Research Article
Occupational Hazards/ Risks Among Dental Staff in Afghanistan
1School of dentistry, Kabul Medical University of Sciences, Afghanistan.
2Statistics department of Mathematics Faculty, Kabul University, Afghanistan.
*Corresponding Author: Shamila Azimi, School of dentistry, Kabul Medical University of Sciences, Afghanistan.
Citation: Azimi S, Azimi S, Azami M. (2024). Calcium Pyrophosphate Deposition Disease. Journal of BioMed Research and Reports, BioRes Scientia Publishers. 4(6):1-9. DOI: 10.59657/2837-4681.brs.24.084
Copyright: © 2024 Shamila Azimi, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: April 29, 2024 | Accepted: May 20, 2024 | Published: May 21, 2024
Abstract
Background: The risks that are exclusive to the dental care setting are known as occupational hazards in dentistry. Aims: Dangers. This research analyses the prevalence of occupational hazards among dental staff in Afghanistan. Methodology: A cross-sectional study, using an online survey including qualitative and quantitative questions. Data collection was started from 16th .03.2021 till 12th.05.2021 and completed by 206 dentists. The questionnaire was designed in Google form and data was collected by online link via social media such as “Facebook, and WhatsApp”. Result: According to a survey the most common occupational hazards among dentists are musculoskeletal problems in Afghanistan. Among musculoskeletal problems, most of the responders had complained of backache while nobody had noticed any pain in their elbow joint. 55% of dentists were vaccinated for common diseases (HBV, HCV, HAV, etc.) and 41.6% were not vaccinated. 74% of participants strongly agreed that dentistry is a stressful field and 26.7% had a high level of fatigue due to work at the end of the day. Conclusion: musculoskeletal problems especially backache are the most prevalent hazards among Afghan dentists and Continuing education programs have to be conducted to overcome these hazards.
Keywords: occupational hazards /risks; dental staff; afghanistan
Introduction
Any risk encountered at work is referred to as an occupational hazard. It can also relate to labor, materials, substances, procedures, or circumstances that either directly or indirectly contribute to workplace illnesses or accidents [1]. The origins of occupational hazard awareness can be found in the 18th century, when the "Father of Occupational Medicine," Bernadino Ramazzini, realized how occupation affected the dynamics of health and illness [2]. The risks that are exclusive to the dental care setting are known as occupational hazards in dentistry. Although it has been said that modern dentistry is the least dangerous of all professions, there are still several risks that cast doubt on this claim and create workplace dangers. Dentists confront many work-related risks when performing their professional duties. These lead to the emergence of several occupationally-specific illnesses that worsen over time. They frequently lead to illnesses and sickness complexes, some of which are thought to be occupational illnesses [3,4]. Dental professionals are exposed to a range of work-related risks when practicing dentistry, including extended work hours, passive work environments, nervous patients, and aerosol exposure from high-speed rotating handpieces [5]. Muscle and joint problems arise during a dentist's professional education and persist throughout their career. The hands, shoulders, neck, and spine are all affected. For dentists, back pain represents a significant risk to their occupational health. Such postural conditions are present during dentistry treatments, increasing the possibility of the body twisting and contorting, varicose veins, etc. [6]. Biological risks are caused by pathogenic organisms that are human-derived, such as bacteria, fungi, and viruses. A dentist may contract an infection directly or indirectly. Many different kinds of substances can be toxic when giving care, such as formaldehyde, silica, powdered natural rubber latex (NRL), beryllium, and the most hazardous mercury [8]. Among healthcare providers and patients, percutaneous exposure events such as needle sticks and sharp tool injuries are the most effective way to spread blood-borne infections [9]. Numerous bodily cells can be harmed by both ionizing radiation, such as X-rays, and other types of radiation, such as visible and UV light. One proven risk factor for cancer is ionizing radiation [10]. Specific viral diseases, such as hepatitis B and acquired immunodeficiency syndrome (AIDS), can be fatal. Bacterial diseases such as syphilis and TB provide a serious concern in the field of dentistry [11-12]. An inherent aspect of a dentist's work is dealing with stressful situations. It is the primary psychological risk that dentist offices observe [13-14]. Dentists experience stress from scenarios such as anesthetizing patients, helping them overcome pain and fear, dealing with unforeseen emergencies that could endanger their lives, or performing treatments for which there is a doubtful prognosis. Because of this, the dentist may experience elevated stress, hypertension, exhaustion, insomnia, irritability, and depression [15]. In dental offices, latex gloves are the primary source of allergic skin reactions. A minor amount of adverse skin reaction can also be caused by various dental materials, detergents, lubricating oils, solvents, and chemicals used in X-ray processing [16]. To lessen the complications of these risks, suitable intervention studies and ongoing education are required. Before implementing this kind of educational program, we need baseline data on the topic's prevalence and level of awareness within the research group. The majority of research on dental professionals' occupational hazards is carried out in affluent nations [17-18].
