case report
Ossified Inflammatory Epulis: A Case Report
1Department of stomatology and dental medicine, Mahres hospital, Sfax, Tunisia.
2Department of stomatology and dental medicine, Hedi Chaker Hospital, Sfax, Tunisia.
3*Department of anesthesiology and intensive care, Habib Bourguiba Hospital, Sfax Tunisia.
*Corresponding Author: Salma ketata,Department of anesthesiology and intensive care, Habib Bourguiba Hospital, Sfax Tunisia.
Citation: Hassen. M, Ines. H, Salma. K, Imene. Z. (2023). Ossified Inflammatory Epulis: A Case Report. Dentistry and Oral Health Care, BioRes Scientia Publishers, 2(3):1-4. DOI: 10.59657/2993-0863.brs.23.014
Copyright: © 2023 Salma ketata, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: August 28, 2023 | Accepted: September 11, 2023 | Published: September 15, 2023
Abstract
Introduction: Etymologically, the epulis is a lesion that develops at the level of the gum. It is classically defined as a benign circumscribed hyperplastic pseudotumor of the gums.
Observation: A 59-year-old patient consulted for a posterior left mandibular gingival mass related to 37 and 38 dilapidated. The lesion being well limited, of firm consistency and slow evolution without underlying osteolysis, evoked a fibrous epulis. The treatment consisted of eliminating the local irritant (RSD, extraction of the dental roots) and the complete excision of the lesion. Histological examination reveals the diagnosis of ossified inflammatory epulis.
Discussion: Epulis is a common pseudotumor of the oral mucosa. Several varieties of epulis are described. Ossifying epulis is a controversial entity from a terminology point of view but it has the particularity of having bone and sometimes cemental metaplasia within the connective stroma which can sometimes be detectable on radiography. The success of the treatment remains dependent on the technique used by the practitioner, the follow-up, and the patient's degree of motivation for oral hygiene. The role of the first-line dentist remains important in the diagnosis, prevention, and treatment of this type of lesion as well as in the clinical follow-up.
Keywords: epulis; gum disease; mandibular hyperplasia
Introduction
Many authors have defined epulis as a lesion located on the surface of the gums. It is a circumscribed hyperplastic benign pseudotumor of the gums [1]. Other authors mention the inflammatory nature of epulis, which results from defective healing or repair of a gingival lesion such as gingival inflammation or traumatic lesion by an ill-fitting prosthesis [2].
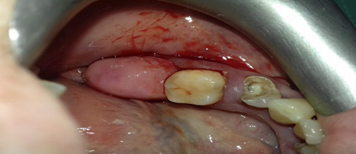
Figure 1: Left Mandibular Hyperplasia
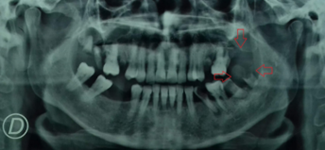
Figure 2: Panoramic X-ray
Presentation of the case
The 59-year-old patient with no medical history was consulted for asymptomatic left mandibular hyperplasia that was pink in color and hard in consistency (Figure 1). The intraoral examination showed a precarious periodontal context and several root tips. In the lower-left sector, the 34 is dilapidated with a periapical image. The 37 is dilapidated. The number 38 is in root-end condition with gingival inflammation. The preoperative panoramic X-ray showed the presence of the root tips of the 37 and the 38 under the gingival formation (Figure 2). The patient performed the clinical analyses. She underwent root scaling and surfacing at the clinic and excision of a 1.5 cm gingival formation at the level of the left mandibular gum next to the molars. The clinical stages are first anesthesia (Figure 3), second, removal of the gingival formation and extraction of the 34 (Figure 4), third, the suture extends from the extraction site from the 34 to the 38 (Figure 5), and finally control of the procedure (Figure 6). Histological analysis showed that the hyperplasia is an ossified inflammatory epulis. Once the excision of the gingival formation was carried out, the root tips of the 37 and the 38 extras in the panoramic X-ray were not found. The patient mentioned a spontaneous fall of these root tips.
Figure 3: Anesthesia
Figure 4: Removal of the gingival formation and extraction of 34.
Discussion
First of all, it should be noted that the types of epulis according to the anatomopathological aspect are simple epulis, inflammatory epulis, vascular or angiomatous epulis (pyogenic granuloma), fibrous epulis (irritative) and epulis with giant cells or epulis with myeloblasts or peripheral granulomas with giant cells [1]. To have an ossification of the inflammatory epulis and that it evolves towards an ossified inflammatory epulis as shown by the anatomopathological analysis, it takes a long time. The ossification stage corresponds to a late stage in the development of inflammatory epulis (3). We can say that the patient waited a long time before consulting because of the absence of pain. Regarding the spontaneous loss of teeth according to the patient's statement, two mechanisms can explain this phenomenon, and most likely, they are combined [4,5,6]. The epulis is of inflammatory origin, whose inflammation with the significant decay of the teeth has overcome the attachment of the alveoli-dental ligament. And the hyperplasia in our case is of a stiff consistency, it has pushed the ends of the roots of the 37 and the 38 as they grow, which favors their fall. Epulis results from defective healing or repair of a gingival lesion. The factors that can be evoked which are behind this phenomenon are multiple. Lack of recovery may be due to poor hygiene, irritating edges of root tips, trauma during chewing, etc.
Conclusion
Epulis is a prevalent lesion. It is necessary to have care in a specialized center but the role of the front-line dentist remains important. For the success of the surgical treatment, it is important to clean up the oral cavity and reduce the sources of gingival inflammation. The patient's degree of motivation for oral hygiene must be as high and must be consulted as soon as possible. It is also necessary to try to fight as much as possible against the factors favoring this type of lesion. Prevention is better than cure.
References
- LES TUMEURS BENIGBES DE LA MUQUEUSE BUCCALE.pdf [Internet]. [cité 29 déc 2021]. Disponible
Publisher | Google Scholor - JOHNSON Ameswué Kpogbé E. (2011). Tumeurs béningnes et kystes maxillo- mandibulaires [médecine]. UNIVERSITE DE OUAGADOUGOU.
Publisher | Google Scholor - Epulis inflammatoire – Epulis fibreuse +/- ossifiante – Dermatologie buccale [Internet]. [Cité 27 mars 2022].
Publisher | Google Scholor - Agence Nationale d’Accréditation et d’Evaluation en Santé (ANAES). (1998). Acta Endosc. avr 28(2):151‑155.
Publisher | Google Scholor - Sibaud V, Vigarios E, Tavitian S, Cougoul P, de Bataille C, Campana F, et al. (Accroissements gingivaux : approche pragmatique. Annales de Dermatologie et de Vénéréologie, 143(6-7): 467‑481.
Publisher | Google Scholor - Côté O. Utilisation du L-PRF conjointement à la thérapie initiale dans le traitement de la parodontite modérée à sévère ; Une étude randomisée contrôlée à double aveugle,73.
Publisher | Google Scholor