Case Report
Neuroimages: Ischemic Zone and Tubercular Zone-Two Faces of the Same Coin
1Department of Neurology, Mahatma Gandhi Medical College and Hospital, Mahatma Gandhi University of Health Sciences and Technology, Rajasthan, India.
2Guru Gobind Singh Medical College and Hospital, Faridkot, Punjab, India.
*Corresponding Author: Himanshu kaushal, Department of Neurology, Mahatma Gandhi Medical College and Hospital, Mahatma Gandhi University of Health Sciences and Technology, Rajasthan, India.
Citation: Kaushal H, Goyal G, Bhatt R, Kain R. (2024). Neuroimages: Ischemic Zone and Tubercular Zone- “Two Faces of the Same Coin”, Clinical Research and Reports, BioRes Scientia Publishers. 2(2):1-2. DOI: 10.59657/2995-6064.brs.24.021
Copyright: © 2024 Himanshu kaushal, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: January 09, 2024 | Accepted: January 25, 2024 | Published: February 02, 2024
Abstract
Central nervous system tuberculosis (CNS TB) is one of the extrapulmonary manifestations of tuberculosis which poses a great burden in the developing world in the form of high morbidity and mortality if not recognized and treated timely. Vascular complications in infectious diseases including tuberculosis (TB) are of paramount importance as they mimic atherosclerotic lesions of small as well as large vessels. Moreover, mortality in patients with CNS TB increases to threefold if there are vascular complications in the form of stroke.
Keywords: neuroimages; ischemic zone; tubercular zone
Introduction
Central nervous system tuberculosis (CNS TB) is one of the extrapulmonary manifestations of tuberculosis which poses a great burden in the developing world in the form of high morbidity and mortality if not recognized and treated timely. Vascular complications in infectious diseases including tuberculosis (TB) are of paramount importance as they mimic atherosclerotic lesions of small as well as large vessels. Moreover, mortality in patients with CNS TB increases to threefold if there are vascular complications in the form of stroke [1]. The infarction patterns vary from small, medium and large vessel infarction. The small vessel infarction patterns are characteristic in the setting of infection and absence of risk factors for atherosclerosis which are discussed here.
Case Presentation
Case 1
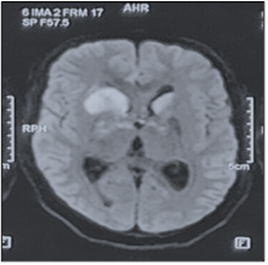
36-year-old male recently diagnosed with miliary pulmonary tuberculosis presented with fever and weakness of left upper and lower limb with upper motor neuron type left facial palsy for 4 days. Diffusion-weighted (DWI) Magnetic Resonance Imaging of the Brain revealed an area of diffusion restriction involving anterior limb of internal capsule, head of caudate (Right>Left) and anterior thalamus suggestive of “Tubercular Zone” infarction (Figure 1).
Figure 1: (Right) MRI Brain DWI shows area of diffusion restriction involving anterior limb of internal capsule, head of caudate (Right>Left) and anterior thalamus.
Case 2
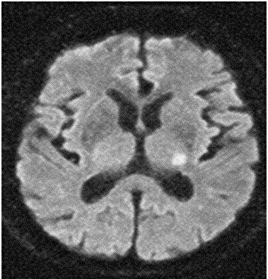
34-year-old male presented with fever and headache for 15 days followed by altered sensorium for 1 day. His Cerebrospinal fluid (CSF) TB Polymerase Chain Reaction (PCR) was positive with lymphocytic pleocytosis (Total cells 90; 85% lymphocytes) and raised proteins (134 mg/dL). MRI Brain DWI sequences revealed diffusion restriction in left posterolateral thalamus, suggesting “Ischemic Zone” infarction (Figure 2).
Figure 2: (Left) MRI Brain DWI shows area of diffusion restriction involving posterolateral thalamus.
Discussion
Classically described by Hsieh et al., infarctions in CNS TB follow two patterns: Tubercular Zone (supplied by medial lenticulostriate arteries) which consists of head of caudate, anterior limb and genu of the internal capsule and anteromedial thalamus and Ischemic Zone (supplied by lateral lenticulostriate arteries) which consists of the lentiform nucleus, posterior limb of internal capsule and posterolateral thalamus [2,3]. Infarcts in “Tubercular Zone” are more common as compared to the ischemic zone. The exact pathophysiology is not known but the most common hypothesis for development of these non-atherosclerotic infarcts is attributed to direct infection of the small vessels leading to infective vasculitis, inflammatory inflitrates and subsequent thrombosis in these areas [3,4].
Conclusion
Infarction patterns in patients with CNS TB may vary from small to large vessel infarction. One should look for “Tubercular Zone” infarctions especially while dealing with patients with CNS TB as these are of prognosntic value when considered with CSF and clinical picture.
References
- Zhang, L., Zhang, X., Li, H. et al. (2019). Acute ischemic stroke in young adults with tuberculous meningitis. BMC Infect Dis, 19:362.
Publisher | Google Scholor - Hsieh FY, Chia LG, Shen WC. (1992). Locations of cerebral infarctions in tuberculous meningitis. Neuroradiology, 34(3):197-199.
Publisher | Google Scholor - Soni N, Kumar S, Shimle A, Ora M, Bathla G, Mishra P. (2020). Cerebrovascular complications in tuberculous meningitis—A magnetic resonance imaging study in 90 patients from a tertiary care hospital. The Neuroradiology Journal, 33(1):3-16.
Publisher | Google Scholor - Naik, S., Bhoi, S. K., Deep, N., Mohakud, S., Mishra, B., Dey, A., Kumar, R., Saharia, G. K., & Kumar, M. (2022). Vascular manifestations of tuberculous meningitis: MR angiography and venography study. Journal of Neurosciences in Rural Practice, 13(529):529-536.
Publisher | Google Scholor