The developed world is the site of the majority of studies on health risks among dentists, with developing countries providing the least amount of data. Thus, the purpose of this study was to determine the prevalence of occupational hazards among Afghan dentists employed by the government and private sectors of clinics. Finding out if dentists were taking the right precautions for their prevention was the study's other goal [19-20]. The collected data can be utilized by Afghan health policymakers to develop strategies and implement them in the community to lower the frequency of risks among dentists.
Methods and Materials
It was chosen to include a maximum number of dental offices in the survey because information on the complete number of registered dental clinics was unavailable. The undergraduate dental students who did not work in a dental office and dentists who were unwilling to participate in the survey were not included in the study. Dentists from all over Afghanistan who hold positions in dental offices and provide dental treatment and who were willing to participate in the survey were asked to complete the online questionnaire. The ethics committee of the institution granted the study ethical clearance. The study participants gave their informed permission both orally and in writing. Data collection took place over two months, from March 16, 2021, to May 12, 2021.There were 206 responses at all, and 203 of them were legitimate. The research methodology chosen was an online survey approach. A closed-ended, 23-question survey was created to evaluate the prevalence of workplace risks and the actions taken to avoid them. The following information was collected from the topics: age, gender, qualification, years of experience, and province. In addition, questions evaluated their history of problems with hearing, musculoskeletal problems (such as carpel tunnel syndrome, back pain, and cervical spinal arthritis), allergies (such as latex, acrylic, and other dental materials), stress, and eye injuries. Questions about administering vaccinations and adhering to different cross-infection control procedures at the clinic were included in the questionnaire's second section. Finally, the participants were questioned about their level of physical activity, work satisfaction, stress, and how they managed it over their holiday. Prior to the primary survey, 15 dentists participated in a pretest of the questionnaire. Several of the questions were changed in response to the individuals' input. Frequency tables were used in the analysis of the data to show the dental staff's responses. The questionnaire was created using a Google form, and data was gathered online via a link from popular social media platforms including Facebook and WhatsApp. SPSS software version 17 was utilized for the study.
Results
The survey included 206 dentists, among them 75.7% (n=156) were male and 24.3% (n=50) were female dentists. The age of dentists ranged from 25-65 years, with a mean of 30±5.2 age years, which is the average working-class age in Afghanistan. Years of clinical practice ranged from 1-30 years. About 25.6% of the participants practiced at dental offices for 2 years followed by 3 years of clinical experience (15.7%). Transition of infectious diseases by patients to dentists, 25% of participants didn't know if they were infected or not, 62.6% were not infected, and an important percentage 12.7 % those dentists were infected by their patients while working in a dental office. Of the 203 participants who filled out the questionnaire, 53 dentists had positive responses about some infectious disease, of which flu was the most transmitted disease 62.3%, covid-19 and sore throat were also observed with lower levels than flu. More details in table (1). Although the survey comprised all provinces of Afghanistan, dentists participated from 18 provinces out of 34, the majority of them were from Kabul 64% (n=132), Herat 9.2% (n=19), Ghazni 4.3%(n=9) and Mazar 3.8%(n=8). 85.9% (n=177) dentists practiced general dentistry whereas only 14.1% (n=29) practiced their specialty. 5.8% (n=12) of dentists were left-handed whereas the rest 94.2% (n=194) were right-handed dentists.
