased intrabdominal pressures masking pelvic venous congestion temporarily during laparoscopy by reducing the engorgement of the pelvic vessels [2].
Management of PCS
The chronic pain associated with pelvic congestion syndrome can be debilitating, affecting the patient’s activity of daily living and personal circumstances. Initial management begins with analgesia as first line, with paracetamol, NSAIDS and opioids. All our patients were taking these either regularly or on an as required basis to provide relief prior to their embolisation. Previously, following failed medical management, treatment for PCS involved surgical option of hysterectomy and bilateral salpingo-ophorectomy. In 2003, Chung et al. carried out a randomised control study which randomised women with PCS who failed medical treatment to one of three arms: hysterectomy and bilateral oophorectomy with post-operative hormone replacement; hysterectomy with unilateral salpingo-oophorectomy of the affected venous congested side and ovarian vein embolisation. The study concluded that there was improvement in pain score after embolisation, which was significantly more effective compared to the other methods. The study advised that ovarian and/or internal iliac vein embolisation was well accepted and an effective treatment for PCS [9].
A systematic review of 970 patients who underwent ovarian vein or pelvic vein coil embolisation by Sutanto et al 2022, also found that this treatment was effective and resulted in clinical improvement of pain scores. Pooled analysis revealed mean improvements of 5.47 points (95% CI, 4.77-6.16) on the visual analogue scale, as well as significant improvement in common symptoms of urinary urgency and dyspareunia associated with PCS [10]. They also found complications were rare and recurrence of symptoms of PCS were found to be about 5.9-25
Discussion of the results table
Following ovarian vein embolization 3 patients felt complete resolution of their chronic pain symptoms and gave post treatment pain scores of 0/10. Recurrence of pain was seen in 3/6 patients with pain scores ranging from 3-4/10. Two of these patients had later attained menopause (one aged 48 and the second patient 6 years following the procedure). Two patients reported concerns regarding libido. One of the patient’s complained of superficial dyspareunia thought to be resulting from atrophic vaginitis and oestrogen deficiency of menopause. The other patient had reported no improvement in her chronic deep dyspareunia and pelvic pain. There were no documented complications of VTE, or puncture site haematoma reported amongst our cases.
Conclusion
Pelvic congestion syndrome (PCS) is an underdiagnosed cause of chronic pelvic pain in women. It commonly affects young, multiparous women and is caused by ovarian and pelvic varicose veins. It is associated with deep dyspareunia, haematuria, proteinuria, and pelvic pain, that is typically exacerbated by prolonged standing, sexual intercourse or menstruation [11]. There are multiple treatment options for PCS, including: hormonal therapy with medroxyprogesterone acetate and goserelin, laparoscopic ovarian vein ligation and hysterectomy and BSO. We present a case series of 6 patients who underwent ovarian vein embolisation as definitive treatment for PCS. From our study we concluded that it is an effective and safe treatment option for PCS, with a low risk for complications, which can significantly improve the quality of life for patients suffering from this chronic, debilitating condition.
Disclosures
None to disclose.
References
- Marcelin C, Le Bras Y, Molina Andreo I, Jambon E, Grenier N, et al. (2022). Diagnosis and Management of Pelvic Venous Disorders in Females. Diagnostics (Basel), 12(10):2337.
Publisher | Google Scholor - Osman MW, Nikolopoulos L, Jayaprakasan K, Raine-Fenning N, et al. (2013). Pelvic congestion syndrome. The Obstetrician & Gynaecologist, 15:151-157
Publisher | Google Scholor - Kolber MK, Cui Z, Chen CK, Habibollahi P, Kalva SP. (2021). Nutcracker syndrome: diagnosis and therapy. Cardiovasc Diagn Ther, 11(5):1140-1149.
Publisher | Google Scholor - (2023). Normal venous anatomy. British Society of Interventional Radiology.
Publisher | Google Scholor - Smith M. (2017). Sonographic View of Pelvic Congestion Syndrome. Journal of Diagnostic Medical Sonography, 33(3):193-198.
Publisher | Google Scholor - Pelvic congestion syndrome.
Publisher | Google Scholor - Phillips D, Deipolyi AR, Hesketh RL, Midia M, Oklu R, et al. (2014). Pelvic congestion syndrome: etiology of pain, diagnosis, and clinical management. J Vasc Interv Radiol, 25(5):725-733.
Publisher | Google Scholor - O'Brien MT, Gillespie DL, et al. (2015). Diagnosis and treatment of the pelvic congestion syndrome. J Vasc Surg Venous Lymphat Disord, 3(1):96-106.
Publisher | Google Scholor - Chung MH, Huh CY, et al. (2003). Comparison of treatments for pelvic congestion syndrome. Tohoku J Exp Med, 201:131-138.
Publisher | Google Scholor - Sutanto SA, Tan M, Onida S, Davies AH, et al. (2022). A systematic review on isolated coil embolization for pelvic venous reflux. J Vasc Surg Venous Lymphat Disord, 10(1):224-232.
Publisher | Google Scholor - Basile A, Failla G, Gozzo C, et al. (2021). Pelvic Congestion Syndrome. Seminars in Ultrasound, CT and MRI. 42(1):3-12.
Publisher | Google Scholor