Table 1: shows the years of dentist’s experiences and transmission of infectious disease.
| Years of clinical practices | Number | Percentage | Diseases | Number | Percentages |
| < 1> | 6 | 2.9 | Flu | 33 | 16.28 |
| 1 year | 20 | 9.85 | Covid-19 | 20 | 9.8 |
| 2 years | 52 | 25.6 | Sore throat | 17 | 8.38 |
| 3 years | 32 | 15.7 | Hepatitis | 3 | 1.48 |
| 4 years | 20 | 9.85 | Respiratory disease | 3 | 1.48 |
| 5 years | 26 | 12.8 | Skin problems | 2 | 0.98 |
| 6-10 years | 33 | 16.2 | Total | 77 | 38% |
| Nov-30 | 14 | 6.9 |
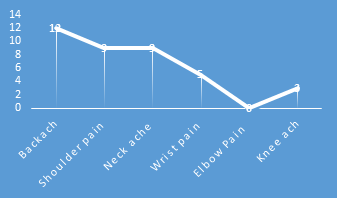
The most common occupational hazards are musculoskeletal problems. Among musculoskeletal problems, most of the responders had complained of backache while nobody had noticed any pain in their elbow joint. “See below Figure (1).” Based on the survey 62% of dentists always used chairs during treatment procedures whereas 4.9% never used them.
Figure 1: shows the prevalence of musculoskeletal problems
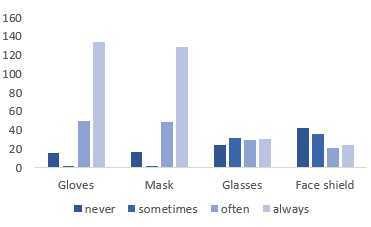
In observation of safety procedures, the survey showed that 57.7% of dentists always took a systemic history from their patients before starting the treatment while 32.5% often did it, 7.3% usually, 1.5% sometimes but 1.5% of dentists never took systemic history. 80.1% of dentists had ventilation systems in their clinics, while 19.9% of them hadn't, also 55% of dentists were vaccinated for common diseases (HBV, HCV, HAV, etc) and 41.6% were not vaccinated. Among participants, 87.8% of them had assistants at their dental clinics while 12.2% worked without any assistant. 19.2% of participants had latex allergy, while 75.9% hadn't and 4.9% didn't know about it. As the results show most dentists are using masks and gloves while working with patients whereas there were only a few percentages of dentists who used glasses and face shields. "For more details see Figure (2).
Figure 2: shows the rate of use of safety appliances among dentists
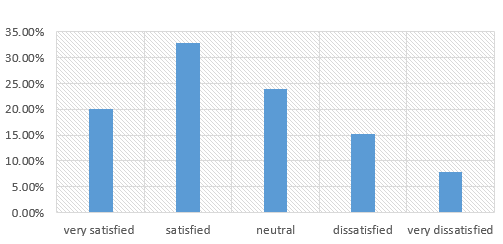
Hearing problems respectively from very low to low, medium, high, and very high levels were 73%, 21%, 7%, and 2%. Moreover, Vision problems were 66% very low, 28% low, 21% medium, 5% high, and 2% very high conducted. The percentage of respiratory problems due to occupational hazards among dentists was 7% very low, 15% low, 7% medium, and 7% high. Prevalence of headaches was different than other problems 56% of dentists had very low levels of headache during work in a dental office, 38% low, 48% medium, 17% high, and 5% had very high levels of headache. The rate of fatigue due to work at the end of the day among participants was 27.6% at the high level, 57.3% at the medium level, and 15.1% at the low level. 74% of participants strongly agreed that dentistry is a stressful field while 19% disagreed and 7% were neutral about it. Despite this 70.4% of dentists enjoyed their occupation, but for less than 3.4 dentistry is not an enjoyable occupation at all. If there was a chance to change the profession, 56.8% of participants said that they wouldn’t change it, while 26.2% of them would change that with any other fields and 17% didn't know if they were changed or not. 20.10% of our participants were very satisfied, 32.8% were satisfied with the incomes that they earn through their profession and 15.2% were dissatisfied. "For more details you can see the Figure (3).”
Figure 3: shows the satisfaction rate of participants with the incomes they earn through their profession.
Discussion
According to a study published in India, 39.8% of those surveyed reported having musculoskeletal discomfort, with necks and backs being among the more common painful areas. This finding is consistent with the current study, which found that doctors between the ages of 25 - 35 (62.1%) and with less than two years of professional experience were also likely to suffer from musculoskeletal pain in the back, neck, and shoulder regions. A survey of dentists in Queensland, Australia, revealed that dentists with less experience and younger age groups were more likely to report MSDs (musculoskeletal diseases) of the neck, upper back, and shoulders [21,22]. It could be because experienced dentists know how to modify their posture and methods of operation. It has been shown that stretching exercises, especially yoga, are good for MSDs because they improve circulation and ease tense muscles for back and neck pain, shoulder pain, wrist and forearm issues, tension headaches, and cervicogenic headaches, yoga proved beneficial [23-27]. According to the findings of the study, the majority of male doctors have wrist and spine joint pain. Conversely, female dentists frequently complained of neck problems. This explains why people who labor in this area for a few years eventually develop various illnesses like cervical and lumbar disk arthritis. An investigation was carried out at Pakistan [28]. While only approximately 31% of participants in our study reported having elbow pain, 53% of participants reported having it. These symptoms are frequently associated with the continual, repetitive movement of the arms that occurs during dental procedures, which puts stress on the elbow and wrist [28]. The current investigation noted that the dentist's working position involved a bent neck and abducted arm. The majority of dentists employed a direct technique to visualize maxillary teeth when doing seated dentistry. One of the main causes of neck pain in dentists was this extension of the neck for improved vision. Sixty-four percent of dentists in Danish research who used a seated technique reported having back pain [29,30]. According to the results transmission of infectious disease is not eminent, at all 38% of dentists were infected by their patients in dental clinics. There is no record of HIV in our results that we could be satisfied with that. About more than half of dentists (55%) were vaccinated for common diseases and that could be causing the lower prevalence of (HBV, HSV, and HVC) diseases among dental staff in Afghanistan. Because the majority of dentists, or 64% of the total, were from Kabul, which is the capital and a more developed city than other provinces that have better knowledge, it is hoped that most dentists, male, and female, used safety equipment like masks, gloves, eyeglasses, and face shields. This may have something to do with their level of awareness. Furthermore, the high degree of adherence to safety protocols by Afghan dentists is demonstrated by the fact that over half of our participants use chairs during treatments, use the clinic's ventilation system, obtain medical histories from patients, and have dental assistants. According to a study done in Pakistan (Karachi), 40.98 of the population has impaired hearing [28]. In contrast, our results showed that 25.75 percent of Afghan dental staff members had hearing issues. This indicates that the prevalence of hearing issues in Afghanistan is two times lower than in other neighboring countries, with only 2% of dentists experiencing severe hearing loss. A total of 24.4% of dentists reported having eye difficulties as a result of working in a dental clinic; more than half of the participants had extremely low-level eye problems, and only 2% had high-level problems. Of Pakistani dentists, 44.68% had eye infections, which is half of the total. It could be the result of more Afghan dentists wearing "eyeglasses" or other safety equipment incorrectly while at work. Stress related to workload (patient) was prevalent in psychological hazards [28]. In both their personal and professional lives, dentists encounter a lot of difficult situations [31]. According to our study, 74% of dentists reported feeling stressed out and exhausted from work at the end of the day. A similar study in England found that 60% of general dentists experience anxiety, tension, or depression; 58% report headaches; 60% report having trouble falling asleep at night; and 48% report feeling exhausted for no apparent reason [20]. There may be a connection between the high frequency of weariness and particular aspects of their jobs. Our research indicates that physical ailments and problems manifest early in dentistry professions. The high frequency of physical diseases could be caused by a lack of knowledge about ergonomics and an uncomfortable workplace, which was a typical occurrence because of antiquated equipment [33]. Additionally, 26.2% of dentists said that they would prefer to switch to any other discipline instead of dentistry if allowed to change careers. The cause was unclear, although it might have had to do with the significant danger of health issues in this line of work. According to certain research, dentists are more likely than other high-risk medical professionals to have severe health issues [34].
Conclusion
The majority of survey respondents reported having musculoskeletal issues, which may have been brought on by a lack of knowledge about ergonomics. The Ministry of Higher Education should include ergonomics in the dentistry faculty's curriculum, and faculty members should host conferences or seminars on dental occupational hazards and preventive measures for students during the university year to increase student awareness of these risks and the use of ergonomic solutions to make dental staff's jobs more comfortable. To see the patient's mouth clearly and reduce errors during treatment, the dentist must bend their body. Because of this, treating a patient can take anywhere from ten to over an hour. Afterward, the patient may experience excruciating pain from strained muscles. As a result, we advise all dentists, whether practicing in Afghanistan or elsewhere, to take breaks after ten to fifteen minutes of patient care. Furthermore, dentists ought to utilize these voids to perform yoga poses or warm-up activities to preserve joint flexibility and mobilize muscles on bones. This is the most straightforward and feasible approach to prevent chronic ailments like wrist, neck, and back pain, as well as the associated side effects. It supports dentists in providing patients with efficient care and injury prevention. Although the prevalence of infectious diseases among the survey participants was thankfully very low and most dentists had received vaccinations against them, the government still needed to mandate vaccinations for all dentists before they began their practical work to bring the rate down to almost zero.
Strengths and Limitations
This study's strength is that it is the first of its kind to be conducted among students pursuing health professions in Afghanistan; there haven't been any prior reports. Additionally, the research ethics committee of Kabul University of Medical Sciences oversaw and confirmed this study in compliance with the ten particular Helsinki principles (scientific requirements and research protocols, informed consent, privacy and confidentiality, research registration and publications, and so on). Owing to the coronavirus and the quarantine, we were only able to obtain information online from dentists; no physical data collection was possible. This information is only a sample of information from dentists who had access to the questionnaire link; it is insufficient to fully resolve and discover the answers to the questions. Therefore, more comprehensive data is required to include the majority of Afghans. Male respondents to the survey outnumbered female respondents by a significant margin. Because of this imbalance, the quality of our data is affected, and we are unable to analyze or evaluate the precise association between a given occupational hazard and gender among Afghan dental staff members. Data Sharing Statement. The research ethics committee of Kabul University of Medical Sciences has the data that support the study's conclusions, but there are limitations on their availability. These data were utilized under license for the current study; thus, they are not publicly available. If you make a legitimate request and have the consent of only the first author, you can obtain data from this work by Shamila Azimi
Declarations
Acknowledgments
The authors express their sincere gratitude to Prof. Mr. Jalal Ataie of Breda University of Applied Sciences, our research mentors, for their guidance and support, without which the completion of this study would not have been feasible. As well as the KEIHAN Foundation for delivering these programs.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Disclosure
The authors declare no competing interests in this work.
References
- Asher RS, McDowell J, Acs G, Belanger G. (1993). Pediatric infection with the human immunodeficiency virus. J Colo Dent Assoc,72:25-28.
Publisher | Google Scholor - Am J Public Health, 91(9):1382.
Publisher | Google Scholor - Akesson I, Lundborg G, Horstmann V, Skerfving S. (1995). Neuropathy in female dental personnel exposed to high-frequency vibrations. Occup Environ Med, 52:116-123.
Publisher | Google Scholor - Jolanta: S. (1999). Occupational hazards of dentistry. Ann Agric Environ Med, 6:13-19.
Publisher | Google Scholor - Hovius M. (1992). Disinfection and sterilization: the duties and responsibilities of dentists and dental hygienists. Int Dent J, 42:241-244.
Publisher | Google Scholor - Rundcrantz BL, Johnsson B, Moritz U. (1991). Pain and discomfort in the musculoskeletal system among dentists. A prospective study. Swed Dent J. 115:219-228.
Publisher | Google Scholor - Szymańska J. (1999). Occupational hazards of dentistry. Ann Agric Environ Med, 6:13-19.
Publisher | Google Scholor - Azari Rm, Ghadjari A, Nejad Mrm, Faghih N. (2008). Airborne Microbial Contamination of Dental Units Tanaffos, 7(2):54-57.
Publisher | Google Scholor - Leggat, Peter A, Kedjarune, Ureporn, and Smith, Derek R. (2007). Occupational health problems in modern dentistry – a review. Industrial Health, 45:611-621.
Publisher | Google Scholor - Kai M, Luebeck EG, Moolgavkar SH. (1997). Analysis of the incidence of solid cancer among atomic bomb survivors using a two-stage model of carcinogenesis. Radiat Res, 148:348-58.
Publisher | Google Scholor - Ayatollahi J, Bahrololoomi R, Ayatollahi F. (2005). Vaccination of dentist and other oral health care providers. J Den Med.18:5-14.
Publisher | Google Scholor - Samaranayake P. (2022). Re-emergence of tuberculosis and its variants: Implications for dentistry. Int Dent J, 52:330-336.
Publisher | Google Scholor - Rodríguez Vázquez LM, Rubiños López E, Varela Centelles A, Blanco Otero AI, Varela Otero F, Varela Centelles P. (2008). Stress amongst primary dental care patients. Med Oral Patol Oral Cir Bucal. 13: E253-E256.
Publisher | Google Scholor - Winwood PC, Winefield AH, Lushington K. (2003). The role of occupational stress in the maladaptive use of alcohol by dentists: A study of South Australian general dental practitioners. Aust Dent J, 48:102-109.
Publisher | Google Scholor - Gortzak RA, Stegeman A, Ten Brinke R, Peters G, Abraham Inpijin L. (1995). Ambulant 24-hour blood pressure and rate of dentists. Am J Dent, 8:242-244.
Publisher | Google Scholor - Rubel DM, Watchorn RB. (2000). Allergic contact dermatitis in dentistry. Aust J Dermatol. 41:63-69.
Publisher | Google Scholor - Leggat PA, Smith DR. (2006). Prevalence of percutaneous exposure incidents amongst dentists in Queensland. Aust Dent J, 51:158-161.
Publisher | Google Scholor - 29-Leggat PA, Chowanadisai S, Kukiattrakoon B, Yapong B, Kedjarune U. (2001). Occupational hygiene practices of dentists in southern Thailand. Int Dent J, 51:11-16.
Publisher | Google Scholor - Leggat PA, Smith DR. (2006). Prevalence of percutaneous exposure incidents amongst dentists in Queensland. Aust Dent J, 51:158-161.
Publisher | Google Scholor - Leggat PA, Chowanadisai S, Kukiattrakoon B, Yapong B, Kedjarune U. (2001). Occupational hygiene practices of dentists in southern Thailand. Int Dent J, 51:11-16.
Publisher | Google Scholor - Mehta A, Gupta M, Upadhyaya N. (2013). Status of occupational hazards and their prevention among dental professionals in Chandigarh, India: A comprehensive questionnaire survey. Dent Res J, 10:446-451.
Publisher | Google Scholor - Leggat PA, Chowanadisai S, Kukiattrakoon B, Yapong B, Kedjarune U. (2001). Occupational hygiene practices of dentists in southern Thailand. Int Dent J. 51:11-16.
Publisher | Google Scholor - Ohlendorf D, Naser A, Al. (2020). Prevalence of Musculoskeletal Disorders among Dentists and Dental Students in Germany. Int J Environ Res Public Health. 24:17:8740.
Publisher | Google Scholor - Bozkurt S, Demirsoy N, Günendi Z. Risk factors associated with work-related musculoskeletal disorders in dentistry. Clin Invest Med, 39(6):27527.
Publisher | Google Scholor - Ísper Garbin AJ. (2017). Musculoskeletal disorders and perception of working conditions: A survey of Brazilian dentists in São Paulo. Int J Occup Med Environ Health, 30:367-377.
Publisher | Google Scholor - Gandolfi MG, Āsana for Neck. (2023). Shoulders, and Wrists to Prevent Musculoskeletal Disorders among Dental Professionals: In-Office Yóga Protocol. J Funct Morphol Kinesiol, 8(1):26.
Publisher | Google Scholor - Al Khalili Y, Ly N, Murphy PB. (2023). Cervicogenic Headache. 2022 Oct 3. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing.
Publisher | Google Scholor - Abhishek, Mohit, etc. (2013). Status of occupational hazards and their prevention among dental professionals in Chandigarh, India: A comprehensive questionnaire survey. Dental Research Journal, 10(4).
Publisher | Google Scholor - Milerad E, Ekenvall L. (1990). Symptoms of the neck and upper extremities in dentists. Scand J Work Environ Health, 16:129-34.
Publisher | Google Scholor - Bassett S. (1983). Back problems among dentists. J Can Dent Assoc, 49:251-256.
Publisher | Google Scholor - Grace E. (1996). Dentistry, stress, and substance abuse. MSDA J. 39:77-79.
Publisher | Google Scholor - Myers HL, Myers LB. (2004). ‘It’s difficult being a dentist’: stress and health in the general dental practitioner. Br Dent J, 197:89-93.
Publisher | Google Scholor - Myers HL, Myers LB. (2004). ‘It’s difficult being a dentist’: Stress and health in the general dental practitioner. Br Dent J, 197:89-93.
Publisher | Google Scholor - J Res Adv Dent, 2017. 6(2):110-112.
Publisher | Google Scholor